The Impact of Obesity on United States Health Care Expenditures
*Corresponding Author(s):
Eric R CarlsonDepartment Of Oral And Maxillofacial Surgery, University Of Tennessee Medical Center, 1930 Alcoa Hwy, Knoxville, Tennessee, United States
Tel:+1 8653053904,
Email:ecarlson@mc.utmck.edu
Abstract
Keywords
Bariatric surgery; Cancer; Diabetes; Dyslipidemia; Morbidly obese; Obese; Overweight
INTRODUCTION
MEDICAL SEQUELAE ASSOCIATED WITH OBESITY
Type 2 diabetes and dyslipidemia are associated with obesity and increased BMI, weight gain and increased abdominal fat distribution are established risk factors for the development of type 2 diabetes. It is estimated that 90% of patients with type 2 diabetes are obese [8].The American Diabetes Association reported that the estimated annual cost of diabetes in medical expenditures increased from $132 billion to $174 billion in 2007, in no small part due to the epidemic of obesity in the United States [9]. Obesity is also associated with elevated triglycerides, low levels of High Density Lipoprotein (HDL) cholesterol and high levels of Low Density Lipoprotein (LDL) cholesterol that together define dyslipidemia. The association of obesity, type 2 diabetes and several human cancers has gained significant attention due to the increased prevalence of obesity and type 2 diabetes [10]. Multiple etiologic factors are considered in the pathogenesis of cancer in obese patients with type 2 diabetes including hyperglycemia with hyperinsulinemia, insulin-like growth factor I, dyslipidemia, adipokines and cytokines and an altered gut microbiome [2,10]. Overweight and obese states are associated with cancer of the uterus, esophagus, kidneys, pancreas, ovaries, breast, colon and gallbladder [1,2,10]. In addition to the increased prevalence of cancer in obese patients, there is an increased risk of death of patients with these cancers [2,11].
Obese men and women are increasingly being diagnosed with Obstructive Sleep Apnea Syndrome (OSAS) that is manifest by partial or complete upper airway obstruction during sleep. These airway obstructions result in periods of apnea (no airway flow) or hypopnea (decreased airway flow), both of which lead to hypoxemia (decreased oxygen concentration of the arterial blood). Symptoms of OSAS include daytime somnolence and hypertension. Substantial medical expenditures are realized in the surgical and non-surgical treatment of OSAS including those related to the use of Continuous Positive Airway Pressure (CPAP) devices.
Obesity is also associated with non-alcoholic fatty liver disease that is associated with hepatomegaly, abnormal liver function blood tests and macrovesicular steatosis that can lead to cirrhosis. While once contested, it is now well known that fatty liver related to obesity leads to cirrhosis that in turn results in increased mortality [12]. Of further note is the association of osteoarthritis and obesity. Osteoarthritis is the most common musculoskeletal disorder and a leading cause of functional disability in the United States. While formerly attributed to the “wear and tear” mechanical and aging processes, osteoarthritis of the major joints is now believed to be associated with obesity, trauma, heredity and metabolic syndrome related to dyslipidemia [13]. Courties et al., reported that hypercholesterolemia and hypertriglyceridemia, both associated with obesity, have been associated with increased risk of osteoarthritis, while increased HDL levels are protective against osteoarthritis of the knee joint [13]. The total number of total knee replacement procedures performed each year now exceeds 640, 000 at a total annual cost of about $10.2 billion [14].
Evidence also exists that obesity is also associated with cognitive dysfunction [15]. Obesity is known to be an independent risk factor for Alzheimer’s disease and is associated with temporal lobe atrophy in adults. Gundstad et al., studied 408 patients from the Brain Resource International Database and categorized them according to BMI and age [15]. There were 178 normal weight younger adults, 140 overweight/obese younger adults, 32 normal weight older adults and 58 overweight/obese older adults. Body mass index was significantly related to performance in all cognitive tests in the study, even in seemingly healthy adults. Excluding people with significant medical comorbidity permitted the authors of this study to determine the independent contribution of elevated BMI in impaired cognitive function. Further, Boeka and Lokken examined neuropsychological performance in a cohort of morbidly obese patients as part of preoperative assessment for weight loss surgery [5]. Their results indicated differences in cognitive performance of morbidly obese patients on tests of executive functioning including planning, mental flexibility and problem solving compared to normative data. No significant differences were identified between obese patients with and without diagnosed medical comorbidity including hypertension, type 2 diabetes and OSAS that supports the independent involvement of obesity in cognitive dysfunction.
