Contribution of Three-Dimensional Reconstructions from CT-Scan for Assessing the Factors Associated with Blunt Splenic Injury Severity
*Corresponding Author(s):
Anne-Sophie StuderDepartment Of General And Digestive Surgery, North Hospital, Aix-Marseille University, Marseille, France
Tel:+33 0491968170,
Email:annesophiestuder@yahoo.fr
Abstract
Purpose
Analysis of influence of anthropomorphometry, splenic variability and crash’s circumstances on the severity of splenic injury.
Methods
Seventy-seven patients with blunt splenic trauma had a tomodensitometry at time of admission. Localisation, type, and lesion’s severity (AAST classification), were determined. Severe splenic lesion was defined by: Grade 4 or 5, lesion of entire parenchyma, or fracture. Three-dimensional splenic segmentation allowed calculation of volume, orientation (colatitude and azimuth), morphometry, morphology and span of hilar vessels. Anthropometric parameters were: Age, gender, BMI, and morphotype. Relationships between spleen, stomach, liver and 10th left rib were detailed.
Results
In univariate analysis, splenic parameters for a severer lesion were: Orientation of hilar side turned towards vertebral column (azimuth, p=0.05), spread conformation of hilar vessels (p=0.10), and high splenic volume (p=0.06). The younger the patient, the more severe was the splenic lesion (p=0.07). A full stomach and a left liver overflowing in the left hypochondrium, were associated with low gravity splenic lesion, (p=0.02 and p=0.03). In multivariable analysis, injured patients whose hilar area was vertically oriented, were more at risk of severe splenic lesion (OR=0.92, 95% CI (0.85-0.99), p=0.02). An abdominal-shaped liver was associated with low gravity splenic lesion (OR= 0.13, 95% CI (0.02-0.93), p=0.04).
Conclusions
Topographic and morphologic variability of the spleen condition its vulnerability in trauma cases. Using this analysis and the biomechanical behaviour of splenic tissue will allow for the creation of a splenic numerical model, and its integration in the virtual human scientific application of modern traumatology.
Keywords
INTRODUCTION
Background
Nevertheless, a failure of non-operative management can occur in almost 10-15% of cases [8]. The severity of the splenic injury, defined by the American Association for the Surgery of Trauma (AAST) [9], is the most accurate predictive factor for failure of non-operative management, both in the early phase but also during the monitoring period.
Although clinical management of blunt splenic trauma is fairly well codified, relatively little is known about the process leading to splenic injury. Only a few studies have explored the biomechanics of the spleen [10-13]. Currently, there is no experimental or numerical model reproducing blunt traumatic splenic injury. Such models could ultimately help to better understand the circumstances, and patients at risk, of severe splenic injury [14]. One explanation for this lack of splenic lesion model could be the high complexity of this type of trauma, and the high variability of the splenic anatomy could be another. The variability of spleen morphometry (mostly spleen volume) has already been investigated by numerous anatomical and radiological studies [15,16]. Very little is known however on the three-dimensional anatomy of the spleen (morphology, spatial orientation, anatomical relationships).
In a previous work, we described the three-dimensional anatomy of the spleen using a CT-scanner in non traumatized patients [16]. The aim of the present study was to evaluate the three-dimensional splenic anatomy in traumatized patients and the potential effect of this three-dimensional anatomy on injury severity.
MATERIAL AND METHODS
Study population
Circumstances of the accident
Tomodensitometric analysis of the splenic lesion and splenic three-dimensional reconstruction
 Figure 1: Localisation of the lesion (Hilar surface): (P) Posterior localisation, (A) Anterior localisation, (S) Superior localisation, (I) Inferior localisation.
Figure 1: Localisation of the lesion (Hilar surface): (P) Posterior localisation, (A) Anterior localisation, (S) Superior localisation, (I) Inferior localisation.Lesion severity was graded according to the AAST classification [9]. The type of splenic lesion was detailed as contusion, laceration, subscapular hematoma, intra-parenchymatous hematoma, fracture or burst fracture. A severe splenic lesion was defined by the presence of one of the following anomalies: AAST grade 4 or 5, lesion of the entire parenchyma, lesion corresponding to a fracture or burst fracture. Segmentation and 3D reconstruction of the spleen were done with Mimics 10.01 software (Materialise Software, Belgium). We also segmented both of the 10th ribs, and the 11th thoracic vertebral body, which served as points of reference for spatial localisation of the spleen (Figure 2) [16].
