Redesigning the Surgical Schedule to Enhance Productivity in the Operating Room
*Corresponding Author(s):
Rathlev NKDepartment Of Emergency Medicine, Baystate Medical Center, University Of Massachusetts Medical School-Baystate, Massachusetts, United States
Tel:+1 4137945375,
Fax:+1 4139088070
Email:Niels.Rathlev@baystatehealth.org
Abstract
Background: Since elective surgical cases are often scheduled in “batches,” peaks and valleys in demand for operating room and postoperative care are created. We examined the effects of “smoothing” the elective surgical schedule, separating elective from urgent and emergency cases and eliminating block scheduling. We sought to decrease the 1) demand for inpatient postoperative care, 2) number of postponed or canceled operating room cases, 3) direct nursing hours on post-surgical floors and 4) Emergency Department (ED) length of stay for admitted patients.
Methods: The division of vascular surgery limited to two per day, the number of elective surgical cases destined postoperatively for an inpatient bed. A similar plan was developed for the department of cardiothoracic surgery. The use of in-patient beds for elective surgical cases was measured by day of the week. Concurrently, we separated elective from urgent and emergency cases and eliminated block scheduling. Direct nursing hours were measured on floors that cared for post-operative patients and the time from ED decision to admit to departure to an inpatient floor were measured.
Results: After the changes, the number of direct nursing hours decreased 5.7% from 8.66 hours per patient day to 8.16. This resulted in projected annualized savings of $130,000. The number of postponed or canceled surgeries decreased from 334 to 3 (99.1 percent reduction) during identical six-month periods year-over-year. The time from ED decision to admit to departure for the inpatient floor for all adult admissions decreased by a mean of 30 minutes (18.5%) per patient from 162 to 132 minutes.
Conclusion: Redesign of the operating room resulted in a 99.5% reduction in the number of postponed and canceled cases. It was associated with reductions in direct nursing hours (5.7%), overtime pay on nursing floors and ED time from decision to admit to departure for admitted patients (18.5%).
Keywords
INTRODUCTION
The inpatient function of the hospital is a set of interdependent systems that have a primary goal of providing the highest quality of care to as many patients as possible. The management team must continuously study and root out constraints in these systems to reach the primary goal [1]. Boston Medical Center is a 624 bed, non-profit, Level 1 Trauma Center teaching hospital with an annual Emergency Department (ED) volume of 124, 447 [2]. We developed an analytical approach to re-engineering the flow of patients through our institution and used data to guide our problem-solving. Key interdependent systems included patient arrival, ED throughput, bed assignment for admissions, discharge, patient departure and bed cleaning, and scheduling of elective surgical cases.
We empowered the stakeholders to create change to reduce inefficiency. By working with surgeons, we redesigned the elective surgery schedule to open slots in operating rooms when the ED predictably was busier. The elective vascular surgery schedule was heavily concentrated in the beginning of the week. This created bottlenecks on those days, while Fridays and weekends were affected much less. Moreover, our goal was to separate elective from urgent/emergency surgical cases in order to decrease the high number of canceled and postponed cases. Finally, we wanted to eliminate block scheduling in the operating rooms in order to minimize unused and idle operation room time [3].
In conjunction with the paradigm changes in the operating room, changes were measured in the length of stay for all ED patients that were admitted. When there are no available beds in a hospital, patients who have been admitted remain or “board” in the ED until an appropriate bed can be assigned. As a result, demand for emergency services eventually exceeds capacity when no available beds remain. Ambulances may finally be diverted to other institutions to alleviate crowding in the ED. Rather than accepting this as inevitable; the causes of ED length of stay were examined in the belief that the variability in operating room scheduling had a significant impact [4].