ECONOMIC CONSEQUENCES OF OBESITY
Adults
The increased prevalence of obesity that has occurred in the U.S. during the last 30 years has been accompanied by a substantial increase in the literature on the direct medical cost of obesity [20]. Cost of illness estimates are commonly cited in the medical literature despite debate about the usefulness of quantifying the cost of illness in general and the cost of overweight and obesity, specifically [21,22]. For example, the American Diabetes Association estimated that the 2004 annual cost of diabetes in medical expenditures and lost productivity increased from $132 billion in 2002 to $174 billion in 2007 [9]. The American Heart Association estimated the direct and indirect cost of cardiovascular disease to be $403.1 billion in 2006 [23]. Although some cost estimates for overweight/obesity, diabetes and heart disease may double count one another, it is important to understand the magnitude of costs that could potentially be saved by better prevention and treatment of obesity.
In 2017, Biener et al., analyzed data from MEPS for 2001-2015 and estimated the percentage of healthcare costs associated with obesity in adults in the most highly populated states and the United States as a whole [19]. These authors examined the direct economic implications of obesity and also assessed the indirect economic impact of obesity including labor market outcomes such as employment, job absenteeism and lost wages. The authors identified some fluctuation in medical expense due to obesity from 2001-2015, but noted an upward trend in the share of national expenditures associated with obesity during this 15-year time period. For the United States as a whole, the percentage of medical expenses related to obesity increased from 6.13% in 2001 to 7.91% in 2015. The lowest expenditure for obesity was noted in Maryland in 2001 (3.57%) and the highest expenditure was noted in North Carolina (14.55%) in 2011. Overall at the state level, the authors found that medical expenses related to obesity were lowest in California, Florida and New York (3-6%) and highest in Illinois, North Carolina, Ohio, Virginia and Wisconsin (8-14%). The medical expenditures for obesity increased 83% in Maryland and 52% in Kentucky during this time period. Many factors were suggested for the disparities in states including differences in the prevalence of obesity, differences in healthcare utilization among the obese, differences in how physicians treat obesity and differences in the cost of medical services. The authors also examined the total medical expenditures associated with obesity as a function of payer including Medicare, Medicaid, commercial health insurance and out of pocket spending by the patient. The average percentage of expenditures for medical care related to obesity between 2010 and 2015 was 9.21% for commercial insurance, 6.86% for Medicare, 8.48% for Medicaid and 4.74% for patient out of pocket spending. The expenditures by Medicare and Medicaid are of particular interest because they indicate the medical costs assumed by society. Specifically, an average of 11.96% of Medicare expenditures in 2001-2015 were devoted to prescription drugs related to obesity while an average of 14.35% of Medicaid expenditures in 2001-2015 were devoted to prescription drugs related to obesity. By contrast, during the same time period, 5.19% of Medicare expenditures and 4.75% of Medicaid expenditures were devoted to inpatient hospital care related to obesity. From 2001-2015 an average of 11.29% of out of pocket prescription drug expenditures were related to care for obesity. Finally, these authors reported that their review of the international literature of the causal effects of obesity on economic outcomes indicated that obesity reduced the probability of employment. In their review, a 1% decrease in BMI was associated with a 2.1% increase in the retention of employment of obese women but no change in the employment of men. In terms of lowered earnings and wages for obese individuals, Biener et al., review of the literature revealed that BMI tends to correlate with wages in a significant and negative fashion for women but not statistically significant for men [19]. Among women, for example, the most significant impact is for white women where an additional 10 pounds lowers wages by 2.8% compared to a biologic sibling.
