ABSTRACT
The mediastinal disease is clinically diverse and can be manifested as cough, chest pain, and dyspnea, etc. CT is an imaging technique that can be used to diagnose mediastinal masses. Diagnosis can usually be confirmed by esophagoscopy, bronchial ultrasound guided mediastinal mass biopsy or percutaneous biopsy. Video-assisted thoracoscopic surgery can remove the mass for pathological diagnosis and play a therapeutic role. Mediastinal gastrointestinal cysts or duplication are relatively rare. Most of the reported cases are located in the posterior mediastinum. Here we present a case of gastrointestinal duplication with ectopic pancreatic mucinous cystadenoma in the anterior mediastinum involving pleural effusion.
Keywords
Anterior mediastinum; Ectopic pancreatic mucinous cystadenoma; Gastrointestinal duplication; Pleural effusion
Introduction
The anterior mediastinal mass usually includes thymoma, lymphoma, teratoma and thyroid mass. Here we report a case of gastrointestinal duplication with pancreatic mucinous cystadenoma presenting as large anterior mediastinal mass.
Case Presentation
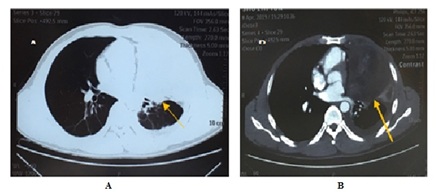
A previously healthy 42-year-old man was transferred to our hospital with complaints of mild cough, chest tightness. The patient developed cough, a small amount of white sputum with chest tightness before 2 months, no fever, chest pain, night sweats, weight loss, hemoptysis, and dyspnea. Tuberculosis antibodies and Antinuclear Antibodies (ANA) were negative Chest X-ray showed a large amount of pleural effusion on the left side. Closed drainage of left thoracic cavity was performed under local anesthesia. The routine examination of pleural effusion: The color was reddish and the clarity was turbid. Rivalta test was weakly positive. The biochemistry of pleural effusion: total protein 42.7g/L, Lactate Dehydrogenase (LDH) 369U/L, adenosine deaminase (ADA)11.6U/L, Alpha-fetoprotein(AFP) 5.68ng/ml, Carcinoembryonic Antigen (CEA) 40.9ng/ml, sugar chain antigen 125(CA125) 499.5U/ml, sugar chain antigen 19-9(CA19-9) 0.6U/ml. Computed Tomography (CT) of the thorax showed left hilar paraventricular space, considering the possibility of malignant lesions, mediastinal lymph node enlargement, left pleural effusion (after drainage) with left lower lobe part does not rise, right pleural thickening (Chest CT) (Figure 1). Left lung biopsy: Under the microscope, the acinus of varying sizes was seen in the loose interstitial. The acinar was lined with cubic or columnar epithelium, scattered in a small number of goblet cells, and some epithelium was mildly atypical, nucleus chromatin was deeply stained, the nucleolus was not clear, and the nuclear division was not seen. According to morphology results, (left lung) glandular epithelial adenomatous hyperplasia with mild atypical hyperplasia was considered. There was no significant change in weight in the near future. There is no special history in the past. The smoking history is 20 years and the smoking index is 600 years. He denied familial genetic diseases and infectious disease history.
Admission physical examination: T: 36.0°C, P: 80 beats/min, R: 18 beats/min, BP: 120/80 mmHg. The left lung breath sound was low, the right lung breath sound was clear. No dry-wet rales were heard in both lungs. There was no obvious abnormality in the heart and abdomen examination, and there was no edema in both lower limbs.
Admission laboratory tests revealed elevated erythrocyte sedimentation rate and plasma D-dimer.
Blood gas analysis: PH 7.402, oxygen partial pressure 65.1 mmHg, carbon dioxide partial pressure 41.2 mmHg. PET-CT showed a mixed density mass of 10.3 cm in the left upper lung, with punctate high density, slightly increased FDG uptake, SUVmax=3.6. The demarcation between the mass and the mediastinal pleura was not clear. There were slight cords in the left lung, insufficient left lower lung expansion, no ground glass or solid opacity in the right lung, and no abnormal FDG uptake focus. The left clavicular region, mediastinum and left hilum showed enlargement and abnormal uptake of lymph nodes. SUVmax=4.0. There was obvious effusion in the left thoracic cavity.
