
Simple Loop Stitch Tie over Technique for Skin Graft
*Corresponding Author(s):
Sabry MDepartment Of Plastic And Reconstructive Surgery, Minia University, Minia, Egypt
Tel:+20 0862371220, +20 1001233552
Email:patriot3832001@yahoo.com, Mohamed.Sabri@mu.edu.eg
Abstract
Purpose: We use a modified technique for tie over in the form of multiple opposing simple loop stitches tied by rubber bands to allow re-application of tie over if indicated without anesthesia.
Methods: The study was conducted on 20 patients presented by raw areas of variable etiologies, treated with skin grafting and simple loop stitch tie over technique.
Results: The patients were followed up for 1-2 months. All grafts showed very good to excellent results as the skin graft take ranges from 75% to 100%. Complications were seen in 5 cases in one case was slipped one simple loop and the other 4 cases was local infection.
Conclusion: We documented a modified, simple, economic, time saving and applicable tie-over dressing that allows fixing and re-fixing of the skin grafts when needed to maintain a proper pressure dressing to the wound.
Keywords
INTRODUCTION
Skin grafting is one of the oldest fundamental procedures of the field of plastic and reconstructive surgery. Tie-over dressing is the most widely used method to secure the skin graft to its recipient bed, reduce the size of dead space, and prevent hematoma formation under the graft. The traditional technique consists of the use of long silk sutures along the circumference of the graft that are tied over impregnated non-adherent gauze filled with a bolus of fluffy gauze. The tedious and time-consuming nature of its application has led to numerous modifications with different suturing [1].
Many modifications to the tie-over suture include the following: A simple tie-over-bolus dressing for skin grafts, the pressure button as a refinement of the traditional “tie-over” dressing, the use of collars and beads with the classic stitches, the ‘‘lacing suture’’ technique, which combines marginal staples with two running stitches that are tied in the middle, a spring-loaded clamp, tie-over sutures secured using a modified 10 ml syringe and its piston,‘‘running’’ tie-over , multiple loop sutures, an elastic tape with silk threads to be for the tie over dressing, tie-over dressing with criss-cross lacing pattern, tie-over bandage for treating raw areas in animals, tie-over dressing using multiple loop silk threads and a barbed suture tie over [1-13].
The purpose of our study was to establish a new modification in the already described technique of tie over in the form of multiple opposing simple loop stitches tied by rubber bands to allow reapplication of tie over if indicated without anesthesia.
METHODS
Between May 2015 and April 2016, a prospective study was conducted on 20 patients their age ranged (2-55 years) with Mean ± SD 22.6 ±17.14 presented by raw areas in various parts of the body were admitted at plastic surgery department, Minia University Hospital, Mina, Egypt. Of these, 17 were males and 3 females. The etiology of these raw areas was full thickness burn in 4 cases (20%), post traumatic in 5 cases (25%), post keloid excision in 3 cases (15%) and post excision of skin malignancies Basal Cell Carcinoma (BCC) and Squamous Cell Carcinoma (SCC) with safety margin in 2 cases (10%), post release of post burn contractures in 3 cases (15%), diabetic foot in 1 case (5%) , post excision of hairy mole in 1 case (5%) and post fire arm injury in 1 case (5%). The patients or their guardians provided an informed consent.
All patients operated under general anesthesia. After application of the skin grafts either Split Thickness Skin Graft (STSG) or Full Thickness Skin Graft (FTSG) and its fixation by metal staples or vicryl a multiple opposing simple loop stitches using 2-0 vicryl in 10 cases (50%) and 2-0 prolene suture in 10 cases (50%) introduced from the graft to its adjacent wound edge and tied like a loop suture. And repeated along the wound edges (Figure 1A). Dressing is prepared to fit the size and the length of the graft bed. Non adherent vaseline gauze is placed over the skin graft followed by the prepared sterile bolus dressing consisting of cotton. A rubber band is passed between two opposite loops. Lastly the rubber bands are tied over the dressings (Figures 1B & C).
Usually the first dressing was done at the 5th day, the graft was assessed and the tie-over dressing was performed again by passing the rubber bands between the opposite loops again (Figure 1) without anesthesia for another 5 days.
