ABSTRACT
Pilomatricoma is a benign neoplasm of the skin that originates in a hair follicle. Pilomatricoma is usually located on the head and neck, trunk, or upper and lower extremities and is most common during the first two decades of life. Pilomatricoma are slightly more common in women than men. The masses are usually asymptomatic and solitary, firm, mobile, dermal or subcutaneous nodules. Involvement of the dorsal trunk is uncommon, and pilomatricomas can be mistaken as other subcutaneous soft tissue lesions. Therefore, diagnostic imaging methods are useful for differential diagnosis. Here, we present an unusual case with MR imaging and pathologic findings of a dorsal trunk pilomatricoma in a 26-year-old woman.
KEYWORDS
Hair Follicle Tumor; Magnetic Resonance Imaging; Pilomatricoma
Introduction
Pilomatrixoma, also known as pilomatricoma or calcifying epithelioma of Malherbe, originates from the cells of the hair matrix. This tumor is an asymptomatic, slow-growing, benign dermal neoplasm [1]. The lesions are typically found in the head and neck (68.2%) and then the trunk (14.4%) and the upper (15.3%) and lower extremity (2%) [1]. These tumors are more common in the second decade of life (60-70%). A typical pilomatricoma is a hard, calcified dermal or subcutaneous nodule observed as a solid mass on Computed Tomography (CT) and Magnetic Resonance (MR) imaging [1]. Here, we present an unusual case with MR imaging and pathologic findings of a dorsal trunk pilomatricoma in a 26-year-old woman.
Case Report
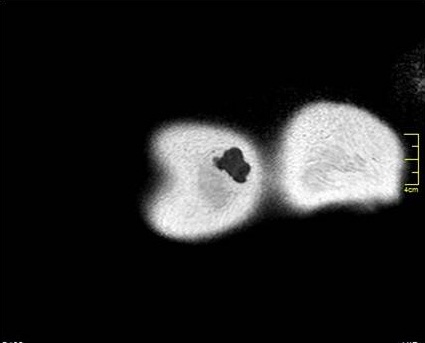
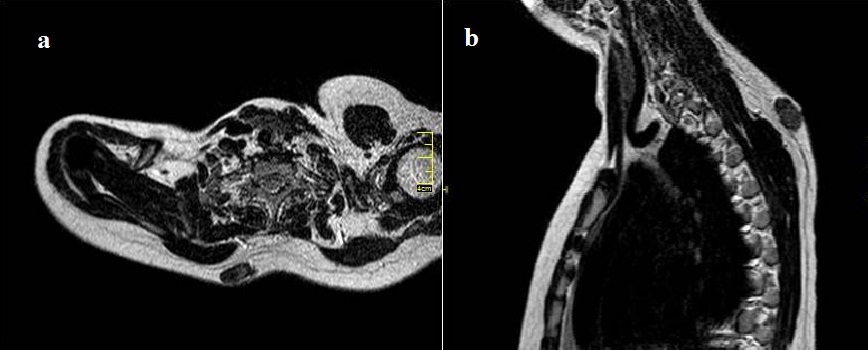
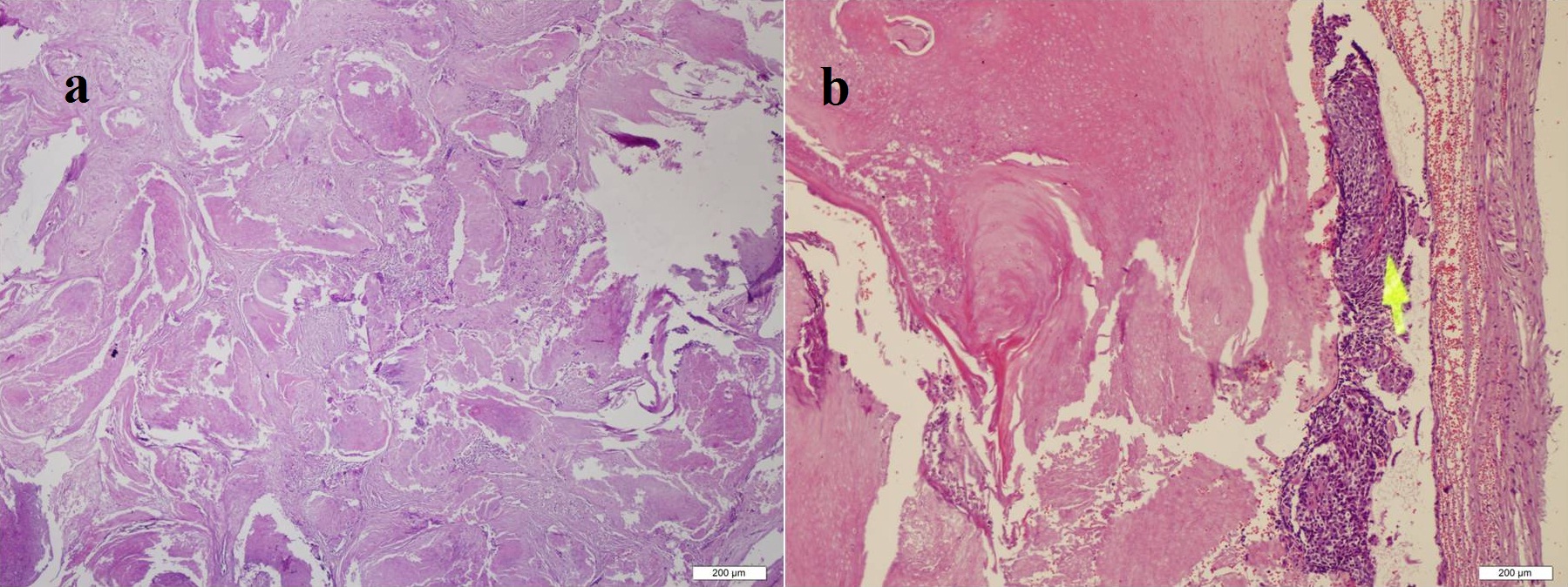
A 26-year-old woman presented with a 1-year history of soft tissue swelling and pain in her right dorsal trunk. Clinical examination revealed a solitary, firm, well-circumscribed mass located on the right dorsal trunk. In addition, the overlying skin showed bluish discoloration. There was no history of trauma or major surgery in this area. General physical examination and laboratory findings were normal. Direct radiography was normal. MR imaging showed a well-circumscribed hypointense lobulated mass in the right dorsal trunk on the axial T1 Weighted Image (WI) (Figure 1). On the axial T2WI (Figure 2a) and sagittal (Figure 2b), the mass was non-homogeneous and isointense to the muscle. There was no fat suppression within the mass. Primarily, the lesion was thought to be a benign mass. The lesion was completely excised under regional anesthesia and closed directly. The surgical specimen revealed a hard well-circumscribed mass, measuring 3x2x1 cm, and was yellowish-white (Figure 3). Histopathological examination of the pilomatricoma showed basaloid and shadow cells (Figure 4 (a,b)). There was no atypical cell or invasion of surrounding soft tissue. A final diagnosis of pilomatricoma was made histopathologically. There was no recurrence at follow-up 6 months later.
