ABSTRACT
The inflammatory bowel disease is a highly prevalent disorder in Spain. Incident cases have been increasing during the last decades. In this study we sought to determine rates and temporal patterns of hospitalizations related both to ulcerative colitis and Crohn’s disease in a 16-year period in Spain. All hospital discharges related to ulcerative colitis and Crohn’s disease among general population reported to the national information system for hospital data during a 16-year period (January 1, 1997 through December 31, 2012) were obtained. Most frequent co-morbidities, diagnostic procedures and surgeries were also reported. A total of 26,948 hospital discharges due to ulcerative colitis and 87,752 due to Crohn’s disease were reported in the 16 years study period in Spain. Mean age was 45.3 (SD = 20.5) and 38.0 (SD = 17.3) years, respectively. There were a total of 392 deaths among ulcerative colitis hospitalized patients and 565 among Crohn’s disease patients.
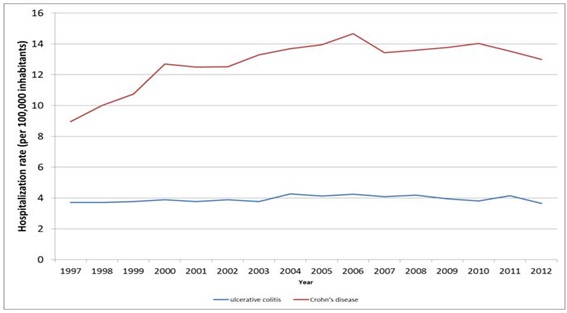
The annual hospitalization rate was 3.94 (CI 95% 3.90 - 3.99) per 100,000 population for ulcerative colitis and 12.84 (CI 95%:12.76 - 12.93) per 100,000 population for Crohn’s disease. The hospitalization rate significantly increased during the study period in the Crohn’s disease group, but remained constant in the ulcerative colitis group. While hospitalization rate in ulcerative colitis constantly increased with age, it peaked for Crohn’s disease in young adults. The hospitalization rate for Crohn’s disease has significantly increased within a 16-year period in Spain, remaining the hospitalization rate stable for ulcerative colitis. The reported trends in hospitalizations for Crohn’s disease describe an important burden on health and economic cost to the Spanish health system.
KEYWORDS
Crohn’s disease; Epidemiology; Hospitalizations; Inflammatory bowel disease; Spain; Ulcerative colitis
Introduction
The Inflammatory Bowel Disease (IBD), comprised of Ulcerative Colitis (UC) and Crohn’s Disease (CD), are idiopathic immune mediated disorders that affect an increasing number of population. The average incidence in Western Europe is estimated to be 10 per 100 000 but the overall incidence varies considerably throughout the world [1]. In the US, the incidence of IBD is rising since the 1940 with an estimated prevalence of 1 million people [2-6]. IBD is a highly prevalent disorder in Spain, with a prevalence in adults of 99.84 per 100 000 inhabitants for ulcerative colitis and 137.17 per 100 000 inhabitants for Crohn’s disease [7]. Incident cases have been increasing during the last decades as seen in several studies including a review of prospective and population based Spanish studies over time. [8-10]. With an average annual incidence rate during the period 2000 - 2012 of 5.6 per 100 000 and 8.9 per 100 000 for ulcerative colitis and Crohn’s disease, respectively [7]. Spain is reaching figures similar to those from Northern European countries.
The presentations of IBDs may vary from a single attack to chronic disabling symptoms, is often characterized by frequent hospitalizations due to relapses that might require bowel surgery, and reduce quality of life [11,12]. Whether or not the disease carries a higher mortality risk has not been fully established; some studies have shown lower and others higher mortality than background populations [13,14]. In addition, there may be subgroups of patients at risk of death from disease related conditions [15].
The use of Tumor Necrosis Factor (TNF) antagonist for IBD is associated with a reduction in the rates of hospitalizations and surgical procedures for ulcerative colitis [16-18] and Crohn’s disease [19-21].
Although the impact of anti-TNF therapy on hospitalization and surgery rates have not been demonstrated at a national level in Spain, two observational studies found a reduction in the need for hospitalizations and for surgery in clinical practice [22,23]. A Canadian study showed that nationwide hospitalization rates had modestly decreased for Crohn’s disease and remained stable for ulcerative colitis between 1994 and 2001 [24]. An increase in temporal hospitalizations and surgery rates can be partly explained by nationwide increases in prevalence of both Crohn’s disease and ulcerative colitis, but it remains unclear whether this tendency could be balanced by the use of more effective biologic therapies.
