
Palpable Pulsatile Mass of the Forehead: A Case Series of Superficial Temporal Artery Pseudoaneurysms
*Corresponding Author(s):
Philippe De VleeschauwerDepartment Of Thoracic And Vascular Surgery, Heilig-Hart Ziekenhuis Lier, Mechelsestraat 24, 2500 Lier, Belgium
Tel:+32-3-4912866; +32-4-77610491,
Email:drpdv@icloud.com
Abstract
Background: Pseudoaneurysms of the Superficial Temporal Artery (STA) are rare and originate in most cases post-traumatically, often in young to middle-aged men. A palpable pulsatile mass at the temporal region is present, and pulsations can be eliminated or reduced by proximal compression of the STA. Diagnosis is often confirmed by duplex-sonography.
Methods: Between 2006 and 2016, five patients with a palpable pulsatile mass of the forehead presented at our institution. Case history, clinical, technical and histo-pathological patient data and corresponding treatment is presented and compared with current literature on pseudoaneurysms of the STA.
Results: In four cases the pulsatile mass was caused by a trauma, while in one case the mass arised spontaneously. Clinical examination revealed a palpable pulsatile mass on the forehead. The pulsatile quality of all tumors disappeared by unilateral compression of the STA. Duplex-sonography revealed a traumatic pseudoaneurysm in four cases and an Arteriovenous (AV) malformation in one case. A resection of the pseudoaneurysms and AV malformation was performed. Histo-pathological examination confirmed the clinical diagnosis.
Conclusion: Despite recent advances in endovascular approaches, surgical resection remains the treatment of choice. Our results are concordant with current literature regarding pseudoaneurysms of the STA.
Keywords
ABBREVIATIONS
STA - Superficial Temporal Artery
AV - Arteriovenous
APE – Anatomo pathological Examination
INTRODUCTION
Although lesions of the STA are rare, the STA is unprotected over a long distance. In most case reports the superficial anterior branch is affected. Between the occipitofrontalis muscle and the temporalis muscle, the anterior branch of the STA is most vulnerable to compression against the rigid scull [2,4] (Figure 1). Male and elderly patients with atherosclerotic and/or calcified arteries are especially vulnerable to this type of aneurysm. men are also more likely to be exposed to trauma [5].
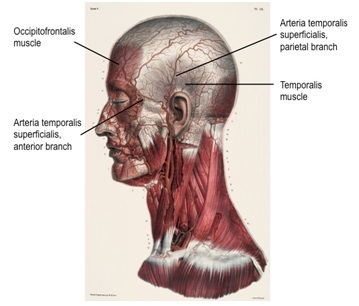 Figure 1: Anatomy of the ATS in relation to occipitofrontalis and temporalis muscle. Between the occipitofrontalis muscle and temporalis muscle the anterior branch of the STA is most vulnerable to compression against the rigid scull [1,4].
Figure 1: Anatomy of the ATS in relation to occipitofrontalis and temporalis muscle. Between the occipitofrontalis muscle and temporalis muscle the anterior branch of the STA is most vulnerable to compression against the rigid scull [1,4].Most aneurysms of the STA are pseudoaneurysms: a trauma to the STA leads to partial trans section and/or contusion of a segment of the artery and causes the lumen of the artery no longer being surrounded by the three layers of the arterial wall [2,4] (Figure 2). This is in contrast to a “real” aneurysm, where the three layers of the arterial wall remain present. Often young patients have a compressible pulsatile mass of 1-1, 5 cm approximately two to six weeks after traumatic injury of the temporal region. Additional symptoms can be throbbing headache, auditorial and visual disturbances, vertigo and rarely facial nerve paresis. The pulsations of the mass can be eliminated or reduced by proximal compression of the STA. A systolic murmur and a palpable ‘thrill’ can be present [2,4].
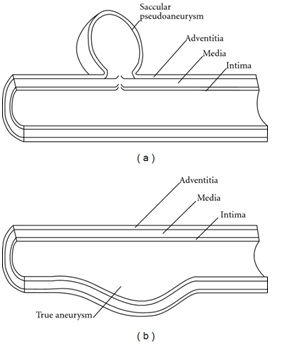 Figure 2: Schematic demonstration of anatomy of pseudoaneurysm (a) true aneurysm (b) In true aneurysm all layers of the vessel wall are involved [6].
