Introduction
Osteoarthritis (OA) is the most common joint disease in adults around the world, it is a progressive disease resulting in chronic joint pain and significant disability [1,2]. The knee is one of the most frequently affected joints by OA [3]. According to Metcalfe, et al. 2013, more than 40% of people over 60 years of age have symptomatic knee OA, and more than 50% of these have bilateral knee OA [4]. In knee OA, the Medial Compartment (MC) is the most commonly distressed as during the stance phase of gait, more than 70% of the load applied to the knee joint passes through the MC, as the centre of mass passes through the medial to the centre of the knee joint [5]. In spite of being a common condition, the aetiology of knee OA is unclear. It is assumed to be a multifactorial disease, the result of a complex interplay of metabolic, genetic, biomechanical, and biochemical factors. OA is characterized by an increased local concentration of inflammatory cytokines, cartilage matrix degeneration and deposition of inappropriate sub-chondral bone [2,6]. Generally, the onset and evolution of knee OA has been linked to the mechanics of ambulation, consequently, there is a lot of literature suggesting that manipulating the biomechanical conditions around the knee joint during ambulation may have a significant influence on severity, progression and outcomes of the knee OA [7].
The objective of this review is to evaluate the relevant evidence-based biomechanical principles that may be applied for the management of knee OA (mainly the MC, as it is the most commonly affected). Different management options will be outlined with respect to biomechanical principles, and then the role of knee braces for the management of knee OA will be critically discussed from a biomechanical point of view.
Methods
A comprehensive search of the most relevant literature was conducted using the following keywords: knee osteoarthritis, biomechanics, conservative, brace, osteotomy and arthroplasty. The search was performed using the following search engines: Midline, Cochrane, Springer, ScienceDirect, google scholar and Web of Science. The search included papers published between 2005 and 2019. Only papers that discussed the biomechanical principles behind the management of primary uni-compartmental knee OA were included.
Results of Literature Review
Knee joint biomechanics and knee OA patho-mechanics
The knee joint alignment is one of the most commonly investigated factors when considering knee joint OA. Varus or valgus knee malalignment had been reported to influence the distribution of forces across the knee joint articular surface [8]. Varus malalignment of the knee is not uncommon in patients with medial compartment knee OA [9] and it increases the External Knee Adduction Moment (EKAM), leading to more compressive forces over the medial compartment of the knee [9,10]. It has been reported that medial knee compartment usually bears 60-80% of the load in people with neutral knee alignment, however a mild increase in knee joint varus alignment of around 4-5° can results in up to 20% increase in the compressive load over medial compartment [11]. Birmingham, et al. and Monil, et al., report that knee varus malalignment can create a vicious cycle, where increase knee medial compartment compressive load can result in accelerated medial compartment OA and subsequent worsening of the knee varus malalignment [9,12].
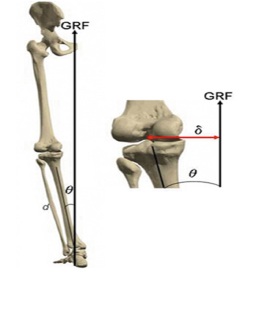
External Knee Adduction Moment (EKAM) (Figure 1) can be defined as the perpendicular distance between the Ground Reaction Force (GRF) and the centre of the knee joint, it is regarded as the relative load on the knee MC compared to the LC, which acts as a force pulling the knee in to the varus position [13,14].
