Y-90 Selective Internal Radiation Therapy to Control Hypoglycemia Caused by Liver Metastases from Malignant Insulinoma
*Corresponding Author(s):
Lorraine PortelanceDepartment Of Radiation Oncology, University Of Miami Miller School Of Medicine, Miami, Florida, United States
Tel:+1 3052434337,
Email:Lportelance@med.miami.edu
Abstract
Insulinomas are uncommon tumors and the majority of these are benign. Malignant insulinomas are associated with worse prognosis. Hypoglycemia resulting from malignant insulinoma is challenging to treat. The efficacy of Yttrium-90 (Y-90) radioembolization is well established for the management of hepatocellular carcinoma and liver metastasis from colorectal cancer. However, only few cases have been reported in the literature in which Y-90 has been used to treat liver metastasis from insulinomas. This case describes the effectiveness of Y-90 radioembolization to control persistent hypoglycemic episodes secondary to liver metastases from a malignant insulinoma.
A 71-year-old patient was diagnosed with a stage IV grade 2 pancreatic Neuroendocrine Tumor (NET) in January 2013. Patient was started on octreotide Long-Acting Repeatable (LAR) (Sandostatin LAR, Novartis) administered intramuscularly at a dose of 30 mg. Soon after she was admitted for syncopal episodes from hypoglycemia. The hypoglycemia was refractory to standard medical management. It was then decided to perform an explorative laparotomy and distal pancreatectomy. Unfortunately, the hypoglycemic episodes persisted after surgery. Patient was referred to interventional radiology and a Trans Arterial Bland Embolization (TABE) targeting the right liver lobe metastasis was done. A week after undergoing TABE she was re-admitted for refractory hypoglycemia.
She was then started on everolimus (Afinitor, Novartis) and a Y-90 radio embolization of the right liver lobe was done. Patient is now 60 months post procedure and never had another episode of hypoglycemia since then. To our knowledge, this combination of Y-90 radio embolization and everolimus has the longest hypoglycemic control reported to date.
INTRODUCTION
Insulinomas represent an uncommon type of NET (Neuroendocrine Tumor) with an incidence of four cases per million person-years [1]. Patients typically present with a history of recurrent hypoglycemic episodes. The majority of these tumors are benign. Surgical resection is the treatment of choice and patients with benign tumors have an 88% overall survival at 10 years [1]. Malignant insulinomas are much lesscommon, representing 5%-10% of these tumors and are associated with worse 10-yearoverall survival (20-30%) [1,2]. Metastatic liver lesions represent the main cause of persistent postoperative symptomatic hypoglycemia in malignant insulinoma [2].
Persistent hypoglycemic episodes from malignant insulinoma often fail multiple treatment modalities and require constant dextrose infusion [3]. The majority of insulinomas do not respond to somatostatin analog therapy as other types of NETs [4] do. Other treatment options, including chemotherapy,and hepatic artery embolization have been used with variable outcomes. More recently the use of Peptide Receptors Radio Nuclide Therapy (PRRT) has been introduce in the management of patients with gastro intestinal NET and seems to be a valuable treatment option.
Selective Internal Radiation Therapy (SIRT) with Yttrium-90 (Y-90) microspheres is an effective treatment for hepatocellular carcinoma and liver metastasis from colorectal cancer or NETs [3,5,6]. However, only few cases have been published in which Y-90 was used for metastatic insulinomas [3,7]. The following case illustrates the potential of Y-90 SIRT to control recalcitrant hypoglycemic episodes secondary to insulinoma liver metastases.
CASE
A71-year-oldHispanic woman was diagnosed with stage IV grade 2 pancreatic NET in January 2013. Her symptoms began about a year before with epigastric pain. In January 2013, she consulted a gastroenterologist with worsening pain and episodes of diarrhea. An endoscopic ultra- sound-guided fine needle aspiration of the pancreas yielded a diagnosis of well-differentiated neuroendocrine tumor with immunohistochemistry showing Ki-67 proliferation rate of 5%, mitotic activity less than 2 per 10 HPF. Tumor cells stained strongly positive for chromogranin, insulin and synaptophysin. Magnetic Resonance Imaging (MRI) on April 2013 showed a tumor of the body and tail of the pancreas with a left para-aortic and two peripancreatic lymph nodes. A pentetreotide scan in May 2013 confirmed the presence of an avid mass in the body and tail of the pancreas with metastases throughout the liver mostly in the right hepatic lobe, the latter seen also in a CT scan (Figure 1). It also showed left para-aorticlymph node and peritoneal carcinomatosis. At that moment, laboratories showed a glucose of 51mg/dL. She was started on octreotide LAR (Sandostatin LAR, Novartis) administered Intra-Muscularly (IM) at a dose of 30 mg every four weeks.