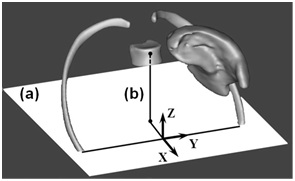 Figure 2: Segmentation of the spleen16, both 10th ribs, 11th thoracic vertebral body, and spatial orientation of the hilar surface: (a) Plane containing the axis of the 10th rib tips, (b) Projection of the centre of the vertebral body of the 11th thoracic vertebra.
Figure 2: Segmentation of the spleen16, both 10th ribs, 11th thoracic vertebral body, and spatial orientation of the hilar surface: (a) Plane containing the axis of the 10th rib tips, (b) Projection of the centre of the vertebral body of the 11th thoracic vertebra.The exact methodology of this three-dimensional reconstruction has been described in a previous publication [16]. This method enabled us to determine splenic volume, morphology, morphometry, orientation, splenic volume boundless rate under the 10th rib, and the span of the hilar vessels. This last parameter was defined as the distance ratio between the highest and the lowest arterial entry points for the total span of the parenchyma, on either side of these entry points. The median was then used to classify the hilum in the grouped type (>0.52) or in the spread type (<0.52). Segmentation enabled us to calculate the spleen’s orientation in space, using angle measurements (colatitude and azimuth), and to determine its horizontal axis using the longest axis 91 of the frontal section. It also allowed for an appreciation of the morphometric organisation of the parenchyma, whether it was dorsal or abdominal in shape and which of the three possible morphologies: Coiled, cupped or flat [16].
Anthropometry of the study population
Analysis of the relationship between intra-abdominal organs
Having divided the left hypochondrium into four parts, we characterized the development of the left hepatic lobe by the number of quarters occupied. The stomach was described according to its empty or full status. The presence of a fracture of the 10th left rib was investigated.
Statistical analysis
RESULTS
Population data and splenic injury
|
Demographic characteristics |
n= 77 |
|
Mean age (years) |
32 ±15.2 |
|
Gender M/F |
59 (76.6%) /18 (23.4%) |
|
Individual Anthropometry |
|
|
General morphotype |
|
|
Stocky |
28 (36.4%) |
|
Slender |
49 (63.6%) |
|
Abdominal perimeter (mm) |
838.7 ±121.4 |
|
BMI (Kg/Cm2) |
|
|
Normal |
58 (75.3%) |
|
Overweight |
9 (11.7%) |
|
Obesity |
5 (6.5%) |
|
Severe obesity |
2 (2.6%) |
|
Malnutrition |
3 (3.9%) |
|
Accident circumstances |
|
|
Pedestrian |
3 (3.9%) |
|
Two-Wheelers |
34 (44.2%) |
|
Truck and light vehicles |
40 (51.9%) |
|
Position during the impact |
|
|
Driver |
47 (61%) |
|
Front passenger |
4 (5.2%) |
|
Passenger back left / back right / back middle |
4(5.2%)/1(1.3%)/2(2.6%) |
|
Direction of the impact |
|
|
Lateral right / Lateral left |
3 (3.9%)/ 8 (10.4%) |
|
Frontal |
38 (49.4%) |
|
Back |
2 (2.6%) |
|
Gravity of the accident |
|
|
Ejection outside the vehicle |
11 (14.3) |
|
Extrication outside the vehicle more than 20 minutes |
16 (20.8%) |
|
Rolled over |
3 (3.9%) |
|
System of protection |
|
|
None |