In 2017 Biener et al., further assessed the expenditures associated with medical care associated with obesity and found that obesity raised individual medical care costs by $3,429 per year in 2013 dollars [24]. With the assumption that the effects of obesity in Biener’s study population, (adult respondents to the MEPS who have biological children in the household) generalizes to the full noninstitutionalized population of American adults, the total medical care costs of obesity for noninstitutionalized adults totaled $342.2 billion in 2013 that equated to 28.2% of all healthcare costs in this population that were attributable to obesity.
Tsai, Williamson and Glickper formed a systematic review of the direct cost of overweight and obesity in the United States [16]. PubMed (1968-2009), EconLit (1969-2009) and Business Source Premier (1995-2009) were searched for applicable published studies, specifically those that calculated the incremental cost per overweight and obese persons and to calculate the national aggregate cost. The search strategy combined the terms “obesity” or “obesity, morbid” with any of the following terms: “costs and cost analysis”, employer health costs”, “cost of illness” and “health care costs”. The authors reviewed a total of 935 published papers or abstracts that only included United States subjects. A total of fifty United States studies were identified and seventeen studies were excluded for a variety of reasons, including median, rather than mean cost reported (n=1); unable to calculate the annual cost of obesity from the data reported (n=1); direct and indirect costs were combined (n=1); no BMI cutoff discussed (n=4); only inpatient or outpatient costs were included (n=3) and duplicate dataset (n=7). A total of thirty-three studies published between 1992 and 2008 comprised this systematic review. Of these, 24 reported on the cost of overweight, 30 on the cost of obesity and 26 on the cost of overweight and obesity combined. These authors reported that only four studies met all study criteria for their designation of a high-quality study, including analysis of adults of all ages, use of standard BMI designations, reporting cost or expenditure and the use of nationally representative samples. In these four studies, the medical costs in 2008 dollars ($Y2008) of overweight was $266, for obesity $1,723 and for overweight and obesity combined $1,023.The aggregate national cost of overweight and obesity was 4.8% of United States health spending in 2008 based on National Health Expenditure Accounts (NHEA) data. Finkelstein et al., who used the Medical Expenditure Panel Survey (METS) data, reported that the incremental cost of obesity to be $1,429 and that the cost of overweight was not significantly different than the cost of normal weight [25]. The total healthcare spending of obesity was estimated to be 9.1%. Among all studies in the systematic review, the incremental cost of overweight was $498. Among the 23 studies that reported estimates of both the cost of normal weight and the incremental cost of overweight, the cost of overweight was 9.9% greater than the cost of normal weight patients. The aggregate national cost of overweight and obesity combined was $113.9 billion ($Y2008). Five studies reported cost estimates for morbid obesity (BMI greater than 40 kg/m2). These studies indicated an average incremental cost of $3,012 that represented a 68% increase over the cost of normal weight. The cost of morbid obesity accounted for 35% of the total cost of obesity.
Children and Adolescents
PREVENTION OF OBESITY-THEORIES OF ACTION
If obesity were successfully addressed, then comorbid diseases would be less prevalent. If comorbid diseases were less prevalent, then United States healthcare expenditures would decrease.
If the incidence of obesity could be reduced in children and adolescents, then fewer American adults would suffer comorbid diseases with resultant decreased United States healthcare expenditures.
Priority must be given to preventive interventions that are cost effective and those that realize cost savings. Cecchini and Sassi retrospectively examined the economic impact of education, counseling and long-term drug treatment on national health care expenditures and the use of healthcare services compared to business as usual approaches in the United States [27]. In 2010, prevention interventions had the potential to decrease total annual healthcare expenditure by up to $2 billion, although the estimate did not include the implementation costs. The largest portion of savings (60.6%) is produced by reduced inpatient care, followed by reduced use of drugs. The reduction in expenditure for outpatient care would be more limited. In the final analysis prevention initiatives for obesity may produce a significant decrease in the use of health care services and expenditures. Savings would become significant when implemented over a long period of time. Finally, Lee et al., indicated that using a computational simulation model in United States children ages 8-11 years of age, maintaining the current physical inactivity level would result each year in a net present value of $1.1 trillion in direct medical costs and $1.7 trillion lost productivity over the course of their lifetimes [28]. The authors indicated that if 50% of children would exercise, the number of obese and overweight youth would decrease by 4.18% thereby averting $8.1 billion in direct medical costs and $13.8 billion in lost productivity. Increasing the proportion of children who exercised to 75% would avert $16.6 billion and $23.6 billion in lost productivity. In the final analysis, national guidelines that recommend that children and adolescents engage in 60 minutes of moderate to vigorous physical activity each day represent an effective strategy to reduce the negative health impacts of obesity on American society while also markedly reducing the health care expenditures associated with obesity [29].