Discussion
A pilomatricoma is a superficial, firm, solitary, slow-growing, painless dermal or subcutaneous mass. It is often 0.5 to 3 cm diameter. The overlying skin normally has bluish discoloration. Pilomatricomas are slightly more common in women [2], and are frequently observed in children; 60% of cases are reported in the first two decades of life. The etiology is unknown. However, there are suggestions that an activating mutation in the β-catenin gene mapped chromosome 3p22-21.3 plays a major role in tumorigenesis [2]. A pilomatricoma is usually a solitary lesion, but multiple pilomatricomas are seen in several genetic disorders such as myotonic dystrophy, Gardner syndrome, xeroderma pigmentosum, and basal cell nevus syndrome [3].
Clinical diagnosis of a pilomatricoma is not easy. It can be confused with other dermal and subcutaneous lesions. Pilomatricoma has been described as a well-defined, hyperechoic, or isoechoic nodule with a hypoechoic rim and posterior acoustic shadowing on ultrasound. Hypoechoic rim depends on the connective tissue capsule, and calcification manifests as an echogenic focus with posterior shadowing [4]. Internal vascularization is observed in 50% of cases [5]. They are usually seen on CT as well-defined non-infiltrative calcified subcutaneous masses [6]. Lesions usually demonstrate isointense-signal intensity in the muscle on T1WI and inhomogeneous intermediate-signal intensity on T2WI with MR imaging [1]. In addition, Hsieh et al., [7] reported low signal intensity on T2WI can depend on keratin and calcification.
Inhomogeneous or peripheral rim enhancement can be seen after the injection of contrast. The enhancement pattern may vary depending on the components of the pilomatricoma [8]. Diffuse enhancement and peritumoral strands around the cystic tumor can be observed with MR imaging. MR imaging findings such as peritumoral edema or inflammation may reflect chronic inflammation with a foreign body reaction [8]. Cystic pilomatricomas demonstrated homogeneous low density without contrast enhancement on CT [9]. The appearance of a cystic lesion on CT or MR imaging could lead to the misdiagnosis of pilomatricoma as another benign cystic tumor, such as a dermoid or epidermoid cyst [9].