 Figure 1: Axial CT scan with contrast prior to Y-90 liver radioembolization. (Image shows numerous contrast enhancing liver metastases).
Figure 1: Axial CT scan with contrast prior to Y-90 liver radioembolization. (Image shows numerous contrast enhancing liver metastases).
Six weeks later, she presented to our institution with lower extremities weakness, frequent falls and syncopal episodes. She was admitted for refractory hypoglycemic episodes that required continuous infusion of D10W, octreotide (Sandostatin) 250 mcg subcutaneous, dexamethasone 1 mg bid and diazoxide, 10mg/Kg/day divided in three equal doses. She continued having multiple daily hypoglycemic episodes as low as 30mg/dL over the next month despite the above-mentioned combined therapy. Given the fact that she had refractory hypoglycemia, which required hospitalization, she was taken to the operating room for a laparotomy and distal pancreatectomy. Pathology showed a pT3N1M1 grade-2 well-differentiated neuroendocrine tumor with evidence of lymphatic vessels and perineural invasion, metastasis to one of one sampled lymph nodes, omentum, diaphragm and liver.
After her procedure, the hypoglycemic episodes persisted. An octreoscan described at least three metastatic lesions in the right liver lobe and widespread lesions throughout the abdomen and pelvis. She was referred to interventional radiology for bland embolization of her liver metastases. The planning angiogram showed multiple vascular masses throughout the right liver lobe. The patient underwent a Trans Arterial Bland Embolization (TABE) through the right hepatic artery using 1.14 mL of suspended 100-300 µm Bead Block® (Biocompatibles UK Ltd., BTG International, Farham, UK) microparticles, followed by 1 mL of suspended 300-500 µm Embosphere® (Merit Medical Systems, Inc., USA) micro particles, until near stasis.
Eight days after the TABE procedure she was re-admitted for hypoglycemia. Hypoglycemic episodes two days before admission were as low as 40 mg/dL and episodes with undetectable blood glucose were registered during admission. After stabilization, she was discharged with recommendations to continue octreotide LAR (Sandostatin LAR, Novartis)30 mg IM every four weeks, take dexamethasone 1 mg every 12 hours and diazoxide (10 mg/Kg/day divided in three doses). Everolimus (Afinitor, Novartis) 10mg by mouth daily was added by the end of August 2013.
Despite the medical, surgical and interventional therapies, the patient continued to have persistent hypoglycemic episodes and spent most of her day in bed. She was referred for Y-90 SIRT. A planning angiography was done to map the tumor arterial supply and a TcMAA was done to assess the Lung Shunt Fraction (LSF). The LSF was 3.9% and the patient underwent right lobeY-90 SIRT with resin SIR-SPHERES® with a dose of 0.84 GBq (23 mCi) infused through the right hepatic artery in September 2013. Post treatment liver Spect images confirmed a good distribution of Y-90 in the right liver lobe metastasis (Figure 2).
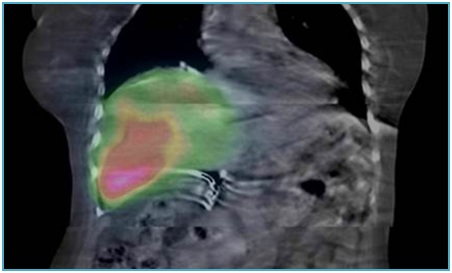 Figure 2: SPECT images post Y-90 liver radioembolization. (Imageshows adequate coverage of the lesions after treatment).
Figure 2: SPECT images post Y-90 liver radioembolization. (Imageshows adequate coverage of the lesions after treatment).
