ABSTRACT
Background Total Hip Arthroplasty (THA) for femoral neck fractures in the elderly is still lauded as one of the most successful surgeries of the century with good short and medium term outcomes. Postoperative dislocation remains the mainset back of hip replacement in the elderly. This study mainly sees keto assess early outcomes of total hiparthroplasty using dual mobility acetabular cup for femoral neckfractures in the elderly with emphasis on dislocation.
Patients and Methods We carried out 80 consecutive total hip replacements using a double articulating acetabular component. We assessed dislocation rates after 6 months and cumulative risks in the years following replacement.
Results After a mean follow-up of 50 months, only 8 (10%) deaths were recorded. We observed 1 case of dislocation at 4 months postoperatively that required revision arthroplasty. No case of instability was recorded.
Conclusion Dual mobility acetabular cups remain suitable implants in the face of postoperative dislocation after total hip replacement for femoral neck fractures in the elderly.
Keywords
Dislocation; Dual mobility cup; Femoral neck fracture
Introduction
Femoral neck fractures in the elderly are generally treated by partial or total hip replacement with early dislocation rates generally around 2-3% [1].The authors intend to demonstrate the efficacy of dual mobility cups for total hip replacement in the prevention of postoperative dislocation.
Patients and methods
We conducted a prospective study, comprising 80 consecutive dual mobility total hip replacements carried out at the Department of Trauma and Orthopedic Surgery A, from January 2010 to December 2017, for older patients with femoral neck fracture (Figure 1 and 2).
We included in this case series all patients who underwent primary THA for femoral neck fractures aged above 55 years. Thus we excluded all cases of neglected femoral neck fractures and cases associated with femoral shaft fractures.
54 women and 26 men, aged between 60 and 90 years with right side femoral neck fractures in 65% of cases were involved. 79% of the patients were autonomous with aided ambulation prior to injury. Parker score averaged 5/9. Average time between fracture and surgery was 3 days.
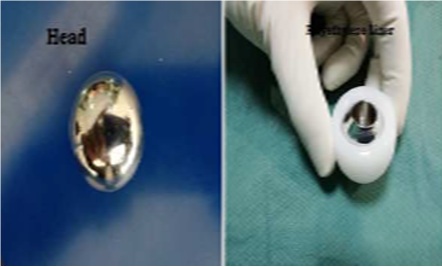
THA was done mostly under spinal anesthesia (n = 70 87.5%) with patient in a lateral decubitus position using a modified posterolateral Moore (Southern) approach in all cases.Dual mobility THA applying Charnley’s low friction torque principle using a 28 mm diameter head that articulates against polyethylene to decrease wear with a secondary larger diameter articulation between polyethylene liner and metal shell of acetabular component further enhancing implant stability (Figure 3 and 4) was carried out. Acetabular component was cemented in 75% of the cases.
Rehabilitation was commenced after the first postoperative day withfull weight bearing and braced ambulation. Patients were discharged on the third postoperative day with leaflets explaining prohibited maneuvers and physical therapy protocol.
Follow-up was carried out monthly up to 6 months and twice yearly afterwards with routine x-rays and physical exams. The Merle d'Aubigné and Postel hip score was used to assess outcomes after THA. We also assessed cumulative risks of dislocations in the years following replacement.
Results
80 patients predominantly women (sex ratio 2:1) were hospitalized for femoral neck fractures after standing fall in most cases (78%). Average time between injury and surgery was 3 days. 35 patients were diabetic, 60 patients were hypertensive whereas 17 patients had chronic renal failure on admission.The following table highlights radiographic outcomes after THA (Table 1).
After a mean follow-up of 50 months (between 12 and 65 months), we observed a single case of dislocation at 4 months postoperatively, following a fall that required open reduction (Figure 5). A single case of deep venous thrombosis of the lower limb was managed with heparin with favorable outcome. We recorded 8 (10%) deaths on the last follow-up. 5 cases were due to acute kidney failure, 3 due to congestive heart disease. No case of instability or atraumatic dislocation wasreported. No cases of acetabular or femoral implant loosening have been reported on postoperative radiography during this period.The Merle d’Aubigné and Postel score averaged 15.8 versus 7.2 preoperatively.
Discussion
Femoral neck fracture is a very common pathology of the elderly. Usually associated with osteoporosis, it mainly affects 70% of women above 80-years-old [2].
