
Pressure-Induced Skin and Soft Tissue Injury in Hospitalized Elderly: Prevalence and Characteristics
*Corresponding Author(s):
Javier Alonso RamírezDepartment Of Geriatric Medicine, Insular Hospital Of Lanzarote, PhD Research In Biomedicine, University Of Las Palmas De Gran Canaria (ULPGC), Las Palmas, Spain
Tel:+34 0034928810000,
Email:xaalonso86@gmail.com
Abstract
Pressure-induced skin and soft tissue injury (PU) are important factors that limit quality of life in older adults and are especially prevalent in two situations: hospitalizations and immobility. It’s caused by multiple factors, external (humidity, shearing) and internal (protein deficit, cachexia). PU development is an indicator of poor health outcome. Age and Barthel Index are two important variables involved in PU development. The increased awareness of health professionals has systematically increased risk assessment and prevention (both primary and secondary) in hospital admissions.
Keywords
INTRODUCTION
Pressure-induced skin and soft tissue injury (PU) is a skin and subcutaneous tissue injury, usually located on a bony prominence as a result of pressure maintained between two hard planes and the intolerance of the tissues to this pressure. It is initially located in the underlying tissue and is identified by color change in the skin. Its origin is multifactorial, due to combined action of external factors (pressure, humidity,…), internal factors (protein deficiency, cachexia,…) and the pressure-time ratio [1].
PU’s are present as rounded or oval lesions located perpendicular to the bony prominences. The most frequent location is: sacrum (32.8%), heels (28%), trochanters (7.6%) and malleoli (6.6%). Its presence in other locations depends on anatomical position adopted during long periods of time [2,3]. A study carried out in Spain reveals that in patients older than 65 the prevalence of PU was 7.8%. Patients who exhibited higher incidence of PU were older adults with hospital admissions longer than 4 days. 59.4% of the PU in hospitalized patients. People older than 65 are at 2.4 times more risk to develop an Adverse Effect (AE) during hospital admissions. In a study conducted by Torra-Bou the incidence of adverse effect related health care was 9.3% [4]. Of this percentage 8.4% corresponded directly to hospital assistance. Seven percent of the AE were directly linked to personal care and Pressure Ulcer (PU) occurred in 3.7% of this elderly subpopulation [4,5].
The PU’s represent one of the main complications of immobility syndrome (spinal cord injuries, advanced dementias, intensive care units, etc.), associating greater morbimortality [6]. The etiology is determined by microscopic changes: edema, cellular infiltration, extravasation and degeneration of hyaline cartilage. These changes in the subcutaneous tissue begin with application of 60 mmHg of pressure for at least one hour. The main prevention strategies are postural changes every two hours. Decubitus lateral position in 90º have an almost 4 times higher rate of injuries than those that are at 30° [1]. A study carried out by Marisa et al., showed that PU prevention protocols reduced the incidence from 41.02% to 23.1% in an intensive care unit [7]. Postural changes, special pressure-management surfaces associated with nutritional support and skin friction prevention are multicomponent strategies that decrease its prevalence. PU’s in hospitalized patients could be prevented in 95-98% of cases [8].
Treatment of PU’s is mainly based on prevention. The first approach to consider is the identification of patients at higher risk of PU. Risk identification, postural changes, skin hygiene and hydration, adequate nutritional support, pressure point protection and constant skin evaluation is the most efficient multidimensional plan [9]. The Braden scale is broadly used for staging PU. Low scores in Braden scale help to identify patients at risk and identify need for specific assistance. This scale includes six parameters [10]: sensory/perception, moisture, activity, mobility, nutrition and friction/shearing. Each subscale has a score of 1 to 4, except for friction. In addition to the score, it considers factors such as age (older than 65), fever, low protein intake, diastolic pressure (below 60 mmHg) and/or hemodynamic instability. Thus, patients are classified in low risk (15 to 18 points), moderate risk (13 to 14 points), high risk (10 to 12 points) and very high risk (9 or less points).
In a study conducted by Homs-Romero, in which 459 professionals participated (nurses, physicians and auxiliaries), 87.7% considered the PU a severe adverse event during hospitalization, particularly the nurse group [8]. PU´s are preceded by a lesion in the deep tissues. First, appears a purple or red coloration in the skin and/or increase the temperature in the area. Once the PU appears it is classified as [11].
Category I: Nonblanchable erythema: Intact skin with non-blanchable erythema of a localized area, usually on a bony prominence. Skin discoloration, heat, edema, hardening, or pain may also be present. The area can be painful, firm, soft, hotter or colder than adjacent tissues. The erythema does not pale/disappear with pressure (Figure 1).
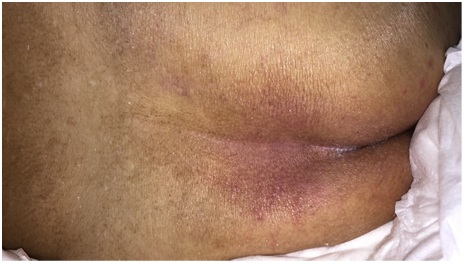 Figure 1: Pressure ulcer stage 1.
