
A Case of Nodular Oncocytic Hyperplasia vs. Reactive Lymphadenopathy
*Corresponding Author(s):
Tejas RavalDepartment Of Otolaryngology Head And Neck Surgery, Southside Regional ENT Specialist, United States
Tel:+1 8047655320,
Email:thraval@gmail.com
CASE PRESENTATION
We report a case of Nodular Oncolytic Hyperplasia. What is unique about this case is the presenting symptoms. The patient noted that her cervical nodules were responsive to antibiotics leading us to believe a diagnosis of reactive lymphadenopathy. After full work up and excisional biopsy, the patient was diagnosed with Nodular Oncoyctic Hyperplasia.
An 80-year-old female with history of hypertension and seizure disorder presented for evaluation of a 2-month history of left sided neck mass. The mass was painless in nature and located in the left parotid tail and upper cervical region. Patient had been treated with ciprofloxacin for urinary tract infection by her primary care physician, which per patient report, seemed to decrease the size of the left sided neck swelling. Patient was otherwise asymptomatic without hoarseness, dysphagia, or constitutional symptoms. Physical examination demonstrated at least two adjacent nodular lesions in the junction of the parotid tail and upper neck. Masses were firm but mobile, and slightly tender. Remainder of the head and neck exam is unremarkable, and facial nerve is intact. Due to her previous response to antibiotics, the patient was started on a 10 day course of amoxicillin with minimal improvement. Computed tomography scan of the neck with intravenous contrast revealed multiple prominent enhancing masses within the left parotid gland, with the largest measuring 1.8 cm, and in a lesser degree within the right parotid gland, thought to be lymph nodes. Fine needle aspiration of the most prominent left-sided mass revealed normal salivary gland cells. Open excisional biopsy was recommended and performed. Intraoperatively, a 1.5 cm nodular mass was found adjacent to the parotid tail. With further intraoperative exploration and berry picking, additional adjacent nodules were found and excised with the main specimen. Dissection spared the cervical and marginal mandibular branches of the facial nerve. Surgical specimen consisted of multi-lobated maroon brown, firm tissue. Microscopic exam revealed well circumscribed proliferation of oncocytes with dense bright eosinophilic cytoplasm and monomorphic nuclei, without a well-defined fibrous capsule (Figures 1 and 2). Surgery went without complication, post-operative House-Brackmann score of 1/6. Patient is being followed with serial physical examinations.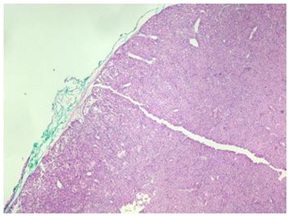 Figure 1: Histopathologic evaluation of gross specimen.
Figure 1: Histopathologic evaluation of gross specimen.
This figure is highlighting how the specimen does not have a well-formed capsule. This is a differentiating factor of nodular oncocytic hyperplasia compared to other similar tumors such as Warthins Tumor.
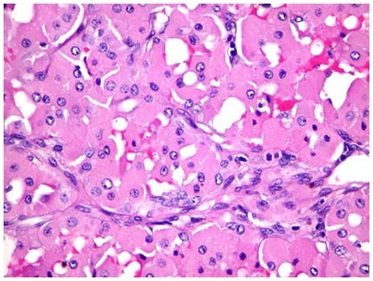 Figure 2: Characteristic oncocytes of Nodular Oncocytic Hyperplasia.
Figure 2: Characteristic oncocytes of Nodular Oncocytic Hyperplasia.
This slice show the characteristic cells that aid in the diagnosis of Nodular oncocytic hyperplasia. Note the oncocytic, bright eosinophilic, cells packed with mitochondria.
DISCUSSION
Nodular Oncocytic Hyperplasia (NOH) is a rare, non-neoplastic growth of the parotid gland. It is a type of oncolytic lesion caused by proliferation of the duct system [1]. The World Health Organization (WHO) classification describes three main types of oncocytic lesions: diffuse oncocytosis, focal nodular/adenomatous oncocytic hyperplasia, and oncocytoma [2]. To diagnose NOH, careful cytologic and histologic evaluation must be performed to differentiate NOH from the other oncocytic lesions and oncocytic-like lesions. Cytology alone has not been found to be sufficient for diagnosis due to the overlap between the oncocytic lesions.
Oncocytes are epithelial cells with abundant, granular, eosinophilic cytoplasm due to presence of numerous large mitochondria of varied sizes [3]. In the head and neck, only a small number of lesions are constructed of oncocytes. However, the head and neck are among the more common sites for the development of true oncocytic neoplasms because oncocytes are normally scattered within major and minor salivary gland tissue [4]. Other locations oncocytic tumors can be found include the kidney,breasts, thyroid glands, upper respiratory tract and lacrimal glands [4]. The quantity of oncocytes, and architectural pattern are a few of the main factors in differentiating the types of oncocytic lesions. Nodular Oncocytic Hyperplasia notably has remnants of the original salivary tissue with acini and fatty tissue present between the oncocytic nodules [1]. Cytological evaluation shows loose sheet-like cluster of round to polygonal cells with granular cytoplasm against a hemorrhagic background [5].