Conclusion: Low-grade malignant tumors of the left upper lung may involve the mediastinal pleura. Left clavicular region, mediastinum and left hilar lymph node metastasis. Left pulmonary insufficiency, old lesions of left lung, left pleural effusion. The pathology consultation opinion (left lung puncture tissue) is consistent with mucinous adenoma.
On April 30, 2019, the patient underwent thoracoscopic assisted thoracoscopic exploration and mediastinal lymph node biopsy under general anesthesia. During the operation, the left pleural cavity was extensively adhered, and the pale yellow effusion was seen in the thoracic cavity. The amount was about 500 ml, and no metastatic lesions were implanted. The lesion was located in the main pulmonary artery window and the enlarged lymph nodes were visible. The electric hook was used to open the mediastinal pleura. One lymph node was taken, and one pleural membrane was taken, and the diameter was about 1 cm. No tumor cells were seen in the frozen sections. A mass in the anterior mediastinum, about 8 cm in diameter, was hard, and the boundary with the surrounding tissue was unclear, invading the anterior segment of the right upper lung. The tumor was completely removed and sent to a frozen section to suggest a benign lesion.
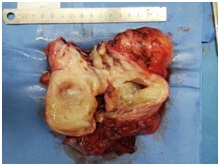
Postoperative pathology: gross- a mediastinal mass, size 11 × 6.5 × 9.5 cm, cut gray, solid, qualitative. Part of the cystic change, the inner wall of the capsule is smooth, the contents have been lost, see also the gray-white tissue 4 pieces, the total size is 5 × 4 × 1.8 cm, the cut surface is grayish white, solid, and medium. See also: a piece of lung tissue, size 7 × 4 × 2 cm, no clear mass on the cut surface (Figure 2).
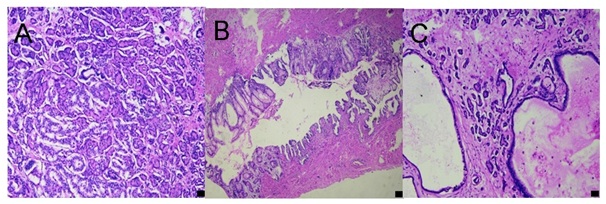
Microscopic examination: The mediastinal mass is cystic, and a large number of pancreatic tissue is seen in the cyst wall. The three structures of acinar, islet and duct are irregular, multi-focal distribution, and a small amount of small intestinal wall or pancreatic duct-like structure is seen, as well as intestinal mucosa, the rest of the wall tissue is fiber, smooth muscle, fat, blood vessels, etc. In the foci, the cystic ductal structure of the pancreas is adenoma-like hyperplasia, secretion is retained, and secretion spillovers in some areas and a large number of fibrous tissue hyperplasia and lymphocyte infiltration in the local (Figure 3).
The final pathological diagnosis: (mediastinal) consistent with gastrointestinal duplication, or gastrointestinal cysts, with ectopic pancreatic mucinous cystadenoma, and local secretions involving local lung surface, left pleural and chest wall tissue.
Hyperplastic fibrous tissue (Left pleura, chest wall nodules, lung tissue and lymph nodes) with hyaline degeneration, visible local calcification, chest wall nodules are hyperplastic fibrous tissue, of which a small number of ductal structures are seen; hilar lymph nodes (0/2); mediastinal lymph nodes (0/1); a small amount of lung tissue can be seen pleural thickening, fibrous tissue hyperplasia and focal lymphocytic infiltration.
The patient recovered well after operation. The thoracic duct was removed without fever, chest tightness and dyspnea. Chest CT was followed up regularly in outpatient clinic.