13 (16.9%) |
|
Seat belt |
20 (26%) |
|
Helmet |
25 (32.5%) |
|
Airbag |
19 (24.6%) |
|
Morphometric analysis of the spleen and neighbouring organs |
|
|
Splenic characteristics |
|
|
Splenic volume (cc) |
233.2±119.5 |
|
Splenic morphometry |
|
|
Abdominal-shape |
41 (53.3%) |
|
Dorsal-shape |
36 (46.7%) |
|
Angle between horizontal and biggest axis of the spleen (°) |
50.5±12.6 |
|
Splenic morphology |
|
|
Flat |
13(16.9%) |
|
Cupped |
57(74%) |
|
Coiled |
7(9.1%) |
|
Percentage of splenic volume under the 10th left rib |
|
|
0% |
5 (6.5%) |
|
Less than 20% |
18 (23.4%) |
|
20 - 50% |
30 (38.9%) |
|
More than 50% |
24 (31.2%) |
|
Orientation in space |
|
|
Colatitude (°) |
80±20.7 |
|
Azimuth (°) |
118.6±29 |
|
Conformation of hilar vessels |
|
|
Spread |
37 (48.1%) |
|
Grouped |
40 (51.9%) |
|
Neighbouring organs |
|
|
Occupation of the left hypochondrium by the left liver |
|
|
01/4 |
26 (33.8%) |
|
01/2 |
28 (36.4%) |
|
03/4 |
15 (19.5%) |
|
04/4 |
8 (10.3%) |
|
Hepatic morphometry |
|
|
Abdominal-shape |
47 (61%) |
|
Dorsal-shape |
30 (39%) |
|
Fracture of the left 10th rib |
|
|
Stomach |
|
|
Full |
33 (42.9%) |
|
Empty |
25 (32.5%) |
|
Analysis of the splenic lesion |
|
|
Splenic lesion: AAST Grade: |
|
|
1 |
31 (40.3%) |
|
2 |
24 (31.2%) |
|
3 |
14 (18.2%) |
|
4 |
8 (10.3%) |
|
5* |
0 (0%) |
|
Localisation of the lesion |
|
|
Hilar |
35 (45.5%) |
|
Lateral |
15 (19.5%) |
|
Lateral and hilar |
23 (29.8%) |
|
Splenic tip |
4 (5.2%) |
|
Type of lesion |
|
|
Contusion |
2 (2.6%) |
|
Intra-parenchymatous hematoma |
12 (15.5%) |
|
Sub-capsular hematoma |
10 (13%) |
|
Laceration |
27 (35.1%) |
|
Fracture |
23 (29.9%) |
|
Burst |
3 (3.9%) |
Table 1: Descriptive parameters of the study population (Quantitative variables are in mean±299 standard deviation).
* No grade 5 in the 77 splenic traumas. 18 / 95 splenic trauma had a splenectomy for haemostasis before going through tomodensitometry.
Univariate analysis (Table 2)
|
Parameters |
Low severity splenic |
High severity splenic |
p |
|
Lesion |
Lesion |
||
|
Mean age (years) |
40±16.3 |
24±6.8 |
0.07 |
|
Gender M/F |
52 (75.3%)/17 (24.7%) |
7 (87.5%)/1 (12.5%) |
0.44 |
|
Individual Anthropometry |
|||
|
General morphotype |
|
|
0.45 |
|
Stocky |
25 (36.2%) |
3 (37.5%) |
|
|
Slender |
44 (63.8%) |
5 (62.5%) |
|
|
BMI (Kg/Cm2) |
|
|
0.57 |
|
Normal |
58 (84%) |
0 (0%) |
|
|
Overweight |
7 (10.1%) |
2 (25%) |
|
|
Obesity |
4 (5.7%) |
1 (12.5%) |
|
|
Severe obesity |
2 (2.9%) |
0 (0%) |
|
|
Malnutrition |
3 (4.3%) |
0 (0%) |
|
|
Accident circumstances |
|||
|
Type of transport |
|
|
0.2 |
|
Pedestrian |
2 (2.9%) |
1(12.5%) |
|
|
Two-Wheelers |
31 (44.9%) |
3 (37.5%) |
|
|
Truck and light vehicles |
36 (52.2%) |
4 (50%) |
|
|
Position during the impact |
|
|
0.39 |
|
Driver |
40 (60.6%) |
7 (87.5%) |
|
|
Front passenger |
3(4.3%) |
1 (12.5%) |
|
|
Direction of the impact |
|
|
0.44 |
|
Lateral right |
2 (2.9%) |
5 (62.5%) |
|
|
Frontal |
33 (47.8%) |
2 (25%) |
|
|
Unknown |
24 (34.8%) |
1 (12,5%) |
|
|
Gravity of the accident |
|
|
0.07 |
|
