
Hybrid Endovascular Repair for Dysphagia Lusoria in a Patient with Marfan Syndrome
*Corresponding Author(s):
Halim YammineDepartment Of Vascular Surgery, Atrium Health, Sanger Heart & Vascular Institute, North Carolina, United States
Tel:+1 6178346117,
Email:hyammine@gmail.com
Abstract
Objective
We present the case of a 51-year-old male with dysphagia lusoria and Marfan syndrome treated with a hybrid repair.
Methods
Review of chart and pre- and post-operative imaging was performed.
Results
The patient presented with a seven-year history of dysphagia with worsening symptoms including hoarseness. He had a prior aortic valve replacement and Bentall procedure, and no other significant comorbidities. Contrast CTA demonstrated an Aberrant Right Subclavian Artery (ARSA), with an area of focal dissection and aneurysmal degeneration measuring 26mm. The aorta measured 33mm proximally and distally, and the ARSA came off 15mm distal to the Left Subclavian Artery (LSA). An open right subclavian to carotid artery transposition was performed through a right neck incision. A 38mm×38mm×100mm proximal free flow Valiant™ device was used to cover the origin of the aberrant right subclavian artery. Completion arteriography and intravascular ultrasound were performed, demonstrating proximal and distal fixation with no evidence of endoleak or dissection.
The patient recovered well and was discharged on postoperative day three. At six weeks, he continued to recover uneventfully. CTA at three months demonstrated a stable repair. At one year, he has no complaints of chest or back pain and recently underwent a successful repair of an LSA aneurysm.
Conclusion
Aberrant right subclavian artery and Marfan syndrome are both rare conditions. When seen together, the treatment of this combined pathology can be challenging. A hybrid approach appears to be safe and effective for this clinical scenario.
Keywords
Hybrid Endovascular; Dysphagia Lusoria; Marfan Syndrome
INTRODUCTION
CASE REPORT
The patient underwent CTA with contrast that demonstrated an aberrant right subclavian artery with an area of focal dissection and aneurysmal degeneration measuring 26mm (Figures 1,2). The aorta measured 33mm both proximally and distally, and the right subclavian artery came off the aorta 15mm distal to a widely patent left subclavian artery. There was moderate dilatation of the left subclavian artery, and it was unclear whether it would be possible to clamp this both proximally and distally. Therefore, the right carotid artery was identified and an open right subclavian to carotid artery transposition was performed through a standard neck incision. Then, a 38mm×38mm×100mm proximal free flow Valiant™ (Medtronic Inc, Santa Rosa, CA) device was used to cover the origin of the aberrant right subclavian artery. Completion arteriography and intravascular ultrasound were performed, demonstrating excellent proximal and distal fixation with no evidence of endoleak or dissection. There was antegrade flow through both carotids as well as the left subclavian artery.

 Figure 2: Focal dissection of the aberrant right subclavian artery seen between esophagus and spinal column.
Figure 2: Focal dissection of the aberrant right subclavian artery seen between esophagus and spinal column.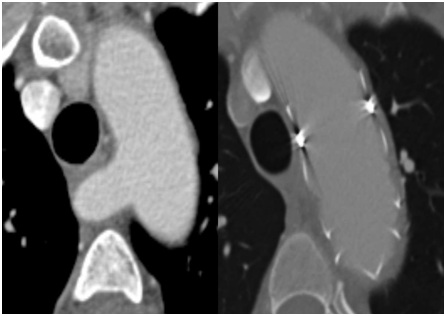 Figure 3: Comparison of pre-operative and post-TEVAR CTA showing successful repair.
Figure 3: Comparison of pre-operative and post-TEVAR CTA showing successful repair.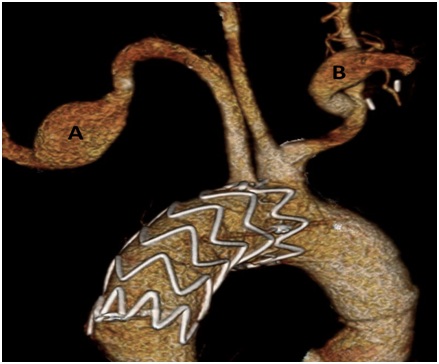 Figure 4: 3D CTA at 3 months post-TEVAR showing successful repair. A) LSA with dilatation, later repaired, B) Right subclavian to carotid artery transposition.