METHODS
The chairs of surgery, anesthesiology and cardiothoracic surgery led the process of implementing the initiative to smooth the elective surgery schedule. This was done in conjunction with the Chief Medical Officer (JC), Director of the Operating Room and a consultant from the Boston University School of Management (EL). Ultimately, the goal was to enhance efficiency and increase the overall surgical volume. Elective vascular cases were initially targeted and the baseline distribution of the number of patients requiring inpatient postoperative care by day of the week was calculated for one month. Based on institutional experience, two cases per day for five weekdays exceeded the number that the vascular surgeons typically performed in a week on patients that required post-surgical inpatient care. The number of direct nursing hours per day was measured on one of the postoperative floors that specialized in vascular cases; it was anticipated that a more balanced flow of patients would create a more predictable demand in nursing staffing.
Instead of enforcing a daily limit on the cardiothoracic surgery service, the vice-chair changed his clinic day from Friday to Wednesday, so that he could schedule operating room cases on Fridays. This effectively “smoothed” the schedule for cardiothoracic surgery. Since both vascular and cardiothoracic surgery preferentially admitted postoperative patients to the Progressive Care Unit (PCU) - a step-down unit from the Surgical Intensive Care Unit (SICU) - the census on this unit was measured before and after the changes in scheduling had been completed. Changes in PCU census were considered representative of the experience on other units.
A plan was created to reduce the number of re-scheduled cases by separating elective from urgent/emergency cases. Reliable priority data for emergency operating room capability was collected to determine the required hours of availability and the number of rooms. The operating room performed between 25 and 32 cases per day in eight rooms. These included pediatric, obstetrics and gynecology and trauma cases. On a regular basis, 33% or 5-12 patients per day were “add-ons” that would frequently delay elective cases. The delays resulted in an unacceptable 20% annual cancellation rate; many cases were never re-scheduled and presumably “lost” to other institutions. Off hours were not issues with respect to cancellations or significant delays. We therefore determined that one operating room suite, available Monday through Friday 7AM to 3:30PM, was sufficient to ensure that elective cases would rarely be canceled. This emergency operating room was fully staffed and ready to go during these hours and the suite was open to all surgeons. Cases were classified and prioritized as follows: 1) emergency cases required the operating room within 30 minutes; 2) urgent cases needed surgery within 30 minutes to 4 hours and 3) semi-urgent cases within 4 to 24 hours.
Finally, block scheduling, i.e, the practice of reserving operating room time and day of the week for a specific surgeon or service, was eliminated. Surgeons were promised that “no case would be refused,” and that consecutive cases could be booked as a group. It was emphasized that the over-arching goal was to increase overall surgical volume. Ideally, utilization of every block would approach 100%. However, utilization of the block schedule was approximately 50% due to variability in surgeon’s vacations, professional meetings, time off etc. Moreover, the block schedule required frequent revisions as surgeons turned over and demand changed. At the same time, surgeons lived in fear of losing their block time. Most cases were booked only three to four days in advance and surgical services used release time in variable fashion. The fears of open or no-block scheduling included expectations that some would “game the system “creating competition for the same time slots. Other concerns included that surgeons might be disadvantaged when booking cases late and therefore lose operating room time and income, and, that the schedule would be disorganized. Open block scheduling gave surgeons flexibility, equal access and promoted booking far in advance. Moreover, it made time in the operating room available for other surgeons during vacations and time away.
RESULTS
Figure 1 depicts the demand for beds for elective vascular cases on two postoperative floors (7 West and 8 West), the PCU and the SICU prior to changes in the operating room schedule. By far, the greatest demand occurred midweek on Tuesdays, Wednesdays and Thursdays. Figure 2 demonstrates the baseline distribution of elective vascular cases that required PCU care by day of the week; the demand varied from zero to four cases per day. The data for elective cardiothoracic surgery cases requiring inpatient beds showed a similar distribution by day of the week for patients destined for the SICU but not the step-down PCU (Figure 3). Conversely, the distribution of unscheduled (including emergency) cardiothoracic surgical procedures varied little by day of the week (Figure 4).