Extrication outside the vehicle more than 20 |
|
|
|
|
minutes |
13 (18.8%) |
3 (37,5%) |
|
|
Unknown |
39 (56.5%) |
5 (62.5%) |
|
|
System of protection |
|
|
0.49 |
|
None |
9 (13%) |
4 (50%) |
|
|
Seat belt |
19 (27.5%) |
1 (12.5%) |
|
|
Helmet |
23 (33.3%) |
2 (25%) |
|
|
Airbag |
18 (26%) |
1 (12.5%) |
|
|
Splenic characteristics |
|||
|
Mean Splenic volume (cc): |
233±119.7 |
233±145.1 |
0.06 |
|
Splenic morphometry: |
|
|
0.85 |
|
Abdominal-shape |
37(53.6%) |
4 (50%) |
|
|
Dorsal-shape |
32 (46.4%) |
4 (50%) |
|
|
Splenic morphology: |
|
|
0.2 |
|
Flat |
10 (14.5%) |
3 (37.5%) |
|
|
Cupped |
52 (75.4%) |
5 (62.5%) |
|
|
Coiled |
7 (10.1%) |
0 (0%) |
|
|
Percentage of splenic volume under the 10th left rib |
|||
|
0% |
2 (2.9%) |
3 (37.5%) |
|
|
Less than 20% |
16 (23.2%) |
2 (25%) |
|
|
20-50% |
29 (42%) |
1 (12.5%) |
|
|
More than 50% |
22 (31.9%) |
2 (25%) |
|
|
Orientation in space (Mean) |
|||
|
Colatitude (°) |
93.2±20.4 |
66.8±24.4 |
0.19 |
|
Azimuth (°) |
123,1±28.8 |
114.1±29.6 |
0.05 |
|
Conformation of hilar vessels |
|
|
0.11 |
|
Spread |
32 (46.4%) |
5 (62.5%) |
|
|
Grouped |
37 (63.6%) |
3 (37.5%) |
|
|
Neighbouring organs |
|||
|
Occupation of the left hypochondrium by the left liver |
|
|
0.48 |
|
1/4 |
22 (31.9%) |
4 (50%) |
|
|
1/2 |
24(34.8%) |
4 (50%) |
|
|
3/4 |
15 (21.7%) |
0 (0%) |
|
|
4/4 |
8 (11.6%) |
0 (0%) |
|
|
Hepatic morphometry |
|
|
0.03 |
|
Abdominal-shape |
46 (66.7%) |
1 (12.5%) |
|
|
Dorsal-shape |
23 (33.3%) |
7 (87.5%) |
|
|
Fracture of the left 10th rib |
7(10.1%) |
0(0%) |
0.35 |
|
Stomach |
|
|
0.02 |
|
Full |
30(43.5%) |
3(37.5%) |
|
|
Empty |
20(29%) |
5(62.5%) |
|
|
Almost empty |
19 (27.5%) |
0 (0%) |
|
Table 2: Significant parameters in univariate analysis, associated with a more severe splenic lesion (p<10%).
There were four splenic parameters for more severe lesions: The hilar side was oriented toward the vertebral column (determined by the azimuth measure, p=0.05), a spread conformation of the hilar vessels (p=0.10), a recovery of the spleen by the 10th left rib (p=0.08) and a high splenic volume (p=0.06). Neither the morphometry nor the morphology of the spleen was linked to the severity of the splenic lesion (respectively p=0.85 and p= 0.2) and anthropometric parameters did not seem to influence the seriousness of injury. Obesity did not appear to be an aggravating or protecting argument for splenic trauma (p=0.62). Younger patients suffered severe splenic lesions most frequently (p=0.07) and gender was not a significant factor (p=0.44). As for the circumstances of the accident, none of the situations recorded seemed to influence the severity of the splenic lesion. The use of a seat belt or the airbag setting didn’t seem to aggravate or protect from high splenic trauma (p=0.49). As to the relationship between intra-abdominal organs, a left liver overflowing in the left hypochondrium and covering the upper part of the spleen was associated with a low severity splenic lesion (p=0.03), whereas an empty stomach was associated with more severe splenic lesions (p=0.02).