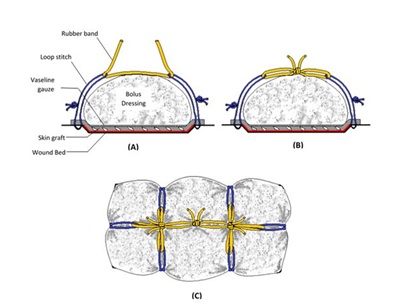 Figure 1: Schematic diagram showing the steps of simple loop stitch tie over technique A: A no adherent vaseline gauze is placed over the skin graft followed by a sterile bolus dressing consisting of cotton. Loop stitches are then performed at edges of the wound by prolene or vicryl 2/0 (blue). A rubber band (yellow) is passed between two opposite loops. B: Appearance after tying the rubber bands. C: Top view showing the final appearance of loop stitch tie over technique.
Figure 1: Schematic diagram showing the steps of simple loop stitch tie over technique A: A no adherent vaseline gauze is placed over the skin graft followed by a sterile bolus dressing consisting of cotton. Loop stitches are then performed at edges of the wound by prolene or vicryl 2/0 (blue). A rubber band (yellow) is passed between two opposite loops. B: Appearance after tying the rubber bands. C: Top view showing the final appearance of loop stitch tie over technique.
But if there were any signs of infection or soaked dressing, rapidly we remove the dressing as early as possible then repeated saline wash and topical antibiotic was added over the graft then the rubber bands were introduced between the opposite loops to take the advantage of the repetitive nature of our technique. This can be done daily until the infection subsides or the soaking of the dressing decreases.
The success rate of graft take was registered by the same surgeon using the formula:
Usually all patients were discharged from the hospital after the 1st dressing then removal of all stitches or staples after the 2nd dressings unless the patient needed repeated dressings (infection or soaked dressing). The follow-up period ranges from 1-2 months after discharging the patient.
Statistical descriptive analysis was carried out by using SPSS 24.0 software.
RESULTS
After surgery, as shown in (Table 1), among the 20 grafts in our study, all grafts showed very good to excellent results as the skin graft take ranges from 75% to 100%. STSG was used in 19 patients (95%) and FTSG was used in 1 patient (5%). We used simple loop stitch tie over dressing technique on different sites of the body. The chest wall 2 skin grafts (10%), leg 2 skin grafts (10%), upper limb 7 skin grafts (35%), groin 1 skin graft (10%), neck 1 skin graft (5%), face 2 skin grafts (10%),foot 4 skin grafts (20%) and scalp 1 skin graft (5%) (Figures 2-6). Complications were seen in 5 cases in one case was slipped one simple loop stitch and the cause was the stitch wasn’t well tied on itself and the patient needs no interference, and in the other 4 cases was the local infection that was treated by wash, topical antibiotic and re application of tie over until complete take of the graft.
|
Patient |
Age in Years |
Etiology |
Site of Raw Area |
Type of Skin Graft |
Complications |
% of Graft Take |
|
No |
||||||
|
1 |
2 |
Burn |
Lt arm and forearm |
STSG |
----- |
9o% |
|
2 |
18 |
Burn |
Chest wall |
STSG |
------ |
90% |
|
3 |
19 |
Burn |
Lt arm |
STSG |
1 loop stitch slipped |
90% |
|
4 |
30 |
RTA |
Rt leg |
STSG |
Local infection |
80% |
|
5 |
35 |
RTA |
Lt leg |
STSG |
Local infection |
90% |
|
6 |
42 |
SCC |
Chest wall |
STSG |
Local infection |
90% |
|
7 |
3 |
Post burn contracture |
Neck |
STSG |
----- |
100% |
|
8 |
8 |
Keloid |
Face |
STSG |
------ |
100% |
|
9 |
50 |
BCC |
Face |
FTSG |
------- |
100% |
|
10 |
9 |
Post burn contracture |
Lt elbow |
STSG |
---- |
100% |
|
11 |
4 |
Post burn contracture |
Lt hand |
STSG |
----- |
100% |
|
12 |
46 |
RTA |
Rt foot |
STSG |
----- |
90% |
|
13 |
4 |
Burn |
Rt arm |
STSG |
---- |
90% |
|
14 |
20 |
Firearm |
Lt arm |
STSG |
---- |
100% |
|
15 |
30 |
Hairy mole |
Scalp |
STSG |
---- |
100% |
|
16 |
12 |
RTA |
Lt groin |
STSG |
---- |
90% |
|
17 |
8 |
Keloid |
Rt foot |
STSG |
---- |
100% |
|
18 |
40 |
RTA |
Lt foot |
STSG |
---- |
90% |
|
19 |
55 |
Diabetic foot |
Rt foot |
STSG |
Local infection |
75% |
|
20 |
17 |
Keloid |
Rt foream |
STSG |
----- |
100% |
Table 1: Patients Data.