PRESCRIPTION WEIGHT LOSS DRUGS
|
pproved Weight Loss Drugs |
Orlistat(Xenical®, alli®) |
Phentermine-Topiramate(Osymia®) |
Lorcaserin(Belviq®) |
Naltrexone-Bupropion(Contrave®) |
Liraglutide (Saxenda). |
|
Type of Drug |
Peripherally acting pancreatic lipase inhibitor; ↓ absorption of ingested fat. |
Appetite- suppressant (sympathomimetic amine) and anticonvulsant. |
Selective serotonin 2c (5HT-2c) receptor agonist; stimulates 5HT-2c receptors in appetite center. |
Dopamine and norepinephrine reuptake inhibitor and opioid antagonist. |
Glucagon-like peptide 1 receptor agonist. |
|
Dosing and Evaluation |
120 mg, 3 times daily with meals (or OTC alli® at half dose, 60 mg) |
Start 3.75/23mg, ↑ to 7.5/46mg after 2 weeks. Evaluate after 12 weeks; ↑ dose or d/c if < 3% weight loss. |
10 mg twice daily (does not require titration) or 20 mg ER once daily. Evaluate after 12 weeks; d/c if weight loss < 5%. |
Week 1: 8 mg/90 mg daily; ↑ weekly to target daily dose 32 mg/360 mg by week 4 (two pills, twice daily). Evaluate after 12 weeks on target dose; d/c if weight loss < 5%. |
SubQ injection (arm, thigh, abdomen; rotate site). Start at 0.6 mg daily; ↑ by 0.6 mg weekly for 5 weeks to target dose 3 mg. Evaluate after 16 weeks; d/c if weight loss < 4%. |
|
Adverse Effects |
GI (diarrhea, flatulence), especially if large amounts fat ingested. |
Paresthesia, dizziness, dry mouth, dysgeusia, insomnia, constipation. |
Headache, dizziness, fatigue, nausea, dry mouth, constipation; hypoglycemia with other diabetes drugs. |
Nausea, diarrhea, constipation, headache |
Nausea; GI symptoms. |
|
Precautions |
Binds fat-soluble vitamins; have patient take daily multivitamin at bedtime. ↑ urinary oxalate; predisposes to kidney stones. |
Known teratogen; rule out pregnancy before starting; test monthly during treatment. |
Serotonin/neuroleptic malignant syndrome if on serotonergic or anti- dopaminergic drug; valve disease, CHF, psychiatric disorders; priapism. |
Warning about suicidal thoughts in patients < 24 years. |
Hypoglycemia a risk in patients on antidiabetic meds; may be severe in those on sulfonylureas or insulin. |
|
Contraindications |
Pregnancy, cholestasis, malabsorption syndromes, use of cyclosporine. |
Pregnancy, glaucoma, use of MAOIs, hyperthyroidism. |
Pregnancy |
Pregnancy; uncontrolled hypertension; seizure disorders; chronic opioid use; MAOI use. |
Pregnancy, breastfeeding; thyroid cancer, multiple endocrine neoplasia type 2, acute pancreatitis. |
|
|
|
|
|
|
|
Adapted from: Kahan S: Quick takes: What you should know about the 5 FDA approved obesity drugs. www.Medscape.com. March 2, 2017. Accessed January 15, 2018.