In this study we sought to determine rates and temporal patterns of hospitalizations related both to ulcerative colitis and Crohn’s disease in a 16-year period in Spain. Our secondary goal was to characterize temporal patterns in surgical utilization, length of stay and economic burden of IBD for the same time period. Hospital data cannot, of course, be used to estimate the prevalence of IBD. Nonetheless, hospital discharge data are a means of identifying and quantifying those patients who require substantial health care resources. With information from Spanish Hospital Discharged Database, this article tracks hospitalizations for IBD at the national level.
Materials and Methods
A retrospective study using the national information system for hospital data (Conjunto Mínimo Básico de Datos (CMBD)) from the Ministry of Health was performed. This system uses clinical codes from the Spanish version of the 9th International Classification of Diseases (ICD-9-MC) and includes an estimated 98% of admissions in public hospitals and 99.5% of the Spanish population [25].
All hospital discharges related to ulcerative colitis and Crohn's disease among general population reported during a 16-year period (January 1, 1997 through December 31, 2012) were obtained (Table 1). Selected ICD 9 CM codes were: 555.0: regional enteritis of small intestine, 555.1: regional enteritis of large intestine, 555.2: regional enteritis of small intestine with large intestine, 555.9: regional enteritis of unspecified site and 556.9: ulcerative colitis unspecified, Two different groups were analyzed:
Group 1: Ulcerative colitis, defined as ICD 9 CM code 556.9 in primary diagnosis position or 558.9 in any diagnosis position plus 556.9 in any diagnosis position.
Group 2: Crohn’s disease, defined as ICD 9 CM code 555.0, 555.1, 555.2 or 555.9 in primary diagnosis position or 558.9 in any diagnosis position plus 555.0, 555.1, 555.2 or 555.9 in any diagnosis position.
For each case, specific data were gathered on age, sex and region. Groups of age for study were: < 12, (12-18), (19-34), (35-54) and > 54 years old. Most frequent co-morbidities, diagnostic procedures and surgeries were also reported.
Statistical methods
The average number of hospitalizations, the Average Length Of Stay in the hospital (ALOS) and the average cost (euros) of hospital stay were calculated. ANOVA and Kruskal-Wallis tests were used for multiple comparisons by year and group of age. The annual hospitalization rate (per 100,000 inhabitants), Average Length Of Stay in the hospital (ALOS), mortality rate (per 100,000 inhabitants) and case-fatality rate (%) were calculated together with 95% confidence intervals. Data from the municipal records corrected by the CMBD National coverage were used as denominator. The distribution by age of the population covered in this study is considered to be equal to the general population.
Binomial regression (Generalized Linear Regression (GLM) with a log link and binomial distribution for the error) was used to assess differences in the rates of hospitalization (per 100,000 inhabitants) and mortality rate (per 100,000 inhabitants) by year, group of age, gender and region. Differences in proportions of case-fatality rate (%) were assessed by the Chi-square test.
The costs of these hospitalizations to the health care systems are estimation from the Ministry of Health. The cost was calculated by considering the diagnostic cost group, the total cost and the number of discharges. Diagnostic cost group was based on the Diagnosis Related Group (DRG) for hospitalized patient depending on discharge ICD classification, age, sex and resources consumption. Each group has similar weight in hospital costs and can be apply to each related patient. DRG’s calculations are made by 3M with Core Grouping System Software [26].
In all tests the significance level used was p < 0.05.Statistical analyses were performed using SAS University Edition and R Studio version 3.0.3.
The present study received a waiver for informed consent from the local ethics committee (Comité de Ética de la Investigación de la Universidad Rey Juan Carlos). The patient information was anonymized and de-identified prior to the analysis.
Results
A total of 114,700 hospital discharges due to ulcerative colitis or Crohn’s disease were reported in the 16 years study period in Spain. Of those, 26,948 (23.5%) were coded as ulcerative colitis and 87,752 (76.5%) as Crohn’s disease. Mean age was 45.3 (SD = 20.5) and 38.0 (SD = 17.3) years, respectively and 55% and 50% were female, respectively. There were a total of 957 deaths among these hospitalized patients during the study period, 392 (mean age 72 years) in ulcerative colitis and 565 (mean age 66 years) in Crohn’s disease.
