ABSTRACT
Objectives
To compare the effectiveness of eccentric-concentric training of wrist extensors and eccentric-concentric training combined with supinator strengthening in healthy subjects.
Methods
A randomized clinical trial was carried out with 30 healthy subjects they were randomly allocated to two groups. Eccentric -concentric training of wrist extensors was given to group A (n=15). Group B (n=15) received eccentric-concentric training of wrist extensors combined with supinator strengthening. All subjects received five treatments per week for six weeks. Function was evaluated using grip strength at the end of the six-week course of treatment (week 6) and one month (week 10) after the end of treatment.
Results
There were no statistical differences between the two groups at the end of treatment and at the follow up.
Conclusion
Future well-designed studies are needed to confirm the results of the present trial in LET patients.
KEYWORDS
Eccentric-concentric; Grip strength; Lateral elbow tendinopathy; Supinator
Introduction
Lateral Elbow Tendinopathy (LET) seems to be the most appropriate term to use in clinical practice because all the other terms such as lateral epicondylitis, lateral epicondylalgia, lateral epicondylosis and tennis elbow make reference to inappropriate aetiological, anatomical and Pathophysiological terms [1]. LET is one of the most common lesions of the arm work-related or sport-related pain disorder. The condition is usually defined as a syndrome of pain in the area of the lateral epicondyle [2] that may be degenerative or failed healing tendon response rather than inflammatory [3]. Hence, the increased presence of fibroblasts, vascular hyperplasia, Proteoglycans and Glycosaminoglycans together with disorganized and immature collagen may all take place in the absence of inflammatory cells [4]. The most commonly affected structure is the origin of the Extensor Carpi Radialis Brevis (ECRB) [4]. The dominant arm is commonly affected, the peak prevalence.
The main complaint of patients with LET are pain and decreased function [2,3] both of which may affect daily activities. Diagnosis is simple, and a therapist should be able to reproduce this pain in at least one of three ways: (1) Digital palpation on the facet of the lateral epicondyle, (2) Resisted wrist extension and resisted middle-finger extension with the elbow in extension and (3) by getting the patient to grip an object [2,3,5].
Although the signs and symptoms of LET are clear and its diagnosis is easy, to date, no ideal treatment has emerged. Many clinicians advocate a conservative approach as the treatment of choice for LET [2,3,6-8]. Physiotherapy is a conservative treatment that is usually recommended for LET patients [2-9]. A wide array of physiotherapy treatments have been recommended for the management of LET [10-14]. These treatments have different theoretical mechanisms of action, but all have the same aim, to reduce pain and improve function. Such a variety of treatment options suggests that the optimal treatment strategy is not known and more research is needed to discover the most effective treatment in patients with LET.
One of the most common physiotherapy treatments for LET is an exercise programme [2-14]. One consisting of eccentric exercises has shown good clinical results in LET [15] as well as in conditions similar to LET in clinical behavior and histopathological appearance, such as Patellar and Achilles tendinopathy [16]. Such an exercise programme is used as the first treatment option for our patients with LET [9,17]. Malliaras and his colleagues concluded that clinicians should consider eccentric-concentric loading alongside or instead of eccentric loading in tendinopathy [16]. A pilot trial showed that an exercise program, consisting of isotonic strengthening, including eccentric, had reduced the pain in patients with rotator cuff tendinopathy at the end of the treatment and three months after the end of treatment [18].
Not only the wrist extensors and especially ECRB but also the supinator may be involved in LET [1]. The exercise program should include exercises not only for wrist extensors strengthening but also for supinator strengthening. Based mainly on clinical experience, supinator weakness is commonly addressed in LET patients as increasing pain, decreasing functional ability and hand - grip strength. To our knowledge, there have been no studies to investigate the effectiveness of supinator strengthening in the management of LET. It is possible to combine concentric-eccentric training of wrist extensors with strengthening of supinator to see if the combination of the above reported therapeutic approaches over’s superior results to eccentric - concentric training alone in LET patients. Therefore, the aim of the present article was to make a comparison of the ejects of an exercise programme consisting of eccentric - concentric training of wrist extensors with strengthening of supinator muscle exercises and an exercise programme consisting of eccentric - concentric training of wrist extensors alone for the treatment of LET.