Figure 4: 3D CTA at 3 months post-TEVAR showing successful repair. A) LSA with dilatation, later repaired, B) Right subclavian to carotid artery transposition.DISCUSSION
Treatment is indicated to relieve dysphagia lusoria, as well as in cases where the ARSA is aneurismal [9]. Both open and endovascular approaches have been successfully performed and reported.[4,9] As TEVAR becomes more common, a variety of endovascular and hybrid techniques have been reported to treat ARSA [10-13]. A combined intervention with right subclavian artery transposition, distal or proximal artery ligation or endovascular occlusion, and TEVAR appears to be a promising endovascular solution for patients with ARSA [10]. Several hybrid procedures have been performed combining bilateral carotid-subclavian bypass with TEVAR, covering the origin of the ARSA [14-17]. Lacroix et al., also report successful TEVAR with a carotid-subclavian bypass and ARSA embolization to treat an aneurysmal ARSA [18]. Caution is necessary, however, when attempting endovascular occlusion of an aneurysmal ARSA, due to reports that proximal migration of a vascular plug deployed in an ARSA can cause recurrent dysphagia [19].
In particular, the use of an open right subclavian to right carotid artery transposition in conjunction with TEVAR in the presence of left subclavian artery dilatation is unique in this patient population. Mazzaccaro et al., echoed similar concern regarding a diseased left subclavian artery, and chose to use a periscope technique rather than a hybrid repair [13]. Multiple instances of successful right subclavian to right carotid bypass in conjunction with TEVAR for treatment of ARSA have been described [10,18]. We have also performed similar procedures with success in other patients with dysphagia lusoria at our institution. However, the positive outcome in this patient show that hybrid endovascular repair of ARSA is a viable option even with the added complexities in Marfan syndrome.
Endovascular treatment of the thoracic aorta in patients with Marfan syndrome is the subject of some controversy [20]. In general, it has been suggested that while TEVAR may be a life-saving option in emergency situations, it has a high rate of reintervention and risk of complications in patients with Marfan syndrome, and thus should be used as a bail-out or bridge procedure to open surgical treatment [21-26].
In terms of Marfan syndrome patients with ARSA, few cases have been described. LeRoux et al., describe the management of 22 patients with ARSA, including one patient with Marfan syndrome [5]. However, it is not clear what technique was used in this patient. Kamiya et al., described 8 patients with aneurysmal ARSA, one of which had Marfan syndrome and a chronic type B aortic dissection, and was treated with a staged repair including a carotid-subclavian bypass, closure of the ARSA, and replacement of the descending aorta [6]. To our knowledge, few Marfan syndrome patients have undergone the type of hybrid endovascular repair of ARSA described in most of the literature regarding the endovascular treatment of ARSA. One case, described by Stanley et al., in 2012, was complicated by a Kommerell diverticulum and acute dissection of an aneurysmal ARSA [7]. Our patient, who had minimal dilation of his ARSA and dysphagia lusoria, now provides another important example of a successful endovascular repair of ARSA in a patient with Marfan syndrome.
CONCLUSION
REFERENCES
- Natsis K, Didagelos M, Gkiouliava A, Lazaridis N, Vyzas V, et al. (2017) Erratum to: The aberrant right subclavian artery: Cadaveric study and literature review. Surg Radiol Anat 39: 1181-1182.
- Levitt B, Richter JE (2007) Dysphagia lusoria: A comprehensive review. Dis Esophagus 20: 455-460.
- Shennib H, Diethrich EB (2008) Novel approaches for the treatment of the aberrant right subclavian artery and its aneurysms. J Vasc Surg 47: 1066-1070.
- Austin EH, Wolfe WG (1985) Aneurysm of aberrant subclavian artery with a review of the literature. J Vasc Surg 2: 571-577.
- LeRoux E, Laurin C, Voisine P, Dumont E, Dagenais F (2017) Management of an aberrant subclavian artery during thoracic aortic surgery in the era of thoracic endografts. Canadian Journal of Cardiology 33: 89-90.
- Kamiya H, Knobloch K, Lotz J, Bog A, Lichtenberg A, et al. (2006) Surgical treatment of aberrant right subclavian artery (arteria lusoria) aneurysm using three different methods. Ann Thorac Surg 82: 187-190.
- Stanley GA, Arko FR, Foteh MI, Jessen ME, DiMaio JM (2012) Hybrid endovascular treatment of an anomalous right subclavian artery dissection in a patient with Marfan syndrome. Ann Thorac Surg 94: 639-641.
- Polguj M, Chrzanowski ?, Kasprzak JD, Stefa?czyk L, Topol M, et al. (2014) The aberrant right subclavian artery (arteria lusoria): The morphological and clinical aspects of one of the most important variations--a systematic study of 141 reports. Scientific World Journal 2014:292734.