Figure 2: Schematic demonstration of anatomy of pseudoaneurysm (a) true aneurysm (b) In true aneurysm all layers of the vessel wall are involved [6]. MATERIAL AND METHODS
RESULTS
| Case | Sex | Age (years) | Origin | Treatment | APE | Time to pseudoaneurysm after trauma |
| Case 1 | Male | 45 | Traumatic | Surgical resection | Pseudoaneurysm (Ø: 0.43 cm) | 4 weeks |
| Case 2 | Male | 18 | Traumatic | Surgical resection | Pseudoaneurysm (Ø: 1.10 cm) | 6 weeks |
| Case 3 | Male | 48 | Atraumatic | Surgical resection | AV malformation (Ø: 2.26 cm) | - |
| Case 4 | Female | 64 | Traumatic | Surgical resection | Pseudoaneurysm | 1 year |
| (Ø: 0.92 cm) | ||||||
| Case 5 | Male | 24 | Traumatic | Surgical resection | Pseudoaneurysm (Ø: 0.80 cm) | 2 weeks |
Case 1
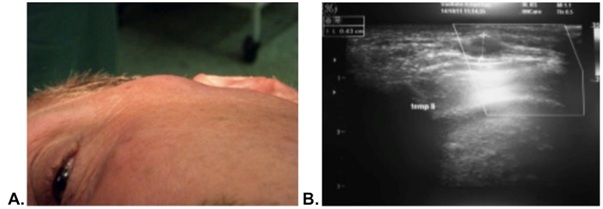 Figure 3: Pulsatile tumor at the left temporal region. B: Duplex-sonography of the STA pseudoaneurysm with a diameter of 0.43 cm.
Figure 3: Pulsatile tumor at the left temporal region. B: Duplex-sonography of the STA pseudoaneurysm with a diameter of 0.43 cm. The diagnosis of a posttraumatic pseudoaneurysm was histo pathologically confirmed. An arterial vessel with an aneurysmatic dilatation and a prominent intima was seen microscopically. In addition, regional fibrosis was observed already showing signs of organization. Within this fibrous plaque inflammatory cells, including mononuclear and eosinophilic cells, were found. Both the tunica elastica and media were fragmented. No smooth muscle fibers were found in the pseudoaneurysm. Histo-pathologically there were no arguments for arthritis.
The patient recovered uneventfully [8].
Case 2
Complete resection of the pulsatile protuberance with ligation of the proximal and distal STA was performed under local anesthesia.
The diagnosis of a post traumatically pseudoaneurysm of 1.10 cm was histo pathologically confirmed.
Case 3
Duplex-sonography showed a very high systolic and diastolic flow of the left STA compared to the right STA. Angio-MRI confirmed a subcutaneous Ateriovenous (AV) malformation at the left frontoparietal region with a maximal diameter of 2.26 cm. The AV malformation showed a slightly hypertrophic and tortuous parietal branch of the left STA (Figure 4). There was no connection with the intracranial circulation.
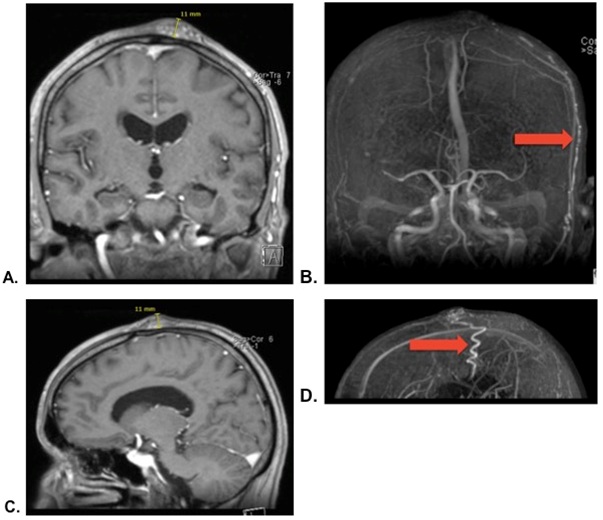 Figure 4A: AV malformation on Angio-MRI (coronal plane). B: AV malformation on Angio-MRI (coronal plane) with a slightly hypertrophic and tortuous left STA (red arrow). C: AV malformation on Angio-MRI (sagittal plane). D: AV malformation on Angio-MRI (sagittal plane) with a slightly hypertrophic and tortuous left STA (red arrow).
Figure 4A: AV malformation on Angio-MRI (coronal plane). B: AV malformation on Angio-MRI (coronal plane) with a slightly hypertrophic and tortuous left STA (red arrow). C: AV malformation on Angio-MRI (sagittal plane). D: AV malformation on Angio-MRI (sagittal plane) with a slightly hypertrophic and tortuous left STA (red arrow).The afferent left STA proximal to the AV malformation was ligated under general anesthesia. Subsequently the AV malformation was completely resected. The diagnosis of an AV malformation was confirmed histo pathologically. Recovery was uneven full.
Case 4
Case 5
Histopathological diagnosis of a posttraumatic pseudoaneurysm of 0.80 cm was confirmed. The tunica media and lamina elastic interna of the tunica intima suddenly disappeared. In other words, a fragmentation and loss of these inner layers was present, concordant with a pseudoaneurysm. The remaining lumen of the arterial vessel consisted of adventitia filled with thrombus (Figure 5).
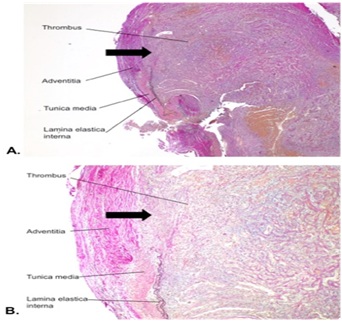 Figure 5A: Transverse section of the pseudoaneurysm (4x magnification). B: Transverse section of the pseudoaneurysm (10x magnification). Black arrow: fragmentation and loss of the tunica media and lamina elastic interna of the tunica intima. The lumen of the pseudoaneurysm consisted of adventitia filled with thrombus.