Histologically, NOH is formed by many variable-sized nodules, comprising oncocyte-like cells with small round nuclei and eosinophilic granular cytoplasm, without fibrous capsule, that is positive for mitochondrial antibodies [4,5]. The parenchyma of the parotid gland, including serous acini, ducts, and adipose tissue, is interspersed among the nodules [4]. NOH compared to diffuse hyperplastic oncocytosis or oncocytoma, has multiple condensed areas of oncocytes and is not surrounded by a fibrous capsule.
The criteria for oncocytoma include the following:
• It is a nodule composed entirely of oncocytic cells
• It has a solid trabecular/acinar growth pattern without prominent peripheral palisading of the tumor cells
• It has a fibrous capsule, not necessarily complete
• There is little internal fibrous stroma
• There are no included ducts
• It is usually a solitary tumor [4]
One of the main differentiating factors between oncocytoma and NOH is the presence of a fibrous capsule. NOH does not have any fibrous capsule while oncocytoma does. When considering a unilateral oncocytic parotid lesion, one must rule out the more common Warthin Tumor. Warthin tumor is the most common oncocytic tumor of the head and neck [6]. Compared to NOH, it affects men slightly more than women and peaks in the fifth to seventh decades of life, while NOH affects women slightly more than men and peaks in the 6th decade of life [5]. A main distinguishing factor for diagnosing Warthin tumor is the presences of mast cells, small lymphocytes and plasma cells.However, if only the oncocyte portion of Warthin tumor is aspirated during cell collection, then it is not distinguishable from oncocytoma or oncocytosis/NOH [6]. Oncocytoma also has few or absent lymphocytes, absent dendritic-lymphocytic aggregates and rare cystic changes compared to Warthin Tumor [6]. Also, the presence of paucicellular specimen comprised of small groups of oncocytic cells should raise the possibility of oncocytosis/NOH in the differential diagnosis and can favor it in elderly patients with multiple salivary nodules [7]. This shows that cytology alone is non-diagnostic and a full histologic evaluation is needed when considering oncocytic salivary gland lesions.
Based on the demographics of the patient, cytologic and histologic evaluation, our patient was diagnosed with NOH. Complete work-up is paramount as this patient presented with an infectious like etiology rather than salivary gland neoplasm. Evaluation including imaging studies, FNA cytology and histology must be performed to accurately diagnose this particular parotid gland lesion. The best treatment for NOH is complete surgical excision of the lesion [4]. Most cases do not require further evaluation or monitoring as NOH is a benign tumor and recurrence is rare.
This article was exempt from institutional review board or ethics committee review.
REFERENCES
- Kontaxis A, Zanarotti U, Kainz J, Beham A (2004) Diffuse hyperplastic oncocytosis of the parotid gland. Laryngorhinootologie 83: 185-188.
- Bonfils P, de Preobrajenski N, Miranda L, Halimi P, Bigorgne C, et al. (2007) Multifocal Nodular Oncocytosis Hyperplasia of the Parotid Gland. Ann Otolaryngol Chir Cervicofac 124: 76-79.
- Tung B-K, Li W-Y, Chu P-Y (2012) Pathology Quiz Case 2. Arch Otolaryngol Head Neck Surg 138: 523.
- Kinoshita Y, Harada H, Kobayashi TK, Yoshizawa K, Yuri T, et al. (2014) Multifocal Adenomatous Oncocytic Hyperplasia of the Parotid Gland. Case Rep Oncol 7: 819-824.
- Chakrabarti I, Basu A, Ghosh N (2012) Oncocytic lesion of parotid gland: A dilemma for cytopathologists. J Cytol 29: 80-82.
- Wakely PE (2008) Oncocytic and oncocyte-like lesions of the head and neck. Ann Diagn Pathol 12: 222-230.
- Rooper LM, Onenerk M, Siddiqui MT, Faquin WC, Bishop JA, et al. (2017) Nodular oncocytic hyperplasia: Can cytomorphology allow for the preoperative diagnosis of a nonneoplastic salivary disease? Cancer Cytopathol 125: 627-634.
Citation: Bayne K, Raval T (2019) A Case of Nodular Oncocytic Hyperplasia vs. Reactive Lymphadenopathy. J Clin Stud Med Case Rep 6: 065.
Copyright: © 2019 Kilee Bayne, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