Figure 1: Pressure ulcer stage 1.
Category II: Partial-thickness loss of skin: The loss of partial thickness of the dermis is presented as a shallow open ulcer with a wound bed between pink and reddish. An intact or ruptured serum-filled blister may be observed (Figure 2).
 Figure 2: Pressure ulcer stage 2.
Figure 2: Pressure ulcer stage 2.
Category III: Full-thickness loss of skin: At this stage a complete loss of the thickness of the tissue is observed. Adipose tissue (subcutaneous fat) may be visible. It should be considered that the PU depth varies according to location and the patient's anatomy. Fascia, muscle, tendon, ligament, cartilage and/or bone are not exposed. This exhibits a lesion of the subcutaneous tissue, which may extend to the muscular fascia (Figure 3).
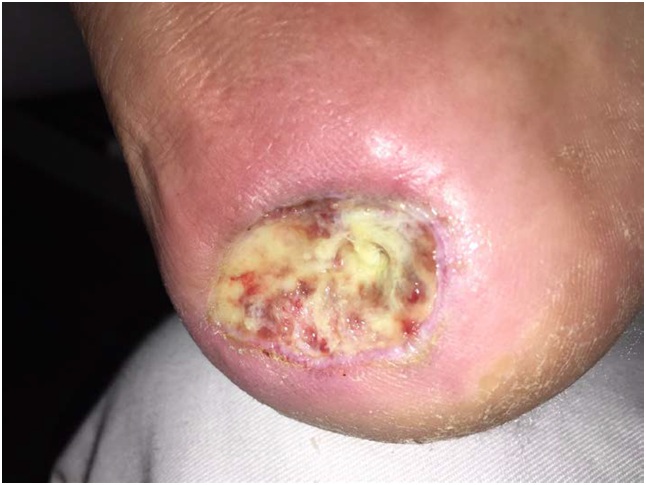 Figure 3: Pressure ulcer stage 3.
Figure 3: Pressure ulcer stage 3.
Category IV: Total loss of tissue thickness: This category produced total loss of tissue with exposed bone, tendon, or muscle. This can extend to the muscle and/or support structures, which may cause the appearance of osteomyelitis or osteitis. The exposed bone/muscle is visible or directly palpable (Figure 4).
 Figure 4: Pressure ulcer stage 4.
Figure 4: Pressure ulcer stage 4.
Unstageable: Unknown depth: Loss of total thickness of tissues where the base of the ulcer is completely covered by slough or eschar. The depth of the wound cannot be confirmed. This usually happens because there is a lot of dead tissue in the wound (Figure 5).
 Figure 5: Pressure ulcer unstageable.
Figure 5: Pressure ulcer unstageable.
METHODOLOGY
The main objective is to describe principle variables of patients with PU in the Geriatric Service in Lanzarote Hospital. A secondary objective is to identify the main agents that colonize the PU. The variables studied are: age, gender, reason of admission, social situation, presence of physical or cognitive impairment, location and culture of PU. We registered Barthel index as a measure of daily activities autonomy (100 better autonomy, 0 completely dependent) [6].
It is an observational retrospective study, of 31 hospitalized patients for a period of 2 months (December and January). The inclusion criteria were: admission to a long-term geriatric unit and exhibiting at least one PU. The following exclusion criteria were applied: not having the complete history or other etiology of ulcer (vascular, mixed). The initial population was 66 hospitalized patients. Once the inclusion and exclusion criteria were applied, a total of 35 (53.03%) were excluded from the study for exhibiting vascular etiology of the PU or missing some clinical history.
RESULTS
The sample consisted of 31 patients admitted to the acute unit and that meet all the inclusion criteria. In relation to the gender, 17 were women (54.8 %) and 14 males (45.2%). Aged between 55 and 102 years (mean 80.42 years Sx 10.61). Patients over 85 represent 32% of the sample. The reason for admitting the patients were immobility syndrome in 50% of patients, followed by infectious disease (17.9%) and acute functional decline (10.7%). The procedence of PU was 45.12% from acute geriatric service and 54.88% from other services (day hospital and long term units). PU cultures were positive for pathogen in an 83.9% of the patients (n=26); 69.2% were due to polymicrobial infection, followed by S. Aureus y Proteus mirabillis (11.5%). In the older subgroup (>85 years) the ratios of positive cultures increased to 90%.