Discussion
Benign mediastinal cysts are usually congenital and form at 6th week of pregnancy, accounting for approximately 20% of primary mediastinal lesions, the most common is bronchiectasis (50-60%), and less common is the alimentary tract duplications (7-15%), which are usually located in posterior mediastinum [1]. Ectopic development of pancreatic tissue is developmental, and abnormalities are found in approximately 2% of autopsy [2]. 70-90% of this abnormality is located in the gastrointestinal tract [3].
Duplications of the gastrointestinal tract are rare congenitial cystic abnormalities and they share a common seromuscular coat and similar mucosal lining as the normal adjacent gastrointestinal tract [4]. Gastrointestinal duplication and pancreatic mucinous cystadenoma are rarely found to coexist in the mediastinal mass. In the case we have presented, mediastinal tumors are cystic and solid. They contain duplication of digestive tract and pancreatic cystadenoma and secrete mucus.
It has been reported that the incidence of gastrointestinal duplication is 1 in 4,500 [5], but the incidence of alimentary tract duplications in mediastinum has not been reported and may be less common. Gastrointestinal duplication in an adult is a rare entity because it is usually discovered in infants or children, they are cystic or tubular in shape, and clinical presentations are related to the location of the lesion and their components [6]. The etiology of gastrointestinal duplications is not clear. It may be related to embryonic development and environmental factors [4]. The patient we presented here was an adult patient with mediastinal mass and pleural effusion. Although the imaging results suggest a malignant possibility, serum CEA and CA19-9 are normal. The pathological findings of the resected mediastinal mass showed gastrointestinal duplication with ectopic pancreatic mucinous cystadenoma. No malignant cells were observed in histological pathology suggesting that the nature of the lesion is benign. Brugge et al. reported mucinous cysts with malignancy (including borderline malignancy) have higher values of CEA than benign mucinous, inflammatory and serous cysts [7]. However, in this case, we did not detect CEA and CA19-9 in the cyst fluid. If a similar case may be encountered in the future, the tumor markers in the cyst fluid can be tested for comparison with serum to help differential diagnosis. There were gastrointestinal and pancreatic tissues in the cyst wall of the resected mediastinum mass, including fibers, smooth muscle, fat, blood vessels. Localized calcifications was found in resected lung tissue, lymph node and left pleura. The walls of benign teratoma usually contain various mature tissues, including cartilage, pancreatic islet, and nerve tissues. Malignant mediastinal teratomas are characterized by the presence of various tissues such as embryonal structures [8]. So this case needs to be differentiated from teratoma. It has been reported that AFP serum levels are elevated in patients with mediastinal teratomas [9]. However, because AFP for pleural effusion 5.68 ng/ml was normal in the external hospital and we originally considered the possibility of lung cancer, we only detected tumor markers of lung cancer such as CEA and NSE, but did not detect AFP. In addition, immunohistochemical staining was not performed because of the benign findings of routine pathology.
We performed surgical treatment on this patient after completing relevant examinations and preoperative preparation. Operation was undertaken because of the possible complications of dyspnea, perforation, compression of adjacent organs and difficulty in differentiating the mass from a mediastinal malignancy. Bower et al. reported, of the 15 patients who underwent surgery for thoracic gastrointestinal duplication, 13 had no problem, but 2 had postoperative aspiration, 1 of which died [6]. Our patient recovered well after operation and is under follow-up.
Conclusion
Gastrointestinal duplications are rare congenital malformation that occur more often in early life, but some patients may show symptoms after adulthood. The pathogenesis is still unclear, and the symptoms depend on the type of pathology and the location of the lesion. The main treatment method is surgical resection. The case we presented was an alimentary tract duplication of the anterior mediastinum with ectopic pancreatic mucinous cystadenoma and the patient recovered well after surgical resection. Long-term prognosis needs to be confirmed by follow-up such as chest CT.
Acknowledgement
The authors would like to thank Xingye Chen and Professor Miaoxia He for providing pathological pictures.
Conflicts of interest
All authors declare no conflicts of interest associated with this manuscript.
Informed consent
Informed consent was obtained from the patient.
Funding
This work was supported by the grant from National Natural Science Foundation of China (grant number: 81670016).