Choice of implant in primary hip replacement for femoral neck fractures remains a popular source of debate among orthopedic surgeons. Many often divided along the lines of either partial or total arthroplasty in what is a population with low life expectancy. Factors that may affect the stability after THA include surgical approach, patient-related factors like neurological disorders component orientation and geometry, and more particularly, head diameter and head-neck ratio [3].The use of low friction torque and dual mobility cups has gained popularity recently under several designations and descriptions including “unconstrained tripolar cups” and “mobile bearing cups” by manufacturers [4,5].
In our study postoperative mortality at 3 months was similar to rates reported by similar prospective studies of femoral neck fractures in the elderly. Skinner, et al., [6] observed that mortality rate was identical between partial and total arthroplasty for displaced femoral neck fractures in the elderly. Nonetheless some authors have reported dislocation rates up to 4 times higher in hemiarthroplasty after femoral neck fractures [7].
Dislocation rates following primary THA is estimated at 2.2% after one year, 3.8% at ten years, reaching up to 6% after 20 years [8]. A meta-analysis [9] observed an average dislocation rate of 10.7%, five times higher than primary replacement for degenerative osteoarthritis.Althoughcerebral palsy, Parkinson’s disease, poliomyelitis and history of cerebrovascular accident, spinal injury or Charcot arthropathy are risk factors for instability,early dislocation is directly linked to surgical approach and component positioning. Popular theory suggests a decrease in muscle control associated with ligamentous laxity following femoral neck fracturesin elderly patients [10]. Dual mobility cups have gained more interestin primary replacement for femoral neck fractures and revision arthroplasty as they exhibit less wear, restore near normal range of motion with increased implant stability [11, 12].
The concept of dual mobility was developed initially by Bousquet in the late 1970s. Its main purpose was to prevent dislocation by combining two articulating systems, one with a large diameter, between a metal cup and a polyethylene liner, and the other with a small diameter between the femoral head and its retentive insert. Generally, as rule of thumb the use of large diameter femoral head could address the problem of instability and mechanical studies have exhibited low dislocation rates with 28 mm femoral head components [13-15].This concept does not exhibit complications pertaining to simple implant retention, which solicits attachment through bony press fit, with less wear as the larger joint allowed additional range of motion during dislocation manoeuvers. Pituckanotai, et al., [16] in a recent network meta-analysis recommend dual mobility and big head as safer implants in THA with less risk of dislocation and revision.
Studies assessing survivorship of dual-articulation acetabular cup systems have reported good long-term results. The main drawback of hybrid primary THA remains aseptic loosening [17]. Tripolar prosthesis with a mobile cup and large-diameter heads are also deemed a reliable solution in highly unstable hips though the thickness of the polyethylene cup presents a considerable limitation which may affect long-term outcome due to a higher risk of wear [18]. A study by Tarasevicius [19] involving 42 patients who underwent dual mobility THA did not report any case of postoperative dislocation.
Conclusion
Surgical management of femoral neck fractures in the elderly by total hip arthroplasty has demonstrated excellent short term outcomes in terms of stable painless hip function. Dual mobility acetabular cups remain suitable implants in the face of postoperative dislocation after total hip replacement for femoral neck fractures.
List of abbreviations
THA: Total Hip Arthroplasty
Declarations
Ethics approval and consent to participate
Local ethics committee approval was sought before the publication of this article.
Consent to publish
Written informed consent was obtained from the patients involved in this case series for publication of this article and associated images.
Availability of data and materials
Not applicable.
Competing interests
The authors declare no potential conflicts of interest with respect to the authorship, and/or publication of this article.
Funding
Not applicable.
Author’s Contributions
All authors contributed either directly or indirectly in the writing and general format of the manuscript.
Figures
Figure 1: (A) preoperative X-ray showing a displaced femoral neck fracture in a 65 year old woman who underwent hybrid total hip arthroplasty using dual mobility cemented cup (B).
Figure 2: (A) 68 year old semi-autonomous man who suffered a right side Trans cervical fracture and underwent cement less total hip arthroplasty with dual mobility acetabular cup (B).
Figure 3: Hydroxy-apatite coated cup and metal head.
Figure 4: Head and polyethylene liner.
Figure 5: Hip x-ray showing dislocation on hip replacement (A) reduced after closed reduction (B).