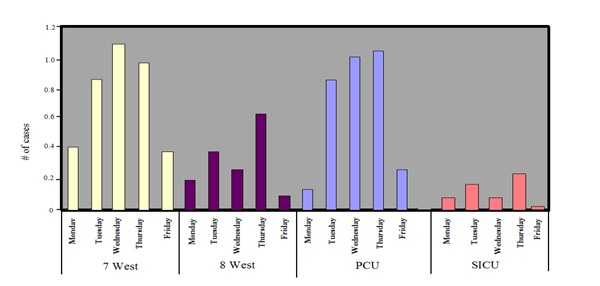 Figure 1: Elective vascular surgery cases: Inpatient bed demand by day of the week for floor (7 West and 8 West), Progressive Care Unit (PCU) and Surgical Intensive Care Unit (SICU) beds.
Figure 1: Elective vascular surgery cases: Inpatient bed demand by day of the week for floor (7 West and 8 West), Progressive Care Unit (PCU) and Surgical Intensive Care Unit (SICU) beds.
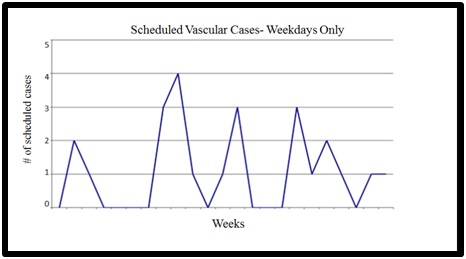 Figure 2: Baseline distribution by day of the week of scheduled vascular cases admitted to the Progressive Care Unit (PCU): demand varied from zero to 4 cases per day.
Figure 2: Baseline distribution by day of the week of scheduled vascular cases admitted to the Progressive Care Unit (PCU): demand varied from zero to 4 cases per day.
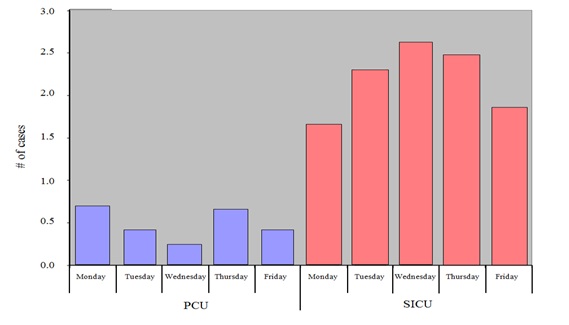 Figure 3: Elective scheduled cardiothoracic surgery cases: Inpatient bed demand by day of the week in the Progressive Care Unit (PCU) and Surgical Intensive Care Unit (SICU).
Figure 3: Elective scheduled cardiothoracic surgery cases: Inpatient bed demand by day of the week in the Progressive Care Unit (PCU) and Surgical Intensive Care Unit (SICU).
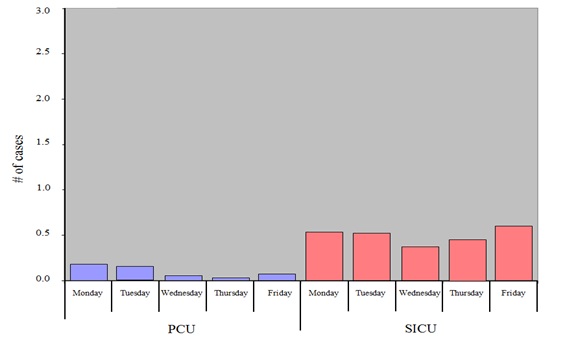 Figure 4: Unscheduled and emergency cardiothoracic surgery cases: Inpatient bed demand by day of the week in the Progressive Care Unit (PCU) and Surgical Intensive Care Unit (SICU).
Figure 4: Unscheduled and emergency cardiothoracic surgery cases: Inpatient bed demand by day of the week in the Progressive Care Unit (PCU) and Surgical Intensive Care Unit (SICU).