Surgical management of knee OA
The surgical option depends on many factors, such as the patient’s age, symptoms, disability and radiographic severity of the disease. There are many surgical techniques used for the management of knee OA, for instance, arthroscopic debridement, arthroplasty and osteotomy. According to the American Academy of Orthopaedic Surgery recommendations, arthroscopic debridement should only be used for patients with mechanical symptoms, such as sudden onset joint locking or instability [6]. Knee Joint arthroplasty can be considered for patients with knee OA, either Uni-compartment Knee Arthroplasty (UKA) or Total Knee Arthroplasty (TKA) [15]. Corrective osteotomies are validated option for the management of knee joint OA when varus or valgus malalignment of the knee joint are considered as the causative factors [16]. The aim is to shift the mechanical axis of the knee from the arthritis compartment to the healthy one of the knee [16]. Voleti, et al., conducted a retrospective study to evaluate outcomes of varus distal femur osteotomy for the management of lateral knee OA associated with valgus knee malalignment. All of the 13 patients included in his study were able to commence sport activities at 11 months postoperatively, with a significant improvement in their functional outcomes [17]. However, small sample size is the main limitation of this study. On the other hand, based on the results of the systemic review conducted by Amendola and Bonasia 2010, good long-term results have been reported after High Tibial Osteotomy (HTO) for patients with MC knee OA [18].
Van Outeren, et al., discussed the results of 2 Randomised Controlled Trials (RCT) assessing the outcomes of HTO compared to conservative management of knee joint medial compartment OA. HTO provided better pain control, while, functional outcomes of HTO compared to unloader brace didn’t show a statistically significant difference [19].
Conservative management of knee OA
According to Zhang, et al., 2008, the optimal conservative management of patients with knee OA should include both pharmacological and non-pharmacological modalities [20]. The most commonly recommended pharmacological treatments are acetaminophen (paracetamol), followed by Non-steroidal Anti-inflammatory Drugs (NSAID) as a second line, and intra-articular corticosteroids [21]. Non-pharmacological management includes patients’ education, weight reduction, exercise and biomechanical intervention [22]. Exercises may reduce the symptoms of knee joint OA. As has been reported by Reeves and Bowling 2011, the effects of exercise on osteoarthritic knee biomechanics is through the production of Internal Abduction Moment (IAM) (produced by the hip abductor muscles and the lateral hamstring muscles), this IAM counteracts the EKAM [23]. Additionally, Thorstensson, et al., stated that the EKAM can be reduced after 8 weeks of exercise in middle age patients who presented early in the disease process [24]. Furthermore, the role of biomechanical interventions, in the management of knee OA is through modifying the EKAM around the knee joint [23]. For instance, lateral wedge insoles (valgus insoles) can be useful to relieve pain, improve function and to slow-down disease progression through modifying the EKAM around the knee joint with MC knee OA [25].
The role of braces in the management of knee OA
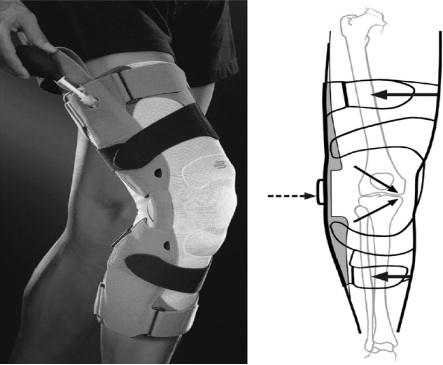
OA is an epidemic with no known, effective cure. A knee with OA will be further damaged if it is not protected physically [26]. Bracing (as shown in Figure 2) could be a useful, non-invasive measure to protect the uni-compartment knee joint OA. The aim of the brace is to reduce contact stress in the affected part of the joint, it could be useful for correcting mal-alignment and decreasing impairment associated with knee OA [13]. The efficacy of valgus knee braces and foot orthoses in the management of MC knee OA were assessed through the systemic review conducted by Raja and Dewan [27]. The results suggested that knee pain (as measured by the Visual Analogue Scale, VAS), analgesic consumption and knee stiffness were decreased significantly by using offloading knee braces and foot orthoses. In addition, knee braces and foot orthoses can improve balance and physical function scores (such as McMaster-Toronto Arthritis score and Knee injury and osteoarthritis outcome score for pain and functional status). As well as, it has been reported that the prolonged use of knee braces (6-12 months) may improve muscles proprioception and several biomechanical factors (such as moments around the knee joint). However, long-term effect of foot orthoses was not discussed clearly in the study. In fact, this review assessed a significant number of studies (25) with a significant overall sample size (more than 1100 patients with knee OA), and this can enhance the result accuracy significantly. Nevertheless, there were many limitations of this review. First, a wide range of age groups were included, for instance, some of the studies included patients in their thirties, whereas other studies only included patients in their seventies. Consequently, result accuracy may be affected, as OA is an age-related disease, and different age groups may have different disease activity rates and different responses to treatment. However, a wide range of age groups would be more representative of the normal population. Second, the studies assessed different types of braces and foot orthoses, which could cause the results to contain bias, because patients’ responses to braces or to foot orthoses may be directly affected by their design, and finally, only 6 Randomised Controlled Trials (RCT) were included, while the remaining studies were either a retrospective or a prospective cohort, with no control group or randomisation, and this may affect the results accuracy significantly.