Material and Methods
A randomized controlled, monocentre trial was conducted in the Cyprus Musculoskeletal and Sports Trauma Research Centre (CYMUSTREC) over 4 months to assess the effectiveness of an eccentric-concentric training of wrist extensors and an eccentric - concentric training of wrist extensors combined with strengthening of supinator. Two investigators were involved in the study: (1) a physiotherapist - lecturer (DS) who evaluated the subjects, performed all baseline and follow - up assessments, and gained informed consent and (2) a physiotherapist - M.Sc in sports physiotherapy student, the primary investigator (MT), who administered the treatments. All assessments were conducted by DS who was blind to the subjects’ therapy group. DS interviewed each subject to ascertain baseline demographic and clinical characteristics, including patient name, sex, age, duration of symptoms, previous treatment, occupation, affected arm and dominant arm.
Subjects between 18 and 45 years old (5) were examined and evaluated in the CYMUSTREC located in Nicosia/Cyprus (European University Cyprus) between January 2016 and April 2016. All subjects lived in Nicosia, Cyprus, were native speakers of Greek and were either self-referred or referred by their physician or physiotherapist.
The inclusion criteria of the study were (5):
1. No history of LET
2. No dysfunction in the shoulder, neck (radiculopathy) and/or thoracic region
3. No history of the fracture in the upper limb in the last 12 months
4. Athletes who did not use their upper limbs in their sport
Subjects were excluded from the study if they had one or more of the following conditions: (a) local or generalized arthritis; (b) neurological deficit; (c) radial, ulnar or median nerve entrapment; (d) limitations in arm functions; (e) the affected elbow had been operated on and (f) osteoarthritis in the wrist [5].
All subjects received a written explanation of the trial prior to entry into the study. All subjects gave signed informed consent to participate in the study. The study was approved by the Cyprus Bioethical Research Ethics Committee (ΕΤΑΒΚ ΕΠ 2016.01.11) and access to subjects was authorised by the manager of the CYMUSTREC (DS).
The subjects were randomly allocated to two groups by drawing lots. Subjects in group A were treated with eccentric - concentric training of wrist extensors and subjects in group B were treated with eccentric - concentric training of wrist extensors combined with supinator strengthening.
All subjects were instructed to use their arm during the course of the study but to avoid activities that irritated the elbow such as grasping, lifting, knitting, handwriting, driving a car and using a screwdriver. They were also told to refrain from taking anti-inflammatory drugs throughout the course of the study. Patient compliance with this request was monitored using a treatment diary.
Communication and interaction (verbal and non-verbal) between the therapist and subject was kept to a minimum, and behaviors sometimes used by therapists to facilitate positive treatment outcomes were purposefully avoided. For example, subjects were given no indication of the potentially beneficial effects of the treatments or any feedback on their performance in the pre-application and post-application measurements [19].
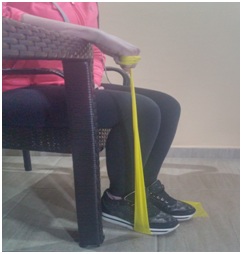
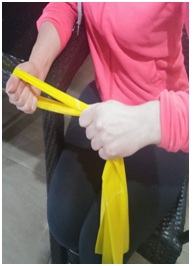
In the eccentric - concentric training group (Group A), eccentric - concentric exercises of the wrist extensors were performed in the non-dominant hand with the elbow on the bed in full extension, the forearm in pronation, the wrist in an extended position (as high as possible), and the hand hanging over the edge of the bed. From this position, patients flexed their wrist slowly (Figure 1) while counting to 15 (20 - 22) using chronometer, then returned to the starting position (extension). In the eccentric - concentric exercises of the wrist extensors combined with strengthening of supinator (Group B), eccentric - concentric training performed in the same way. Strengthening exercises of the supinator were performed in the non-dominant hand with the elbow on the bed in full extension, the forearm in pronation, the wrist in mid - position and the hand hanging over the edge of the bed. From this position, patients supinated their arm slowly (Figure 2) while counting to 15 (20 - 22) using chronometer, then returned to the starting position (pronation).