A rapid cycle test was conducted for one month that revealed the feasibility and benefit of limiting the vascular surgery service to two elective operating room cases per day. Because of the limit on daily surgeries, the weekly schedule became more evenly distributed from Monday through Friday (Figure 5). The daily PCU census showed significant “smoothing” of the peaks and valleys in demand when the data from the year before (blue line) and the year after (red line) are compared in (Figure 6). The range was a census from one to 10 cases, whereas the range was two to seven cases a year later. This represents a 55% reduction in variability year over year. The number of direct nursing hours in the PCU decreased by 5.8% from 8.66 hours per patient day to 8.16 after smoothing the surgical schedule for vascular and cardiothoracic surgery (Figure 7). The result was a more predictable demand for nursing staffing, fewer overtime payments, and ultimately, and annualized savings of approximately $130,000.
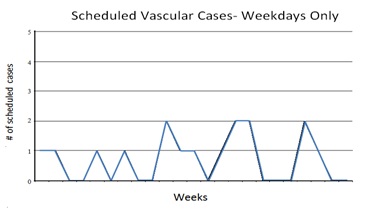 Figure 5: Distribution by day of the week of elective vascular cases admitted to the Progressive Care Unit (PCU) after imposing a maximum limit of 2 per day.
Figure 5: Distribution by day of the week of elective vascular cases admitted to the Progressive Care Unit (PCU) after imposing a maximum limit of 2 per day.

Figure 6: Daily Progressive Care Unit (PCU) census 2003 vs. 2004.
 Figure 7: Direct nursing hours per patient day defined as hours spent in direct patient care in the Progressive Care Unit (PCU): 8.66 prior to vascular and cardiothoracic surgical smoothing versus 8.16 after smoothing; this represents a 5.8% decrease.
Figure 7: Direct nursing hours per patient day defined as hours spent in direct patient care in the Progressive Care Unit (PCU): 8.66 prior to vascular and cardiothoracic surgical smoothing versus 8.16 after smoothing; this represents a 5.8% decrease.
In the 12-month period (April 1, 2003 to March 31, 2004) before the separation of urgent and emergency from elective cases, a total of 6,608 cases were scheduled and 349 emergency cases were performed Mondays through Fridays from 7AM to 3:30PM; however, 771(11.6%) elective patients were either delayed or canceled. The annual volumes of scheduled and emergency (354) cases were essentially unchanged in the following year (April 1, 2004 to March 31, 2005) after separation of urgent/emergency from elective cases. Importantly, only seven elective patients were canceled. This represents a 99% reduction in canceled or delayed cases.
At baseline, the ED length of stay for all patients exhibited no clear upward or downward trend (Figure 8). After the changes in operating room scheduling had been implemented, the amount of time admitted ED patients “boarded” i.e., waited for an inpatient bed after the admission decision had been made, decreased from 162 to 132 minutes. This represents a 30-minute (18.5%) improvement in “boarding” time from disposition decision to actual departure for admitted ED patients (Figure 9).
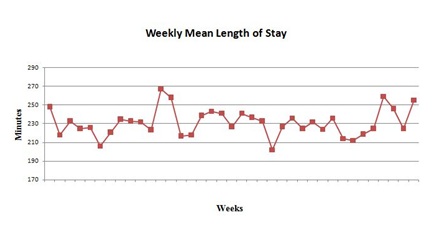
Figure 8: Baseline ED length of stay in minutes for all patients.
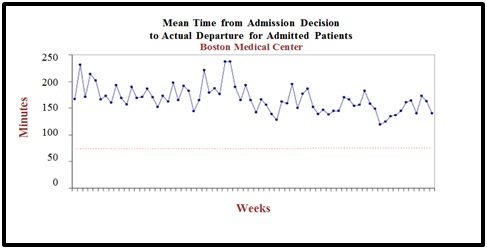
Figure 9: Mean time from admission decision to actual departure from the emergency department for admitted patients during changes in operating room scheduling: decrease of 30 minutes from 162 minutes to 132 minutes or a 18.5% reduction.