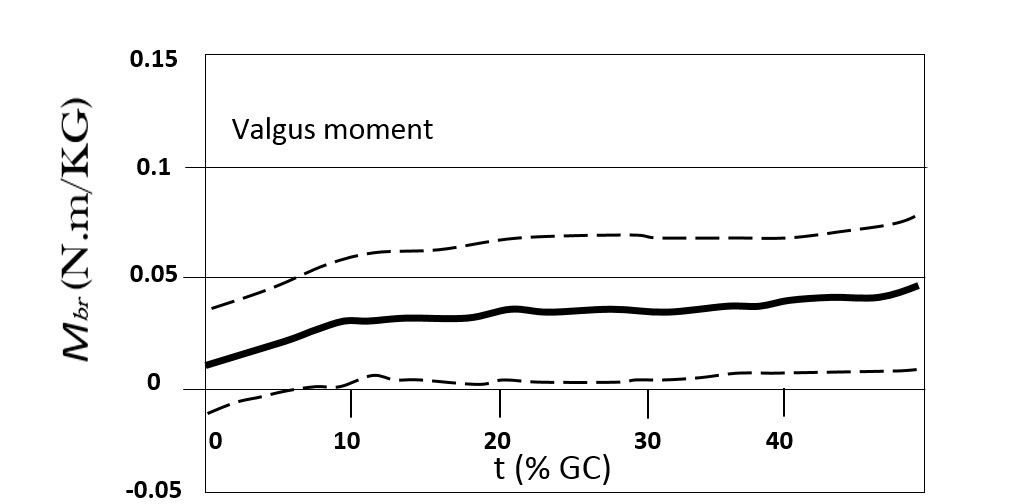
In addition, the biomechanical effects of valgus knee braces in MC knee OA were evaluated by Schmalz, et al., through performing gait analysis for 16 patients with MC knee OA after 4 weeks of wearing braces [29]. The results showed that the effect of moments created by the brace on the knee joint were as follows: the brace valgus moment (Mbr) was increased slightly during the early and late parts of the stance phase of the gait cycle, while it decreased in the mid stance phase (when knee flection occurs) as shown in figure 3. Additionally, the mean and maximum value of moment generated by the brace during the stance phase was equivalent to only 9 and 10 percent of the External Knee genu-varus (Adduction) Moment (EKAM), respectively (as illustrated in Table 1). This means that the knee brace did not affect the knee EKAM significantly, which leads to conclude that the actual effect of valgus knee braces is to compensate part of the external load, which is normally compensated by muscles and ligaments in an osteoarthritic knee without a brace, hence, decreasing the medial compartment load. This means that the real effect of braces regarding symptom relief could be due to its effect on relieving muscle tension and decreasing MC load. However, the small sample size limits the study’s reliability, as well as the fact that the participants’ gait was only assessed after 4 weeks of wearing the braces, and there was no baseline data of gait analysis to compare with; so, it is difficult to decide whether this result reflects the real effects of braces in patients with knee OA or it is inaccurate, as the patients’ symptoms had improved during the 4 weeks of wearing braces, due to decreased muscle spasms and improved overall joint biomechanics.