Trends in hospitalization rates
The annual hospitalization rate was 3.94 (CI 95% 3.90 - 3.99) per 100,000 population for ulcerative colitis and 12.84 (CI 95%:12.76 - 12.93) per 100,000 population for Crohn’s disease. The hospitalization rate significantly increased during the study period in the Crohn’s disease group (p < 0.001), but remained constant in the ulcerative colitis group, were variations were not significant (p = 0.183) (Figure 1).
Table 2 shows the hospitalization rate for Crohn’s disease and ulcerative colitis by group of age. While hospitalization rate in ulcerative colitis constantly increased with age (p < 0.001), for Crohn’s disease the hospitalization rate peaked in young adults (19 - 34 years old).
Mortality and case-fatality rates
The mortality rate was 0.057 (CI 95% 0.052 - 0.063) per 100,000 population for ulcerative colitis and 0.083 (CI 95%:0.076 - 0.090) per 100,000 population for Crohn’s disease. The mortality rate significantly increased during the study period in the Crohn’s disease group (p = 0.023) but remained stable (p = 0.218) for the ulcerative colitis group. There was also a significant increase of mortality rate in both groups by age (p < 0.001) (Table 2).
The case-fatality rate was 1.46% (CI 95% 1.31 - 1.16) for ulcerative colitis and 0.64% (CI 95% 0.59 - 0.70) for Crohn’s disease. The case-fatality rate significantly increased during the study period in the Crohn’s disease group (p = 0.003), but did not vary (p = 0.802) for the ulcerative colitis group. Case-fatality rate dramatically increased by group of age for both groups, reaching in patients aged 55 and older 3.88% (CI 95% 3.482 - 4.279) for ulcerative colitis and 2.82% (CI 95% 2.56 - 3.08) for Crohn’s disease.
Length of stay and cost of hospitalization
The Average Length Of Stay at the hospital (ALOS) was significantly higher (p < 0.001) in those patients with ulcerative colitis (12.59 days; SD = 13.18) than in those with Crohn’s disease (11.37 days; SD = 12.32; p < 0.001). The ALOS significantly decreased during the study period (p < 0.001) and increased with age (p < 0.001) in both groups. Hospitalization costs were higher for Crohn’s disease related hospitalizations (€4442; SD = €3708) than for ulcerative colitis (€3930; SD = €3054). Costs were significantly higher in older patients in both groups.
Comorbidities
Most frequent comorbidities in Crohn’s disease group were: iron deficiency 7.4%, diabetes mellitus 3.2%, cholelithiasis and cholecystitis 2.3%, osteoporosis 1.6%, perianal abscess 1.5%, constipation 1.5% and hypercholesterolemia 1%. Most frequent comorbidities in ulcerative colitis group were: iron deficiency 8.8%, diabetes mellitus 6.5%, hypercholesterolemia 2.3%, osteoporosis 1.9%, cholelithiasis and cholecystitis 1.5% and constipation 1.3%.
Procedures
Among all the 87,752 hospitals discharged related to Crohn’s disease recorded in this study, 33% had at least a diagnostic procedure, mainly gastroscopy and colonoscopy with or without biopsy. This figure reaches the 51% in hospital discharges related to ulcerative colitis. When looking for surgical procedures, 12,417 (14%) of the patients hospitalized with Crohn’s disease had at least one surgical procedure during the hospital stay, compared with 1,871 (7%) of the patients hospitalized with ulcerative colitis. Abdominal surgery was more frequent in Crohn’s disease. The most frequent surgery for Crohn’s disease were cecectomy, partial resection of small intestine, small-to-large intestinal anastomosis and right hemicolectomy. On the other hand, colectomy was more frequent in ulcerative colitis. Other common surgeries for Crohn’s disease patients were ileostomy and perianal surgery.
Discussion
The results presented in this study are the first tracking hospitalizations for IBD on a national level in Spain and can contribute to evaluate the real burden of IBD. They showed an increase in hospitalizations for Crohn’s disease and a stable trend for ulcerative colitis during the 16 years study period between 1997 and 2012. Previous data published in Spain show an incidence rate of 3.8 per 100,000 inhabitants and year for ulcerative colitis and 1.9 per 100,000 inhabitants and year for Crohn’s disease in the late 1990s, with important regional variations and an increasing temporal trend, especially for Crohn’s disease [8,27]. This increase for Crohn’s disease has also been observed in other western countries [28].