Multivariable analysis
 Figure 3: Segmentation of the spleen, the 10th left rib and the 11th thoracic vertebrae (Anterior View). The hilar surface is more verticalized and turns towards the vertebral column.
Figure 3: Segmentation of the spleen, the 10th left rib and the 11th thoracic vertebrae (Anterior View). The hilar surface is more verticalized and turns towards the vertebral column.DISCUSSION
The splenic organ varies widely between individuals in terms of anatomic characteristics, morphology, geometry, orientation in space and vascularisation [16]. In this study, we have shown that some parameters related to the three-dimensional anatomy of the spleen, such as orientation of the splenic vessels, could be associated with the severity of a splenic injury during a road accident.
Splenic lesions may occur in many different circumstances. Therefore, to gather a relatively homogenous population, this study focused on traffic accidents only, but even with this selection parameter, the injury mechanisms involved can be multiple (direct impact, deceleration) and associated. The results in this study show no evidence of aggravating or mitigating circumstances for the conditions in which the accident occurred in severe splenic trauma; even for seatbelt use, which agrees with some studies [19,20]. However, Holbrook et al., have demonstrated the negative role of the seat belt on the liver [21]. The debate continues since studies have shown that the incidence rate of injury to intraabdominal organs was higher for belted passengers [22].
The analysis of clinical or radiological data does not make it possible to understand the process leading to traumatic injury. However, classifying injuries according to their severity highlights the factors associated with their seriousness, which makes it possible to speculate on the role of each factor in the traumatic process. Orientation of the spleen’s hilar surface is associated to severe lesions in this study, as its position affects the way the neighbouring organs will fit together and around the splenic parenchyma and the hilum. If the hilar side is turned toward the front of the body, the hilar vessels will get more protection from the parenchyma behind them. A full stomach will also protect the spleen from severe splenic trauma, acting like an airbag inside the abdomen. The left liver overflowing into the left hypochondrium will have the same protective effect, and, like the rib cage, gastric and hepatic tissues will absorb the shock waves. The incidence of 10th left rib fracture is not related to a more severe splenic lesion in our study. This result reaffirms the debate associated to the rib cage [23]: Is it a protective hammock or a danger for the parenchyma? in this analysis, the younger patients had the most severe injuries, which suggests anatomical avenues for reflection. As people age, the thoraco-abdominal region changes: morphotype tends to be stocky, costo-xiphoid angle opens, muscle strap loosens, the vertebral column settles down, and this brings about a re-organisation, re orientation of the relationships between intra-abdominal organs. Factoring for different local conditions, might explain that the elderly present less severe splenic lesions. Likewise, our population of young people, essentially male, corresponds to those more exposed to severe injuries, as highlighted by French demographic data [1]. In this study, a status of obesity was not associated with a higher risk of severe splenic lesion. The adipose tissue would protect the splenic parenchyma in a case of direct impact, but cases of existing deceleration in blunt abdominal trauma have not been studied yet. Other studies on trauma in obese patients have reported that complications due to trauma increase morbidity and mortality rates, but not the severity of the original lesion to the internal organs themselves [24-26].
The main limitation of this study is the low number of patients included in the severe splenic lesion group. This bias results from the study’s methodology which requires a spleen CT-scan. Grade 5 hemodynamically unstable patients go directly to the operative room and undergo haemostasis splenectomy, and are therefore impossible to include in this type of analysis.
CONCLUSIONS
This work suggests that parameters of intrinsic and extrinsic variability condition the tolerance threshold of the abdominal organs during trauma. These hypotheses require further laboratory study to define the role of each movement and each anatomical structure in terms of shock resistance [10-13]. Such a study could use a numerical 3D model in which the biomechanical properties of each organ are determined by experimental tests [27-30]. This would be of major interest because it allows for wide-scale tests as they are free from the problems inherent in studies using post-mortem human surrogates. Trauma conditions can be infinitely adapted (high or low kinetic trauma, car or bike accident and so forth), as well as the means of prevention (effects of seat belts, airbags, and so forth). This virtual human could then be used to improve prevention, protection devices, but also as a way to aid clinical decision.