Figure 5A: Transverse section of the pseudoaneurysm (4x magnification). B: Transverse section of the pseudoaneurysm (10x magnification). Black arrow: fragmentation and loss of the tunica media and lamina elastic interna of the tunica intima. The lumen of the pseudoaneurysm consisted of adventitia filled with thrombus.DISCUSSION
Nonsurgical methods include observation and application of continuous pressure over the aneurysm with eventual thrombosis. These methods can be effective in cases of small STA pseudoaneurysms, sometimes associated with arteriovenous fistulas [1,5]. Others suggest that conservative treatment is not appropriate due to the risk of rupture, bleeding and thrombo embolism [5,11].
Nowadays endovasculair approaches for treatment of vascular malformations gain popularity. Endovascular treatment using a microcoil or vascular plug may be used as a therapeutic tool when the STA pseudoaneurysm has a relatively inaccessible localization, such as the proximal STA [1]. In these cases, adequate dissection of the parotid gland and the facial nerve before ligation and resection of the aneurysm may pose a greater threat than the aneurysm itself; justifying endovascular embolization as the first choice of treatment [1]. Compared to surgical resection, coil embolization requires a longer preoperative time but has a shorter recovery time and avoids/minimizes the surgical scar [1, 9].Nikolakopoulos et al., suggest that an endovascular approach should only be performed when angiography is mandatory for diagnosis [5].
Furthermore, percutaneous ultrasound-guided injection of thrombin can be used on chronic or sub acute pseudoaneurysms with a diameter of 4 cm or less [5]. In contrast to coil-embolisation, local injection of thrombine has a higher incidence of complications such as allergic reactions, risk for recanalisation and distal ischemia [5,9]. Other disadvantages are the lag time for resolution of the thrombosed pseudoaneurysm and the need for reexamination with duplex ultrasound to ensure no recanalization of the pseudoaneurysm has occurred [5].
The diagnosis is confirmed histo pathologically with loss of normal arterial architecture and an arterial wall that mainly consists of fibrous tissue and organized thrombus.
CONCLUSION
STA pseudoaneurysms are rare and develop in most cases post traumatically. Despite recent advances in endovascular approaches, surgical resection remains the treatment of choice.
FUNDING
REFERENCES
- Cvetic VZ, Radmili O, Lukic B, Colic M, Davidovic L (2016) Endovascular Treatment of Traumatic Pseudoaneurysm of the Superficial Temporal Artery. Vasc Endovasc Surg 50:171-174.
- Marovic P, Manohar P, Tsan C (2011) Traumatic pseudoaneurysm of the superficial temporal artery. ANZ J Surg 81: 88-89.
- Younus SM, Imran M, Qazi R (2015) Superficial Temporal Artery Pseudoaneurysm: A Case Report. Front Surg 2: 51.
- Evans CC, Larson MJ, Eichhorn PJ, Taylor RS (2003)Traumatic pseudoaneurysm of the superficial temporal artery: two cases and review of the literature. J Am AcadDermatol 49: 286-288.
- Nikolakopoulos KM, Papageorgopoulou CP, Ntouvas IG, Kakkos S, Tsolakis I (2016) Palpable Mass on the Head after Minor Trauma. Case Rep Vasc Med 2016: 1340589.
- Owlia MB, Mehrpoor G (2012) Behcet's Disease: New Concepts in Cardiovascular Involvements and Future Direction for Treatment. ISRN Pharmacol 2012: 760484.
- Wei W, Akkersdijk GP (2011) Spontaneous aneurysm of the superficial temporal artery. Lancet 378: 168.
- Goossens K, De Vleeschauwer P (2012) Een 45-jarige patiënt met een traumatisch pseudoaneurysma van de arteria temporalis superficialis. Tijdschr voor Geneeskunde 19: 951-953
- Hong JT, Lee SW, Ihn YK, Son BC, Sung JH, et al. (2006) Traumatic pseudoaneurysm of the superficial temporal artery treated by endovascular coil embolization. Surg Neurol 66: 86-88.
- Mizouni H, Hedhli M, Zainine R, Sahtout S, Besbes G, et al. (2011) Post-traumatic pseudoaneurysm of the superficial temporal artery: a rare cause of facial mass. Eur J Radiol Extra 79: 33-35.
- Czihal M, Sturm A, Hoffmann U, Kuhlencordt PJ (2015) Painful nodule of the forehead after blunt trauma: superficial temporal artery pseudoaneurysm. Vasc Med 20: 86-87.
Citation: Domen A, De Vleeschauwer P, Goossens K, Deruyver Y (2017) Palpable Pulsatile Mass of the Forehead: A Case Series of Superficial Temporal Artery Pseudoaneurysms. J Angiol Vasc Surg 2: 010.
Copyright: © 2017 Andreas Domen, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