DISCUSSION
By definition, “natural” variability in a system cannot be controlled and must simply be managed. The demand for non-elective in-hospital and ED care typically exhibits “natural” variability and does not vary greatly by day of the week. Examples are including the number of patients presenting to the ED for acute care and the types and number of emergency surgical cases that present. In contrast, “artificial” variability can be controlled and is exemplified by the planned scheduling of the types and numbers of elective interventions and testing [5]. According to the theory of “smoothing “artificial variability, a hospital needs to control and balance, variables that affect bed availability [6]. Elective surgical procedures are, to a substantial degree, subject to “artificial” variability since scheduling is largely created based on factors that are not related to patient flow and efficiency; physician schedules are a prominent example.
Much artificial variability remains in healthcare and we must eliminate it [7]. The science is the easy part; changing the culture to one that embraces and leads to improvement is the difficult part. Hard work and good intentions are necessary, but not sufficient, to deliver exceptional results [8]. According to Kotter, there are eight stages that leaders must follow in the process of creating major change: 1) establish a sense of urgency, 2) create a guiding coalition and leadership team, 3) develop a vision and strategy, 4) communicate and enroll people in the change visions, 5) empower broad-based action, 6) generate short-term wins, 7) consolidate gains and produce more change and 8) anchor new approaches in the culture [9]. The act of enrolling others in the initiative and getting their “buy-in” is critical. Collaborators must understand what is to be accomplished and why. However, many change efforts fail because individuals are simply told “what to do” without soliciting their feedback [10]. Instead, their concerns should be listened to and they must be given time to ask questions. Finally, potential collaborators must understand that their concerns have been heard and appropriately vetted before their commitment to create change is requested.
Hospital-wide solutions to inpatient and emergency department crowding were explored at Boston Medical Center. Current knowledge was applied to problem-solving and an analytical approach was applied to re-engineering flow. Using principles of rapid cycle change, successful changes should be fine-tuned and implemented [11]. If they are not successful during a brief cycle, the idea must be reconsidered. “Smoothing” the elective surgical schedule was a challenge because surgeons were asked to change their work schedules according to the new operating schedule; meetings were held with the vascular surgeons to discuss the concepts and the fact that they could schedule more surgeries over the course of the week (a total of 10 rather than the typical seven or eight) by agreeing to perform a maximum of two elective cases per day. To encourage acceptance of this new paradigm, vascular surgeons were assured that they would be able to perform all elective cases in a timely fashion and that no case would be refused. Instead of creating a limit per day, the chief of cardiothoracic surgery proposed a different solution by moving his operating day to effectively produce the same result and “smooth” the elective schedule.
Acknowledging that every system is perfectly designed to obtain exactly the results that are gets, a paradigm change was instituted in the operating room to enhance productivity and reduce the number of canceled and postponed cases [8]. Following the “Theory of Constraints”, management science was used to determine the true constraints [12]. Once the principal constraint was found, the goal was to solve it, before moving on to what is now the true constraint. To accomplish this in the operating room, data on utilization was needed so that bottle necks could be identified, and improvements could be made. Accordingly, the number of operating rooms and the hours of the day that needed to be available to accommodate urgent and emergency cases were determined. The change in separating these from elective cases clearly resulted in more productive use of operating room time with fewer gaps. Similar benefits have been demonstrated with this paradigm in a pediatric population at Cincinnati Children’s Medical Center [13]. Separating the flows of cases provided more choices in both day and time and surgeries were scheduled faster. With open block scheduling, surgeons did not need to notify the scheduling team of planned time off and a minimal number of complaints were ultimately filed.