In fact, the results provided by Schmalz, et al. 201 [29] were supported by many other studies, such as the studies conducted by Kutzner, et al. 2011, Moyer, et al. 2015, and Pagani, et al. 2013 [30-32]. According to Kutzner, et al. 2011, the efficacy of two types of valgus knee braces on MC load in MC knee OA in three participants was assessed [30]. The results showed that the MC compression load could be reduced up to 25% with the application of knee braces. However, the small number of participants could affect the study’s external validity significantly. Furthermore, according to a systemic review and meta-analysis performed by Moyer, et al., 2014, it has been shown that there was evidence to suggest that knee braces can decrease the MC compressive force in knee joint OA [31]. It can change the medio-lateral distribution of force across the knee and increase the MC joint space, and amoderate to large, statistically significant improvement in EKAM during walking was recorded (P < 0.001), while, no change in alignment was reported. The main reported side effects of braces were slipping, patients discomfort and skin irritation. Importantly, a significant number of studies were included (30 studies) with a total number of patients equal to (478), and this can enhance this review external validity. Still, some of the limitations of this review are, firstly, 26 out of 30 included studies were either laboratory measurements on a single day or a retrospective cohort. So, there was no randomisation process or control group, which may decrease its internal validity. Secondly, a very wide-ranging age group of patients (21-85-years-old), although being more representative of the population, could cause significant bias, especially when assessing knee OA, as it is an age-related process and patients´ functional requirements could have varied markedly.
Additionally, Pagani, et al., through recording of Electromyography (EMG) activity for 12 patients with MC knee OA in three conditions: without a brace, with a neutral brace and with a valgus brace, reported that both the neutral and valgus knee braces can decrease muscle contraction and activation compared to the condition without braces [32]. So, it could be effective in decreasing MC load, which may reduce symptoms and decelerate disease progression. However, the small number of participants and the absence of previous baseline or long-term follow-up are limitations of the study. As a summary of the main findings of the studies above, it could be concluded that there is some evidence to suggest that knee braces can help to alleviate the symptoms of MC knee OA by decreasing the MC compressive load and muscle activation, however, the effects of braces on knee alignment and EKAM was limited.
The role of braces on long-term disease progression was reviewed by Steadman, et al., 2016 [33]. It was shown that even though there is clinical evidence to suggest that knee braces can improve symptoms of knee OA, biomechanical evidence may suggest that braces may not act effectively to hinder disease progression, although braces may be effective in decreasing MC compressive load significantly in patients with MC knee OA and it may affect EKAM; but, importantly, other parameters were not changed significantly. However, regardless of the fact that EKAM is strongly associated with knee OA progression, this moment does not directly cause knee OA alone. For instance, mal-alignment is a crucial factor in the progression of knee OA, and there was no evidence reporting a significant reduction in mal-alignment with knee braces.
Conclusion
In conclusion, knee OA is a common condition, with many conservative measures and surgical techniques used for its management. However, considering the effectiveness of knee braces in the management of MC knee OA from a biomechanical point of view, there is some evidence to suggest that knee braces can relieve pain and stiffness associated with MC knee OA. The mechanism that leads to symptom relief is thought to be acting by opposing some of the load and compression applied on the MC in patients with MC knee OA. This load is thought to be tolerated normally by muscles and tendons around the knee joint in case of no braces being applied; so, this extra load applied upon muscles may be important in the pain accompanied with knee OA. However, evidence showed that although knee braces could relieve symptoms and MC load in knee OA, it may not be effective in the reduction of disease progression, as the braces cannot change the whole biomechanical moment generated around the knee joint in OA, which means some moment will continue its effect on the knee joint after the braces have been applied. As a result, it may be difficult to assume that knee braces could be really effective on a long-term scale. However, the effects of knee braces may be useful to delay surgery in patients with knee OA. In fact, this particular point may need to be investigated more in the future.