In both groups three sets of 15 repetitions of slow progressive exercises of the wrist extensors and supinator respectively, at each treatment session were performed, with 1-min rest interval between each set. Subjects were told to continue with the exercise even if they experienced mild pain. However, they were told to stop the exercise if the pain became disabling. The mild and disabling pain was monitored asking the subject to rate the pain on VAS before and after treatment. Mild pain was defined below 4 on VAS whereas disabling pain was defines above 8 on VAS [20-22]. When subjects were able to perform the exercises without experiencing any minor pain or discomfort, the load was increased using free weights.
All the above reported exercise programmes were given five times a week for 6 weeks and were individualized on the basis of the subject’s description of pain experienced during the procedure.
Function was measured in the present study. Each subject was evaluated at the baseline (week 0), at the end of treatment (week 6) and at 1 month (week 10) after the end of treatment. Function was measured by grip strength. Grip strength is defined as the amount of force each subject is able to generate with an isometric gripping action [19]. Force was measured in pounds with a Jamar hand dynamometer (Figure 3) that had adjustable handles to accommodate different hand sizes. The arm was placed in a standardized position of elbow extension, forearm pronation and internal rotation of the upper limb such that the palmar aspect of the hand faced posterior with the upper limb placed by the subject’s side. Subjects were then instructed to squeeze the dynamometer handles and then to release their grip [19]. The attained grip force was subsequently recorded, and the reading was not visible to the subject. Three measures of pain-free grip strength were recorded with a 30 seconds rest interval between each measurement, and the mean value of these repetitions was calculated. It is a valid and reliable outcome measure in LET patients.
The change from baseline was calculated for each follow - up. Differences between groups were determined using the independent test. The difference within groups between baseline and end of treatment was analyzed with a paired t test. A 5% level of probability was adopted as the level for statistical significance. SPSS V.21.00 statistical software was used for the statistical analysis.
Results
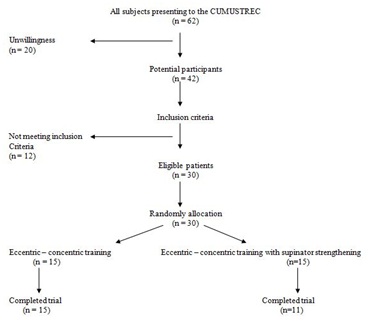
Sixty two subjects eligible for inclusion visited the CUMUSTREC with in the trial period. Twenty were unwilling to participate in the study, and 12 did not meet the inclusion criteria described above. The other 30 patients were randomly allocated to one of the two possible groups: (a) eccentric - concentric training of wrist extensors (n=15; 5 men, 10 women; mean (SD) age 28.06 (3.56) years); (b) eccentric - concentric training of the wrist extensors and supinator strengthening (n=15; 9 men, 6 women; mean (SD) age 29.53 (4.34) years). Subject flow through the trial is summarized in a CONSORT flow chart (Figure 4).
At baseline, there were more women in the groups (two more in total). The mean age of the subjects was less than 30 years. There were no significant differences in mean age (p>0.0005, independent t test) between the groups. All subjects were manual workers.