Pilomatricoma should be differentiating the painful tumors of the skin such as leiomyoma, eccrine spiradenoma, neuroma, dermatofibroma, angiolipoma, neurilemmoma, endometrioma, glomus tumor, and granular cell tumor [10]. Also, calcified lymph node, a hemangioma containing phlebolith, granuloma annulare and dermatofibrosarcoma should be distinguished from a pilomatricoma [8]. Some of these tumors can be reliably differentiated from the pilomatricoma with signal intensity characteristics. Granuloma annulare is a soft tissue mass without calcification. Lesions usually demonstrate low signal intensity on T1WI and T2WI and extensive diffuse enhancement following gadolinium administration. Anechoic vascular channels of hemangioma on ultrasound may be helpful in differential diagnosis [8]. Dermatofibrosarcoma protuberans typically originates from the dermis as a multinodular mass and then spreads into the subcutaneous tissues and muscle. The tumor appears as low signal intensity on T1WI and high signal intensity on T2WI. The tumor is also enhanced following the administration of contrast [11]. Thus, the lesion should be completely excised for a definitive diagnosis and should be examined histopathologically. Leiomyomas are benign soft tissue neoplasms that arise from smooth muscle. They can arise on any part of the body and can be found in the dermis, the subcutaneous fat or the deep fascia. MR findings of leiomyomas are slight hyperintensity to muscle on T1WI, mixed iso/hyperintensity to muscle on T2WI. Prominent enhancement was present after the intravenous injection of gadolinium [12]. Fibromas tend to show low signal intensity on all pulse sequences. Radiologic imaging is helpful in the differential diagnosis. But, histopathological examination should be performed for a definitive diagnosis.
The characteristic histological appearance of a pilomatricoma is a nest of small basaloid cells that undergo keratinization. Also, the most characteristic microscopic findings of the pilomatricoma are ghost or “shadow” cells. They have distinct cell borders, with eosinophilic cytoplasm and a central clearing, representing the outline of an absent nucleus. Commonly, there is an associated foreign-body multinucleated giant-cell reaction and fibrosis with calcification. Keratin debris, and central calcification are also characteristic. Calcification was detected in 70-85% of cases [3]. In our case, basaloid and shadow cells were seen by histopathological examination. These cells are characteristic for pilomatricoma. Also, atypical cells or invasion of surrounding soft tissue were not detected.
Although the clinical course is usually benign, malignant transformation has been reported in the literature [13-15]. The use of fine-needle aspiration biopsy in the diagnosis of pilomatricoma is still controversial. Based on a review of multiple case reports and series, Wang et al., reported that 45% of cases of pilomatrixoma were incorrectly diagnosed with fine needle aspiration cytology [16]. Nevertheless, the authors showed that fine needle aspiration is accurate when two key components, basaloid cells and ghost cells, are visualized, because these cells are specific for pilomatricoma [16]. Nonaggressive excision and curettage are sufficient treatment, because the cells do not regress spontaneously. Prognosis is excellent. Pilomatricoma generally has a low recurrence rate (0-3%). If a pilomatricoma recurs after excision or rapid growth, the mass should be evaluated with detailed histopathological analysis for malignant cells [3,6].
Conclusion
We present a case of pilomatricoma in the subcutaneous tissue of the dorsal trunk with MR imaging findings in a 26-year-old woman. The signal intensity of the pilomatricoma and the presence of calcifications could be helpful for a radiological differential diagnosis. Although a pilomatricoma is benign, malign transformations have been reported in the literature. Consequently, the tumor should be excised completely, and histopathological examination should be performed for a definitive diagnosis.
Figures
Figure 1: An axial T1-weighted Spin Echo (SE) Magnetic Resonance (MR) image (TR/TE: 18/647) shows a well-defined, lobulated soft-tissue mass confined to the subcutaneous soft tissues. The mass is isointense relative to the muscle on the unenhanced T1-weighted image.
Figure 2(a,b): An axial (a) and sagittal (b) T1-weighted SE MR images (TR/TE: 100/9230, TR/TE: 100/3607, respectively) reveal a non-homogenous soft tissue mass with signal intensity equal to that of muscle.
Figure 3: Gross specimen shows a well-circumscribed, yellowish-white mass containing calcifications, measuring 3x2x1 cm.
Figure 4(a,b): Histopathologic section shows characteristic features of a pilomatricoma, including (a) shadow and (b) basaloid cells (hematoxylin-eosin; original magnification, 40X).