(STSG-Split Thickness Skin Graft; FTSG- Full Thickness Skin Graft; RTA- Road Traffic Accident; SCC- Squamous Cell Carcinoma; BCC- Basal Cell Carcinoma; Lt- Left; Rt- Right).
 Figure 2: 8 years old child with post burn keloid on the lt side of the face A: Preoperative, B: Excision of keloid, C: STSG Application, D: Simple loop stitch are placed at wound edges, E: Application of bolus dressing and the loops tied using rubber bands, F: 10th day, G: 2 weeks and H: 1 month post-operative.
Figure 2: 8 years old child with post burn keloid on the lt side of the face A: Preoperative, B: Excision of keloid, C: STSG Application, D: Simple loop stitch are placed at wound edges, E: Application of bolus dressing and the loops tied using rubber bands, F: 10th day, G: 2 weeks and H: 1 month post-operative.
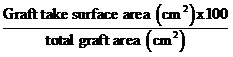
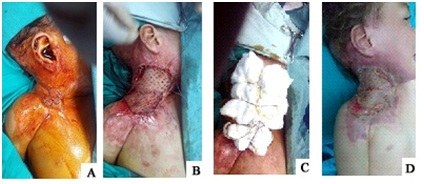 Figure 3: 3 years old child with post burn contracture on the right side of the neck, A: Preoperative, B:Application of STSG and Simple loop stitches, C: Application of bolus dressing and the loops tied using rubber bands and D: 3 weeks post-operative.
Figure 3: 3 years old child with post burn contracture on the right side of the neck, A: Preoperative, B:Application of STSG and Simple loop stitches, C: Application of bolus dressing and the loops tied using rubber bands and D: 3 weeks post-operative.
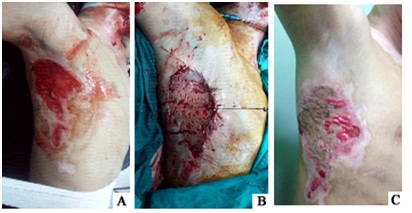 Figure 4: 18 years old male patient with post burn raw area on lateral chest wall, A: Preoperative, B:Application of STSG and simple loop tie over sutures and C: 1 month post-operative.
Figure 4: 18 years old male patient with post burn raw area on lateral chest wall, A: Preoperative, B:Application of STSG and simple loop tie over sutures and C: 1 month post-operative.
 Figure 5: 9 years old child with post burn contracted left elbow, A: Preoperative, B: Raw area after release of the contracture, C: STSG Application, D: 1 week and E: 1 month post-operative.
Figure 5: 9 years old child with post burn contracted left elbow, A: Preoperative, B: Raw area after release of the contracture, C: STSG Application, D: 1 week and E: 1 month post-operative.
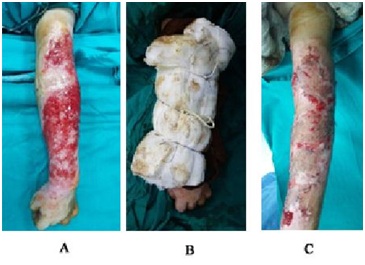 Figure 6: 2 years old child with post burn raw area on the left upper limb, A: Preoperative, B: Simple loop stitch tie over and C: 2 weeks post-operative.
Figure 6: 2 years old child with post burn raw area on the left upper limb, A: Preoperative, B: Simple loop stitch tie over and C: 2 weeks post-operative.
DISCUSSION
In a skin graft, good postoperative care begins with the dressing, a bolus or tie-over dressing can be used. The bolus dressings minimize the risk of hematoma or seroma formation and also prevent shearing forces from disrupting the graft [14].
Although tie-over dressings are widely used when performing skin grafts, the difficulty in re-fixation after the dressing has been opened is the disadvantage of a conventional tie-over dressing. Many researchers have introduced various tie-over dressing methods; of them, those that are reproducible have also been introduced [1,3,11,12].
Our method (simple loop stitch suture tie over technique) differs from the classic method in that repetitive tie-over dressing is possible to perform using simple loop stitch. When tie-over dressing needs to be opened in the early stage to examine the skin graft and then re-fixation is required in patients with infected wound or a bleeding tendency, re-fixation could be carried out on the skin graft sites as in the operation which was applied in 4 cases of our series who suffered from infection and the repetitive nature of our technique helped the survival of the graft and their take ranged from (75-90%) and the patients did not need any other operative interference.