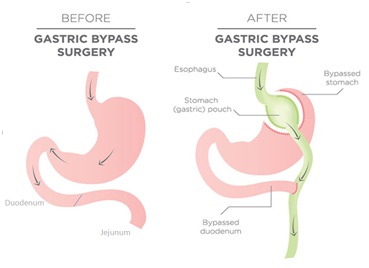
BARIATRIC SURGERY FOR OBESITY
DISCUSSION
Poverty reduction policies including the 1996 Personal Responsibility and Work Opportunity Reconciliation Act have led to a marked increase in the involvement of women with young children in the labor force. In 2009 the United States Department of Labor, Bureau of Labor Statistics reported an increase in the number of employed mothers with children under the age of 18 from 47% in 1975 to 71% in 2008 [34]. With women steadily moving into the paid labor force, men have consequently increased their contributions to household labor including the production and support of child health. Changes in family structure and dynamics, particularly the significant rise in dual-earner families and working single parent families, are important factors that are likely contributing to escalating obesity rates among children and adolescents [35]. While studies investigating the positive association between the expansion of the maternal workforce and childhood obesity rates exist, evidence is largely absent demonstrating the role of fathers in child weight [34]. Benson and Mahktari used economic theory, a nationally representative dataset and proper econometric modeling and analysis to study the joint role of parental employment on children’s health utilizing the metric of Percentile Body Mass Index (pBMI) [34]. Specifically, these authors used the 2007 wave of the Child Development Supplement (CDS) of the Panel Study of Income Dynamics (PSID) for children who live with both parents to address how father’s work hours influence childhood obesity. Intuitively, the study identified that decreases in parental contributions to child health associated with increased parental labor force participation negatively impacted child health with increases in childhood obesity. The positive coefficient estimates on mother’s (12%) and father’s (2%) hours of work were felt to be consistent with the joint parental decision making process in promoting favorable child health. The influence of father’s hours of work in the study was more than double that of mother’s hours of work. The study identified another predictor of child pBMI in parental wages was measured by the log of the mother’s wage relative to that of the father’s wage. Higher hourly wage for mothers relative to those of father’s were predictive of lower pBMI outcomes for their children. Sociodemographic factors were also influential in pBMI in that being Hispanic had the highest positive influence on pBMI, while being geographically located in the south and increasing child age were associated with lower pBMI. Other protective factors influencing pBMI included parent-child activities such as reading, building, talking, performing yard work, engaging in sports, hand crafts, washing dishes and completing homework, all of which decreased pBMI. The building/repair work was associated with a decreased risk for overweight and obese childhood states presumably due to increased expenditures of calories. The observation of reading being associated with decreased likelihood of overweight and obese states suggests that this activity might support engagement with children with subsequent motivation for adopting physical activity and weight control goals. In the final analysis, the findings of this research indicate that father’s household production input hours may be more efficient than those of mother’s in terms of the production of child health. Father’s may benefit, therefore, from training, social support and educational resources emphasizing the health issues of children including meal preparation, the encouragement of physical activities and social support.
CONCLUSION
CONFLICT OF INTEREST
REFERENCES
- Mitchell N, Catanacci V, Wyatt RR, Hill JO (2011) Obesity: Overview of an epidemic. Psychiatr Clin North Am 34: 717-732.
- Berger NA (2014) Obesity and cancer pathogenesis. Ann N Y Acad Sci 1311: 57-76.
- Flegal KM, Carroll MD, Kit BK, Ogden CL (2012) Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 307: 491-497.
- Finkelstein EA, Khavjou OA, Thompson H, Trogdon JG, Pan L, et al. (2012) Obesity and severe obesity forecasts through 2030. Am J Prev Med 42: 563-570.
- Boeka AG, Lokken KL (2008) Neuropsychological performance of a clinical sample of extremely obese individuals. Arch Clin Neuropsychol 23: 467-474.
- Pandya A, Gaziano TA, Weinstein MC, Cutler D (2013) More Americans living longer with cardiovascular disease will increase costs while lowering quality of life. Health Aff (Millwood) 32: 1706-1714.
- Trogdon JG, Murphy LB, Khavjou OA, Li R, Maylahn CM, et al. (2015) Costs of chronic diseases at the state level: The chronic disease cost calculator. Preventing Chronic Disease 12: 150131.
- Allison DB, Saunders SE (2000) Obesity in North America: An overview. Med Clin North Am 84: 305-332.
- American Diabetes Association (2008) Economic costs of diabetes in the U.S. In 2007. Diabetes Care 31: 596-615.
- Gallagher EJ, LeRoith D (2015) Obesity and Diabetes: The Increased risk of cancer and cancer-related mortality. Physiol Rev 95: 727-748.
- Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ (2003) Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med 348: 1625-1638.
- Adler M, Schaffner F (1979) Fatty liver hepatitis and cirrhosis in obese patients. Am J Med 67: 811-816.
- Courties A, Sellam J, Berenbaum F (2017) Metabolic syndrome-associated osteoarthritis. Curr Opin Rheumatol 29: 214-222.
- Ferket BS, Feldman Z, Zhou J, Oei EH, Bierma-Zeinstra SMA, et al. (2017) Impact of total knee replacement practice: Cost effectiveness analysis of data from the Osteoarthritis Initiative. BMJ 356: 1131.
- Gunstad J, Paul RH, Cohen RA, Tate DF, Spitznagel MB, et al. (2007) Elevated body mass index is associated with executive dysfunction in otherwise healthy adults. Compr Psychiatry 48: 57-61.
- Tsai AG, Williamson DF, Glick HA (2011) Direct medical cost of overweight and obesity in the USA: A quantitative systematic review. Obes Rev 12: 50-61.
- https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/2012AgeandGenderHighlights.pdf
- Kornfeld R, Harman R, Catlin A (2010) Health Care expenditures in the national health expenditures accounts and a gross domestic product: A reconciliation. BEA working paper, Washington, DC, USA.
- Biener A, Cawley J, Meyerhoefer C (2018) The impact of obesity on medical care costs and labor market outcomes in the US. Clin Chem 64: 108-117.
- Wang Y, Beydoun MA (2007) The obesity epidemic in the United States-gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev 29: 6-28.
- Roux L, Donaldson C (2004) Economics and obesity: Costing the problem or evaluating solutions? Obes Res 12: 173-179.
- Williamson DF, Narayan KM, Teutsch SM (1998) The economic impact of obesity in the United States: Whither? Obes Res 6: 173-175.
- Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, et al. (2006) Heart disease and stroke statistics-2006 update: A Report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 113: 85-151.
- Biener A, Cawley J, Meyerhoefer C (2017) The high and rising costs of obesity to the US health care system. J Gen Intern Med 32: 6-8.
- Finkelstein EA, Trogdon JG, Cohen JW, Dietz W (2009) Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood) 28: 822-831.
- Wright DR, Prosser LA (2014) The impact of overweight and obesity on pediatric medical expenditures. Appl Health Econ Health Policy 12: 139-150.
- Cecchini M, Sassi F (2015) Preventing obesity in the USA: Impact on health service utilization and costs. Pharmacoeconomics 33: 765-776.
- Lee BY, Adam A, Zenkov E, Hertenstein D, Ferguson MC, et al. (2017) Modeling the economic and health impact of increasing children’s physical activity in the United States. Health Aff (Millwood) 36: 902-908.
- Cradock AL, Barrett JL, Kenney EL, Giles CM, Ward ZJ, et al. (2017) Using cost-effectiveness analysis to prioritize policy and programmatic approaches to physical activity promotion and obesity prevention in childhood. Prev Med 95: 17-27.
- Kahan S (2018) Quick takes: What you need to know about the 5 FDA-approved obesity drugs. Medpace, Cincinnati, Ohio, USA.
- Rosenthal RJ, Morton J, Brethauer S, Mattar S, DeMaria E, et al. (2017) Obesity in America. Surg Obes Relat Dis 13: 1643-1650.
- Adams TD, Davidson LE, Litwin SE., Kim J, Kolotkin RL, et al. (2017) Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med 377: 1143-1155.
- Mokhtari M, Pollock ED (2015) Weight, mental health, income and marital satisfaction: Evidence from the national longitudinal survey of youth. J Obes Weight Loss 1: 001.
- Benson L, Mokhtari M (2011) Parental employment, shared parent–child activities and childhood obesity. J Fam Econ Iss 32: 233-244.
- Haslam DW, James WP (2005) Obesity. Lancet 366: 1197-1209.
Citation: Leyd LM, Carlson ER (2018) The Impact of Obesity on United States Health Care Expenditures. J Obes Weight Loss 3: 009.
Copyright: © 2018 Eric R Carlson, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.