COMPLIANCE WITH ETHICAL STANDARDS
Conflict of interest: The authors declare that they have no conflict of interest. For this type of study, formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
ACKNOWLEDGMENT
The authors wish to thank the Laboratory of Applied Biomechanics of Aix-Marseille University, Marseille, France and Kathleen Beaumont for language and writing assistance.
REFERENCES
- Observatoire National Interministériel de Sécurité Routière (2012) La sécurité routière en France : Bilan de l’année 2011. Observatoire National Interministériel de Sécurité Routière, La documentation française, France.
- Cheynel N, Gentil J, Freitz M, Rat P, Ortega Deballon P, et al. (2011) Abdominal and pelvic injuries caused by road traffic accidents: Characteristics and outcomes in a french cohort of 2009 Casualties. World J Surg 35: 1621-1625.
- Helmi I, Hussein A, Ahmed AH (2001) Abdominal trauma due to road traffic accident in Qatar. Injury 32: 105-108.
- Richardson JD (2005) Changes in the management of injuries to the liver and spleen. J Am Coll Surg 200: 648-669.
- Edgren G, Almqvist R, Hartman M, Utter GH (2014) Splenectomy and the risk of sepsis a population-based cohort study. Ann Surg 260: 1081-1087.
- Cirocchi R, Boselli C, Corsi A, Farinella E, Listorti C, et al. (2013) Is non-operative management safe and effective for all splenic blunt trauma? A systematic review. Crit Care 17: 185.
- Liu P, Liu H, Hsieh T, Huang C, Ko SF (2012) Nonsurgical management of delayed splenic rupture after blunt trauma. J Trauma Acute Care Surg 72: 1019-1023.
- Tinkoff G, EspositoTJ, Reed J, Kilgo P, Fildes J, et al. (2008) American association for the surgery of trauma organ injury scale I: Spleen, liver, and kidney, validation based on the national trauma data bank. J Am Coll Surg 207: 646-655.
- Moore EE, Cogbill TH, Jurkovich GJ (1995) Organ injury scaling: Spleen and liver (1994 revision). J Trauma 38: 323-324.
- Stingl J, Bá?a V, Cech P, Kovanda J, Kovandová H, et al. (2002) Morphology and some biomechanical properties of human liver and spleen. Surg Radiol Anat 24: 285-289.
- Nicolle S, Noguer L, Palierne JF (2012) Shear mechanical properties of the spleen: Experiment and analytical modelling. J Mecha Behav of Biomed Mater 9: 130-136.
- Kemper AR, Santago AC, Stitzel JD, Sparks JL, Duma SM (2012) Biomechanical response of human spleen in tensile loading. J Biomech 45: 348-355.
- Umale S, Deck C, Bourdet N, Dhumane P, Soler L, et al. (2013) Experimental mechanical characterization of abdominal organs: Liver, kidney & spleen. J Mecha Behav of Biomed Mater 17: 22-33.
- Behr M, Arnoux PJ, Serre T, Bidal S, Kang HS, et al. (2003) A human model for road safety: From geometrical acquisition to model validation with radioss. Comput Methods Biomech Biomed Engin 6: 263-273.
- Caix M, Cubertafond P (1978) Etude anatomique de la région thoraco-abdominale considérée en fonction du type morphologique. Anat Clin 1: 185-188.
- Studer AS, Kahn CJF, Bège T, Thollon L, Loundou A, et al. (2015) An anatomic and morphometric analysis of splenic variability using 3D reconstruction and spatial orientation from computed tomography. Ann Anat 201: 50-55.
- Didansky PM (1925) Les divers types de formes et de position des organes du corps humain. In: Bulletins et mémoires, Société anatomique de Paris, Paris, France..
- Dufour, Rigaud, Cabanié, Gouazé (1952) Les types morphologiques humains. In: Bulletins et mémoires, Société anatomique de Paris, Paris, France. Pg no: 174-186.
- Rutledge R, Thomason M, Oller D, Meredith W, Moylan J, et al. (1990) The spectrum of abdominal injuries associated with the use of seat belts. J Trauma 31: 825-826.