The preferred location was heel (36.3%), sacrum (30%) and trochanter (26.7%). The PU was characterized as stage III (58.1%) and IV (29%). From whole sample 67.8% of the patients presented cognitive impairment in moderate-severe degree (GDS-FAST≥6). 12.9% has no cognitive decline. While that 80.6% present total dependence for daily day activities (Barthel index below 20 points). In 74-85 group 92.3% were dependent (n=13) while in those older than 85 (n=10) 100% were severe dependent patients. The more relevant comorbidities were described in table 1.
|
Comorbidities |
Percentage (%) |
|
Incontinence |
86.7 |
|
Cerebrovascular disease |
36.7 |
|
Cardiovascular disease |
36.7 |
|
Respiratory pathology |
30 |
|
Fracture (hip or vertebral) |
13.3 |
|
Cancer |
10 |
Table 1: Relevant comorbidities.
DISCUSSION
The data found in the literature are consistent with that found in this study. Age is an important risk factor for the PU [4,5]. In addition, the incidence has a negative correlates with the Barthel index. The lower score, the higher incidence of PU. It is associated with greater morbidity-mortality [6]. In relation to localization, it is fulfilled what is found in the scientific literature. The most frequent location of PU is sacrum, heels and trochanters [2,3]. The percentage of PU found in the heel was higher in this study. Both urinary and fecal incontinence were the most prevalent comorbidities which is consistent with found by other authors and increases risk of PU development [12].
Health professionals (physicians, nurses or auxiliaries) are aware of the importance of both the identification of patients at risk and prevention (both primary and secondary) of PU. This coincides with in relation to the adverse effects linked to geriatric patient hospital admission [8]. Prevention is the more important and cost-efficient intervention [12].
ETHICAL RESPONSIBILITIES
The authors state that the procedures followed were in line with the ethical standards of the responsible human experimentation committee and in agreement with the World Medical Association and the Helsinki Declaration.
CONFIDENTIALITY OF THE DATA
The authors state that they have followed the protocols of their work center on the publication of patient data.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
REFERENCES
- López-Casanova P, Verdú-Soriano J, Berenguer-Pérez M, Soldevilla-Agreda J (2018) Prevención de las úlceras por presión y los cambios de postura. Revisión integrativa de la literatura. Gerokomos 29: 92-99.
- Agreda JJS, Bou J-ET I, Soriano JV, Casanova PL (2011) 3.er Estudio Nacional de Prevalencia de Úlceras por Presión en España, 2009. Epidemiología y variables definitorias de las lesiones y pacientes. Gerokomos 22: 77-90.
- Ortiz-Vargas I, García-Campos ML, Beltrán-Campos V, Gallardo-López F, Sánchez-Espinosa A, et al. (2017) Cura húmeda de úlceras por presión. Atención en el ámbito domiciliary. Enfermería Universitaria 14: 243-250.
- Torra-Bou JE, Verdú-Soriano J, Sarabia-Lavin R, Paras-Bravo P, Soldevilla-Ágreda JJ, et al. (2016) Las úlceras por presión como problema de seguridad del paciente. Gerokomos 27: 161-167.
- Aranaz-Andrés JM, Limón R, Mira JJ, Aibar C, Gea MT, et al. (2011) What makes hospitalized patients more vulnerable and increases their risk of experiencing an adverse event? Int J Qual Health Care 23: 705-712.
- Agreda JJS, Bou J-ETI, Soriano JV, Cuervo FM, Casanova PL, et al. (2006) 2º Estudio Nacional de Prevalencia de Úlceras por Presión en España, 2005. Epidemiología y variables definitorias de las lesiones y pacientes. Gerokomos 17: 154-172.
- Rogenski NMB, Kurcgant P (2012) The incidence of pressure ulcers after the implementation of a prevention protocol. Revista Latino-Americana de Enfermagem 20: 333-339.
- Homs-Romero E, Güimil JAE, Rodríguez TL, Lombardo FC, Pérez MC, et al. (2018) Percepción de los profesionales sanitarios sobre la gravedad de las úlceras por presión como evento adverso. Gerokomos 29: 39-44.
- Pegenaute EA, de Galdiano Fernández AG, Ciarrusta NZ, Coscojuela MÁ, Erro CAM (2005) Úlceras por presión en cuidados intensivos: valoración del riesgo y medidas de prevención. Enfermería Intensiva 16: 153-163.
- Fernandes LM, Caliri MHL (2008) Using the braden and glasgow scales to predict pressure ulcer risk in patients hospitalized at intensive care units. Revista Latino-Americana de Enfermagem 16: 973-978.
- NPUAP (2014) NEW 2014 treatment of pressure ulcers: clinical practice guideline. NPUAP, Washington, D.C., USA.
- Baumgarten M, Margolis DJ, Localio AR, Kagan SH, Lowe RA, et al. (2006) Pressure ulcers among elderly patients early in the hospital stay. J Gerontol A Biol Sci Med Sci 61: 749-754.
Citation: Ramírez JA, Fernández FJB, Hernandez DP, Mendoza GP (2018) Pressure-Induced Skin and Soft Tissue Injury in Hospitalized Elderly: Prevalence and Characteristics. J Gerontol Geriatr Med 4: 021.
Copyright: © 2018 Javier Alonso Ramírez, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