- Stone WM, Ricotta JJ, Fowl RJ, Garg N, Bower TC, et al. (2011) Contemporary Management of Aberrant Right Subclavian Arteries. Ann Vasc Surg 25: 508-514.
- Kopp R, Wizgall I, Kreuzer E, Meimarakis G, Weidenhagen R, et al. (2007) Surgical and endovascular treatment of symptomatic aberrant right subclavian artery (arteria lusoria). Vascular 15: 84-91.
- van Bogerijen GH, Patel HJ, Eliason JL, Criado E, Williams DM, et al. (2015) Evolution in the Management of Aberrant Subclavian Arteries and Related Kommerell Diverticulum. Ann Thorac Surg 100: 47-53.
- Davidian M, Kee ST, Kato N, Semba CP, Razavi MK, et al. (1998) Aneurysm of an aberrant right subclavian artery: Treatment with PTFE covered stentgraft. J Vasc Surg 28: 335-339.
- Mazzaccaro D, Derosa TM, De Febis E, Righini P, Nano G (2016) Total endovascular repair of aberrant right subclavian artery aneurysm using the periscope technique: A case report. International journal of surgery case reports 29: 126-129.
- Corral JS, Zúñiga CG, Sánchez JB, Guaita JO, Basail AM, et al. (2003) Treatment of aberrant right subclavian artery aneurysm with endovascular exclusion and adjunctive surgical bypass. J Vasc Interv Radiol 14: 789-792.
- Attmann T, Brandt M, Müller-Hülsbeck S, Cremer J (2005) Two-stage surgical and endovascular treatment of an aneurysmal aberrant right subclavian (Lusoria) artery. Eur J Cardiothorac Surg 27: 1125-1127.
- Ferrero E, Ferri M, Viazzo A, Carbonatto P, Pecchio A, et al. (2011) Aneurysm of the aberrant right subclavian artery: Surgical and hybrid repair of two cases in a single center. Ann Vasc Surg 25: 839.
- Hoo AJS, Rokkas CK, Rossi PJ (2017) Distal migration of a vascular occlusion plug in an aberrant right subclavian artery resulting in recurrent dysphagia following use in repair of dysphagia lusoria. Journal of Vascular Surgery 66: 40.
- Lacroix V, Astarci P, Philippe D, Goffette P, Hammer F, et al. (2003) Endovascular treatment of an aneurysmal aberrant right subclavian artery. J Endovasc Ther 10: 190-194.
- Kedora J, Grimsley B, Pearl G (2009) Endovascular treatment of an aberrant right subclavian artery aneurysm with use of the Zenith iliac plug. Proc (Bayl Univ Med Cent) 22: 144-145.
- Cooper DG, Walsh SR, Sadat U, Hayes PD, Boyle JR (2009) Treating the thoracic aorta in Marfan syndrome: Surgery or TEVAR? J Endovasc Ther 16: 60-70.
- Ince H, Rehders TC, Petzsch M, Kische S, Nienaber CA (2005) Stent-grafts in patients with Marfan syndrome. J Endovasc Ther 12: 82-88.
- Gagné-Loranger M, Voisine P, Dagenais F (2016) Should endovascular therapy be considered for patients with connective tissue disorder? Can J Cardiol 32: 1-3.
- Geisbüsch P, Kotelis D, von Tengg-Kobligk H, Hyhlik-Dürr A, Allenberg JR, et al. (2008) Thoracic aortic endografting in patients with connective tissue diseases. J Endovasc Ther 15: 144-149.
- Waterman AL, Feezor RJ, Lee WA, Hess PJ, Beaver TM, et al. (2012) Endovascular treatment of acute and chronic aortic pathology in patients with Marfan syndrome. J Vasc Surg 55: 1234-1241.
- Dong ZH, Guo Fu W, Wang YQ, Guo Da Qiao Xu X, et al. (2009) Retrograde type A aortic dissection after endovascular stent graft placement for treatment of type B dissection. Circulation 119: 735-741.
- Dardik A, Krosnick T, Perler BA, Roseborough GS, Williams GM (2002) Durability of thoracoabdominal aortic aneurysm repair in patients with connective tissue disorders. Journal J Vasc Surg 36: 696-703.
Citation: Calarese AW, Yammine H, Ballast JK, Arko FR (2019) Hybrid Endovascular Repair for Dysphagia Lusoria in a Patient with Marfan Syndrome. J Surg Curr Trend Innov S1: 005.
Copyright: © 2019 Adam W Calarese, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