Meanwhile ulcerative colitis related hospitalization rate increase continuously with age, Crohn’s disease highest hospitalization rate occurs in very young adults. This age pattern is in line with data published in IBD patients in Wales [29]. While previous studies showed that women were considerably more likely than men to be hospitalized for Crohn’s disease, we did not find differences in gender distribution of hospital admissions for Crohn’s disease [29,30]. On the contrary, for ulcerative colitis, our results showed that men were more likely than women to be hospitalized something that was not reported in previous published data [29]. Mortality rate, calculated with a population denominator, was higher for Crohn’s disease patients than for ulcerative colitis patients, according to the higher hospitalization rate. On the other hand case-fatality rate was higher in ulcerative colitis patients, showing the higher severity of the ulcerative colitis flares. A potential explanation for these differences found in case-fatality rate could be the 7 year higher mean age of the patients with ulcerative colitis.
As shown in previous publications, older patients with IBD-related hospitalizations have substantial morbidity and higher mortality than younger patients [31]. Our study also showed increasing mortality and case-fatality rate with age, which is consistent with a previous European study [29]. Surprisingly, despite population ageing, no rise in neither mortality, nor case-fatality rates was found in our study during the analyzed period, again in line with previous data in Europe [32].
In Crohn’s disease absolute indications for surgery include stenosing and penetrating disease not responsive to medical therapy, complex perianal disease, high grade dysplasia and cancer [33]. Ulcerative colitis surgery is limited to colectomy for not responsive severe disease, high grade dysplasia and cancer. In line with other studies our data showed that the likelihood of surgery during hospital admission was higher in ulcerative colitis patients [28].
Therapy with TNF antagonist has been associated with a significant reduction in the rates of hospitalizations and surgery for ulcerative colitis and Crohn’s disease [16-18]. However, the results of our study did not show a significant reduction in the hospitalization rate during the study period in Spain. The two TNF antagonist marketed in Spain, infliximab and adalimumab, were approved for the use in Crohn’s disease in 1999 and 2007, respectively and for ulcerative colitis in 2006 and 2013, respectively. The prescription of both drugs was initially limited and progressively raised over time, making it difficult to determine its true impact. In our study the rate of hospital admissions for Crohn’s disease peaked in 2006 and slightly decreased thereafter until 2012.
Taking into account the increasing prevalence of Crohn’s disease in Spain it seems plausible that anti-TNF therapy is contributing to stabilize the hospitalization rate for Crohn’s disease after 2006 in Spain. IBD related hospitalizations pose an important economic cost to the Spanish health system, as seen in other Western countries, like the US [28].
Strengths and Limitations
The main strength of this study is the representativeness of the CMBD hospital discharge dataset. However, use of administrative data in general has several limitations. The CMBD does not contain any personal identifiers that would allow validation of diagnostic coding with a subset of medical records. Results from different Canadian studies have demonstrated the accuracy of administrative IBD coding for research purposes [34,35]. Although this has yet to be validated in Spain for IBD, several population base studies using the CMBD data base have been performed [36-38]. The CMBD includes only patients who were admitted to hospital. Those treated in hospital but not admitted for an overnight stay are excluded, as are people treated on an outpatient basis, or primary care. Consequently, this article underestimates the true burden of inflammatory bowel disease, as it reflects only the more acute and severely symptomatic cases. Another limitation of the study is that the unit of observation is a hospitalization and not a unique patient. Therefore, we cannot distinguish whether rising trends in hospitalizations are due to increases in the number of patients who are hospitalized, readmissions, or both. It has to be taken into account that we only considered direct healthcare costs. The indirect costs related, essentially, to the patient’s loss of productivity, were not included.
In conclusion, we have shown by using nationwide hospital discharge data that the hospitalization rate for Crohn’s disease has significantly increased within a 16-year period in Spain, remaining the hospitalization rate stable for ulcerative colitis. It remains unclear whether the increase in IBD hospitalizations can be attributed to an increase in the prevalence of IBD. If that was the case, prevention research must focus on identifying modifiable environmental and life style factors and design strategies to identify individuals at risk of hospitalization due to the underlying disease process. Our findings reinforce the need for effective treatment strategies to reduce IBD complications.
Acknowledgments
Thanks to the Subdirección General delInstituto de Información Sanitaria for providing the information upon which this study is based.
Funding
The cathedra “Evaluación de Result adosen Salud. Rey Juan Carlos University” is sponsored by Abbvie.