Patients undergoing urgent and emergent surgical procedures are at risk for adverse outcomes [14]. Delays further increase the risk to patients due to increased morbidity and mortality. As a case in point, delayed non-cardiac surgery cases in Ottawa, Canada experienced statistically significant increases in mortality (OR 1.59), length-of-stay (OR 1.07) and total costs (OR 1.07) versus those without delay [15]. Previous literature has demonstrated that each additional elective surgical case can prolong the mean length of stay per ED patient because of competition with ED admissions for in-patient beds [2]. While other interventions in the ED were instituted concomitantly, the changes in operating room scheduling were considered to be powerful in terms of reducing ED cycle times and reducing “boarding”.
CONCLUSION
There is much artificial variability in healthcare and we can no longer afford this waste. Batching does not make sense if your goal is to minimize each individual input cost. We must change our systems to maximize flow which will improve safety, staff and patient satisfaction and waste. All hospitals should map flow on in-and outpatient units and operating rooms, and test changes to improve. Redesign in the operating room reduced waste and rework by “smoothing” the elective surgical schedule, separating elective from urgent/emergency cases and creating open block scheduling. It resulted in a 99% reduction the number of postponed and canceled cases. The paradigm changes were associated with reductions in direct nursing hours (5.7%), overtime pay on nursing floors that cared for patients postoperatively and the total length of stay for patients admitted from the ED (18.5%).
CONFLICTS OF INTEREST
None reported.
REFERENCES
- Goldratt EM, Cox J (1986) The goal: a process of ongoing improvement. Routledge, Abingdon, UK.
- Boston Medical Center (2004) Annual report 2004. Boston Medical Center, Boston, Massachusetts, USA.
- Levine WC, Dunn PF (2015) Optimizing operating room scheduling. Anesthesiol Clin 33: 697-711.
- Rathlev NK, Chessare J, Olshaker J, Obendorfer D, Mehta SD, et al. (2007) Time series analysis of variables associated with daily mean emergency department length of stay. Ann Emerg Med 49: 265-271.
- Wickramasinghe N, Geisler E (2008) Encyclopedia of Healthcare Information Systems. Medical Information Science Reference, USA.
- Litvak E, Buerhaus PI, Davidoff F, Long MC, McManus ML, et al. (2005) Managing unnecessary variability in patient demand to reduce nursing stress and improve patient safety. Jt Comm J Qual Patient Saf 31: 330-338.
- http://www.ihoptimize.org/what-we-do-methodology-artificial-variability-patient.htm
- Stroh DP (2018) Exposing the hidden benefits of business as usual: Why the status quo is so difficult to change. The System Thinker, USA.
- Kotter JP (1996) Leading Change. Harvard Business Review Press, Brighton, Massachusetts, USA.
- Langley GL, Moen RD, Nolan KM, Nolan TW, Norman CL, et al. (2009) The Improvement Guide: A practical approach to enhancing organizational performance (2ndedn). Jossey-Bass, San Francisco, CA, USA.
- Deming WE (2000) The New Economics: For Industry, Government, Education. MIT Press, Cambridge, Massachusetts, USA.
- Goldratt EM, Cox J (2004) The Goal: A Process of Ongoing Improvement (3rdedn). Routledge, Abingdon, UK.
- Litvak E (2010) Managing Patient Flow in Hospitals: Strategies and Solutions (2ndedn). Joint Commission Resources, Illinois, USA.
- Haider AH, Obirieze A, Velopulos CG, Richard P, Latif A, et al. (2015) Incremental cost of emergency versus elective surgery. Ann Surg 262: 260-266.
- McIsaac DI, Abdulla K, Yang H, Sundaresan S, Doering P, et al. (2017) Association of delay of urgent or emergency surgery with mortality and use of health care resources: a propensity score-matched observational cohort study. CMAJ 189: 905-912.
Citation: Rathlev NK, Chessare J, Litvak E (2018) Redesigning the Surgical Schedule to Enhance Productivity in the Operating Room. J Emerg Med Trauma Surg Care 5: 023.
Copyright: © 2018 Rathlev NK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.