Baseline grip strength was 72.2 lb (95% CI 55.34 to 86.7) for the whole sample (n=30; Table 1). There were no significant differences between the groups for baseline pain-free grip strength (p>0.05 independent t test; Table 1). At week 6, there was a rise in pain - free grip strength of approximately 8 units in the group receiving eccentric - concentric training of wrist extensors and 10 units in the group receiving eccentric - concentric training of wrist extensors and supinator strengthening compared with the baseline (p<0.0005, paired t test; Table 2). There were no significant differences in the magnitude of improvement between the groups at weeks 6 and 10 (p<0.0005 independent t test; Table 2).
Discussion
The results obtained from this randomized clinical trial are novel, as to date there have been no data comparing the effectiveness of eccentric - concentric training of wrist extensors and an eccentric - concentric training combined with supinator strengthening in LET management. There were no statistical differences between the two groups at the end of treatment and at the follow up.
In LET not only the ECRB but also the supinator may be involved [1] the exercise program should include exercises not only for ECRB strengthening but also for supinator strengthening. Based mainly on clinical experience, supinator weakness in LET patients is commonly addressed as increasing pain, and decreasing functional ability and hand - grip strength. This means that the causes of LET may not be limited to the ECRB. Functional impingement of the supinator due to altered joint mechanism and muscle imbalance can impair the stabilization of the elbow resulting in overcompensation of the ECRB [23]. This may lead to micro trauma of the soft tissue structures present at the lateral epicondyle thus causing symptoms of LET. It is reasonable that enhancements with gripping might have happened from a blend of enhanced motor control and upgraded muscular power of the supinator [23]. Changes in the supinator may lead to altered and compensatory changes in the ECRB that may overload the ECRB during repetitive movements, thus causing symptoms of LET. Using supinator strengthening loading, usual motion might have been returned, resulting in resolution of pain with actions and a return to painless gripping for the patient [23].
A recently published trial assessed the effectiveness of eccentric training of wrist extensors and supinator strengthening in healthy subjects [24]. They found that the above combination produced a graded increase in surface electromyography activity in the healthy ECRB [24]. However, clinical studies are currently being conducted to determine if this approach is effective in the treatment of LET.
Alfredson et al., [25] were first proposed the eccentric training of the injured tendon. It is the most commonly used conservative approach in the treatment of tendinopathy. Malliaras and his colleagues [16] concluded that clinicians should consider eccentric - concentric loading alongside or instead of eccentric loading in Achilles and patellar tendinopathy. A Heavy Slow Resistance (HSR) program is recommended in the management of lower limb tendinopathy [26,27]. The HSR program was produced equivalent pain and function improvement (VISA) than the Alfredson eccentric program, but significantly better patient satisfaction at six month follow - up. In the Achilles tendon, eccentric and HSR have recently been shown to yield similar clinical outcomes (VISA and patient satisfaction) at 1 year follow up. Based on the above findings, the HSR program can be recommended as an alternative to the Alfredson eccentric program lower limb tendinopathy rehabilitation. Studies determining the effectiveness of such as exercises at other tendinopathies such as LET are needed.
Systematic review [15] and RCT [28] favor eccentric over other types of contractions in the management of LET, but Martinez - Silvestrini et al., [29] stated that, unlike Achilles tendinopathy, LET is often related to forceful grip activities requiring isometric contraction, which would be more beneficial than eccentric contraction in LET. LET is often related to forceful grip activities requiring isometric contraction of the wrist flexors and extensors [30]. Perhaps isometric contractions would be more beneficial than eccentric ones in lateral epicondylitis [30]. A case study showed that the combination of eccentric training with isometric contraction had positive effects in LET [31]. Recently, isometric exercises have been recommended to reduce and manage tendon pain increasing the strength at the angle of contraction without producing inflammatory signs [32]. Five repetitions of 45 - second isometric mid - range quadriceps exercise at 70% of maximal voluntary contraction have been shown to reduce patellar tendon pain for 45 minutes post exercise and this was also associated with a reduction in motor cortex inhibition of the quadriceps that was associated with patellar tendinopathy [33]. Therefore, it was hypothesized that the simultaneous use of these two kinds of contractions (isotonic and isometric) will further enhance the analgesic effect of contractions in the treatment of LET, increasing the arm function [34].