- Siegel JH, Mason-Gonzalez S, Dischinger P, Cushing B, Read K,t al. (1993) Safety belt restraints and compartment intrusions in frontal and lateral motor vehicle crashes: mechanisms of injuries, complications, and acute care costs. J Trauma 34: 736-758.
- Holbrook TL, Hoyt DB, Eastman AB, Sise MJ, Kennedy F, et al. (2007) The impact of safety belt use on liver injuries in motor vehicle crashes: The importance of motor vehicle safety systems. J Trauma 63: 300-306.
- Sharma OP, Oswanski MF, Kaminski BP, Issa NM, Duffy B, et al. (2009) Clinical implications of the seat belt sign in blunt trauma. Am Surg 75: 822-827.
- Park S (2012) Clinical analysis for the correlation of intra-abdominal organ injury in the patients with rib fracture. Korean J Thorac Cardiovasc Surg 45: 246-250.
- Hoffmann M, Lefering R, Gruber-Rathmann M, Rueger JM, Lehmann W (2012) The impact of BMI on polytrauma outcome. Injury 43: 184-188.
- Cramer C, Rueger JM, Hoffmann M (2013) Fat or thin: does it impact outcomes in polytrauma? J Trauma 15: 301-307.
- Ditillo M, Pandit V, Rhee P, Aziz H, Hadeed S, et al (2014) Morbid obesity predisposes trauma patients to worse outcomes: A national trauma data bank analysis. J Trauma Acute Care Surg 76: 176-179.
- Brunet C, Serre T, Cheynel N, Arnoux PJ, Thollon L, et al. (2004) Les traumatismes virtuels du foie : Apport des essais expérimentaux en sollicitation dynamique et de la modélisation numérique.. E-mémoires de l’ ANC 3: 73-82.
- Bourgoin S, Bège T, Lalonde N, Mancini J, Masson C, et al. (2012) Three dimensional determination of variability in colon anatomy: Applications for numerical modeling of the intestine. J Surg Res 178: 172-180.
- Massalou D, Bège T, Masson C, Bourgoin S, Foti P, et al. (2013) Influence of loading speed on the mechanical properties of the colon. Comput Methods Biomech Biomed Engin 16: 189-190.
- Bège T, Ménard J, Tremblay J, Denis R, Arnoux PJ, et al. (2015) Biomechanical analysis of traumatic mesenteric avulsion. Med Biol Eng Comput 53: 187-194.
Citation: PurposeAnalysis of influence of anthropomorphometry, splenic variability and crash’s circumstances on the severity of splenic injury.MethodsSeventy-seven patients with blunt splenic trauma had a tomodensitometry at time of admission. Localisation, type, and lesion’s severity (AAST classification), were determined. Severe splenic lesion was defined by: Grade 4 or 5, lesion of entire parenchyma, or fracture. Three-dimensional splenic segmentation allowed calculation of volume, orientation (colatitude and azimuth), morphometry, morphology and span of hilar vessels. Anthropometric parameters were: Age, gender, BMI, and morphotype. Relationships between spleen, stomach, liver and 10th left rib were detailed.ResultsIn univariate analysis, splenic parameters for a severer lesion were: Orientation of hilar side turned towards vertebral column (azimuth, p=0.05), spread conformation of hilar vessels (p=0.10), and high splenic volume (p=0.06). The younger the patient, the more severe was the splenic lesion (p=0.07). A full stomach and a left liver overflowing in the left hypochondrium, were associated with low gravity splenic lesion, (p=0.02 and p=0.03). In multivariable analysis, injured patients whose hilar area was vertically oriented, were more at risk of severe splenic lesion (OR=0.92, 95% CI (0.85-0.99), p=0.02). An abdominal-shaped liver was associated with low gravity splenic lesion (OR= 0.13, 95% CI (0.02-0.93), p=0.04).ConclusionsTopographic and morphologic variability of the spleen condition its vulnerability in trauma cases. Using this analysis and the biomechanical behaviour of splenic tissue will allow for the creation of a splenic numerical model, and its integration in the virtual human scientific application of modern traumatology.
Copyright: © 2018 Anne-Sophie Studer, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.