Moreover, proper tension was maintained on the skin graft sites via simple loop suture technique in body areas where dressing fixation is difficult and hairy sites like face (Figure 2), neck (Figure 3) chest wall (Figure 4). Some authors have reported methods that utilize materials such as a bra hook with a band or a jacket clip for a reproducible tie-over dressing [15,16].
A tie-over dressing using a bra hook with a band may be difficult to apply to extremely large or small wounds, whereas the tie-over dressing that we introduced could be applied regardless of the size of the defect site by controlling the length of the simple loops. In addition, as we used vicryl, prolene or rubber bands materials that were easily obtained, we did not have to prepare special materials during the preparation for surgery.
Hyeon et al., in 2013, using their method (multiple loop sutures technique) had the disadvantage that multiple loop thread must be fabricated, they sterilized and reused the threads that were utilized during the tie practice, thereby saving the time that would have been needed to make multiple loop threads during surgery which we did not have to do in our series as we used a single simpler loop stitch technique [12].
Another advantage of our technique is the pressure gained over the skin graft as a double pulley system like the technique used by Misra and Belecher in 2002 which gain more pressure than that gained by the conventional tie over technique [9].
As for saving the suture material in comparison with the conventional tie over technique when long sutures are used and wasted in that technique. Using our technique we determine the length of the suture needed to fit the amount of the dressing and is more saving and economic than the conventional one.
Before starting this series we anticipated some other complications such as skin necrosis between the ends of the loop sutures but it did not occur because we avoided excessive tension on the loop sutures. The application of the simple stitch tie-over dressing takes shorter time less than the classic tie over and can be done again and again without anesthesia which is not found in the classic tie over method.
CONCLUSION
We documented a modified, simple, economic ,time saving and applicable tie-over dressing that enables easily fixing and re-fixing the skin grafts when needed to maintain a proper pressure dressing to the wound and with this reliable method, the skin grafts were taken successfully.
CONFLICT OF INTEREST
None
REFERENCES
- Ersoy B, ?irino?lu H, Tezel E (2011) Tie-over dressing with criss-cross lacing pattern. Dermatol Surg 37: 1671-1673.
- Christ JE (1982) A simple tie-over-bolus dressing for skin grafts. Surg Gynecol Obstet 154: 246-247.
- Burd DA (1985) The pressure button: A refinement of the traditional “tie-over” dressing. Plast Reconstr Surg 75: 296.
- Niranjan NS (1985) A modified tie-over dressing for skin grafts. Br J Plast Surg 38: 415-418.
- Branfman GS Cassel JM (1988) A simple method for securing a bolster in position over a split-thickness skin graft. Plast Reconstr Surg 81: 136-137.
- Koldas T (1992) A simple method for the classic tie-over dressing. Ann Plast Surg 28: 386-387.
- Amir A, Sagi A, Fliss DM, Rosenberg L (1996) A simple, rapid, reproducible tie-over dressing. Plast Reconstr Surg 98: 1092-1094.
- Pelissier P, Martin D, Baudet J (2000) The running tie-over dressing. Plast Reconstr Surg 106: 1436-1437.
- Misra A, Belcher HJ (2002) A new loop suture tie-over technique for skin graft dressings. J Hand Surg Br 27: 129-133.
- Yoshitatsu S, Takagi T (2002) A new tie-over method improves cosmetic results. Dermatol Surg 28: 542-543.
- Tobias J, Tobias, K (2012) Tie-over Bandage: it’sa stretch. Procedures Pro/NAVC Clinician’s Brief 31-34.
- Jo HJ, Kim JS, Kim NG, Lee KS, Choi JH (2013) Redoable tie-over dressing using multiple loop silk threads. Arch Plast Surg 40: 259-262.
- Joyce KM, Joyce CW, Mahon N, Kelly JL (2015) Use of a barbed suture tie-over technique for skin graft dressings: a case series. Arch Plast Surg 42: 341-345.
- Paletta CE, Pokorny JJ, Rumbolo P (2006) Skin grafting: Plastic surgery (2thedn). Elsevier, New York, USA.
- Do?an F, Ozyazgan I, Eskita?ço?lu T (2006) A new useful and renewable tie-over dressing method using package bands and bra hooks. Ann Plast Surg 57: 348-349.
- Budi S, Rados J, Stanec Z (2009) A sports jacket clip: a simple method of securing tie-over dressings. Journal of Plastic, Reconstructive & Aesthetic Surgery, 62: 495-496.
Citation: Sabry M, El-sheikh AM, Darwish AMA (2018) Simple Loop Stitch Tie over Technique for Skin Graft. J Emerg Med Trauma Surg Care 5: 024.
Copyright: © 2018 Sabry M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