The load of exercises was increased according to the patients’ symptoms otherwise the results are poor [35]. Furthermore, eccentric exercises were performed at a low speed in every treatment session because this allows tissue healing [4]. Ice was recommended at the end of the treatment but research has shown that ice as a supplement to an eccentric exercise programme offers no benefit to patients with tendinopathy [20]. Finally, the avoidance of painful activities is crucial for tendon healing, because training during the treatment period increases patients’ symptoms and delays tendon healing [36].
Eccentric exercises appear to reduce the pain and improve function, reversing the pathology of LET [18,35-38] as supported by experimental studies on animals [39]. The way that eccentric training achieves the goals remains uncertain, as there is a lack of good quality evidence to confirm that physiological effects translate into clinically meaningful outcomes and vice versa. The clinical improvement of the HSR group was accompanied by increased collagen turnover. It is unknown if the isometric contractions can reverse the pathology of the tendinopathy and in this case the pathology of LET or reduce only the pain.
The exercise programme in both groups was carried out in home. Although a home exercise programme can be performed any time during the day without requiring supervision from a therapist, our clinical experience has shown that patients fail to comply with the regimen of home exercise programmes [20]. Although many ways can be recommended to improve the compliance of patients with the home exercise programme such as phone calls, exercise monitors and better self - management education, it is believed that this problem can be really solved by the supervised exercise programmes performed in a clinical setting under the supervision of a therapist. It is believed because our experience has shown that many patients stopped the home exercise programme without giving explanations, whereas patients completed the supervised programme. One possible reason why they continue the supervised exercise programme could be the cost. In the supervised exercise programme, the patients visit the therapist more times than the home exercise programme and this is more expensive. A future study will combine the both types of exercise programmes in order to maximize the compliance of the patients.
However, this trial does have some shortcomings. First, a power analysis was not performed. Second, no placebo (sham) or no treatment group was included in the present trial. The placebo (sham)/no treatment group are important when the absolute effectiveness of a treatment is determined. However, the absolute effectiveness of technique based interventions is difficult to investigate because a good and trustworthy placebo (sham)/no treatment control for exercise programmes appears to be difficult or impossible to devise, due in part to difficulties in defining the active element of these treatments. Absolute effectiveness also does not provide the therapists with information as to which is the most appropriate treatment for the management of a condition, in this case LET. Third, other activities treatments patients might be getting when not in the clinic were not monitored. Patients’ diaries suggested that patients were compliant to the study instructions, although patients may have given incorrect details to please the investigators. For example, it was possible that patients followed the treatment but took analgesic medications at the same time, and the improvement of symptoms may be due to those medications. Therefore, ways should be found to measure how other treatments such as analgesic medications contribute to the improvement of symptoms. Fourth, this study was conducted on healthy participants, and further studies recruiting people suffering with LE is required to determine whether the same graded increase exercise programme is found in the presence of a pathological tendon. Finally, the blinding of patients and therapists would be problematic in that case, if not impossible, because patients know if they are receiving the exercise programme treatment and therapists need to be aware of the treatment to administer it appropriately. In addition to the previous reported weaknesses, structural changes in the tendons related to the treatment intervention were not shown, and the intermediate and long-term effects (6 months or more after the end of treatment) of treatments were not investigated. Further research is needed to establish the possible mechanism of action of this treatment approach, and the cost - effectiveness of such treatment, because reduced cost is an important issue for the recommendation of any given treatment.
In conclusion, an eccentric - concentric training of wrist extensors combined with supinator strengthening did not improve the grip strength in healthy subjects. Future well - designed studies are needed to confirm the results of the present trial in LET patients.
Figures
Figure 1: Eccentric - concentric training of wrist extensors.
Figure 2: Supinator strengthening.
Figure 3: Hand grip dynamometer JAMAR.
Figure 4: Flow chart of the study.