After the Y-90 SIRT procedure there were no more hospital admissions for hypoglycemic episodes. Nine months post treatment, the patient developed a liver abscess which was drained percutaneously. Patient continued close monitoring of her metastatic disease. The patient was last seen in follow up in February 2019, she was asymptomatic and without any significant hypoglycemic episode after her SIRT procedure. She was still taking everolimus (Afinitor, Novartis) 10 mg daily and monthly octreotide LAR at a dose of 30 mg IM. She is tolerating the therapy well with minimal side effects. Her last PET Ga-68 Dotatate scan on 2/21/18 showed no increase in her liver disease. In addition, Everolimus was cut back to every other day because her blood sugar is under better control. She is completely independent on her activities of daily living and has missed some medical appointments because of traveling.
DISCUSSION
Recurrent hypoglycemia from liver metastases cause significant morbidity and is the hallmark symptom of malignant insulinomas. Surgical approaches may have a palliative role, however these procedures carry significant morbidity and the disease tends to recur [8].
Streptozocin-based regimens have the potential to achieve a 39% response rate with a median duration of 9.3 months [9]. Several case reports show control of hypoglycemic episodes and disease stabilization with everolimus [10,11]. Octreotide LAR is frequently being used off label for this medical condition. The combination of octreotide and everolimus blocks the proliferation of cancer cells and inhibits the mTOR-pathway in neuro-endocrine tumors [12]. Everolimus has been associated with hyperglycemia in up to 13% of the patients making it a good therapeutic option for patients with recalcitrant hypoglycemia. Everolimus was prescribed few weeks before the Y-90 SIRT was performed.
TABE is another treatment option. In two published small series, tumor embolization showed decrease in tumor size by more than 50%and hormone suppression within days after the procedure [13]. In our case report, ten days after TABE patient was still having severe hypoglycemic episodes therefore an attempt to treat the liver metastasis with Y-90 SIRT was done.
Y-90 radio embolization is performed by injecting radioactive Y-90 micro-spheres in the hepatic artery under radiologic guidance. This approach is taking advantage of the fact that the blood supply to the normal liver parenchyma is mostly through the venous system while tumors have a rich arterial vascularization.Y-90 SIRT is known to be effective for liver metastasis from NETs. Kennedy et al. reported 60.5% and 2.7% partial and complete tumor regression with the use of this treatment in these tumors and a median survival time of 70 months with no significant toxicities [6].
In this case report, the patient was started on everolimus (Afinitor, Novartis) 10 mg daily in the week preceding the Y-90 SIRT procedure. Everolimus might act as a radiosensitizer, the best way of combining these two modalities is under investigation. To our knowledge, this combination of Y-90 radio embolization and everolimus is the case report with the longest symptom control to this date.
Peptide Receptor Radionuclide Therapy (PRRT) is now considered the standard of care for neuro endocrine tumors refractory to LAR. PRRT is a second line treatment option for patients with metastatic NETs over-expressing somatostatin receptors. A published randomized clinical trial showed that patients with midgut NET who had progressive disease on first line treatment with LAR have an improvement in disease free survival (65.2% in the experimental arm versus 10.8% in the control group at 20 months) when treated with an intravenous infusion of 177Lu-Dotatate every eight weeks compared to octreotide LAR 60 mg every four weeks. The rate of objective tumor response in the therapeutic arm in this study was only 18% (1% complete response and 17% partial response) [14]. In patients for whom tumor response is essential to control symptoms, SIRT with Y-90 might still be used in combination with PRRT.
CONCLUSION
Y-90 radio embolization is a valuable treatment option to control hypoglycemic episodes from hepatic metastases of malignant insulinoma. Although PRRT is now the treatment of choice in patients with NET refractory to Sandostatin LAR, SIRT might still play a role for the control of liver metastasis not responding to systemic treatment.
REFERENCES
- Service FJ, McMahon MM, O'Brien PC, Ballard DJ (1991) Functioning insulinoma--incidence, recurrence, and long-term survival of patients: a 60-year study. Mayo Clin Proc 66: 711-719.
- Starke A, Saddig C, Mansfeld L, Koester R, Tschahargane C, et al. (2005) Malignant metastatic insulinoma-postoperative treatment and follow-up. World J Surg 29: 789-793.
- Chandra P, Yarandi SS, Khazai N, Jacobs S, Umpierrez GE (2010) Management of intractable hypoglycemia with Yttirum-90 radioembolization in a patient with malignant insulinoma. Am J Med Sci 340: 414-417.
- Lamberts SW, van der Lely AJ, de Herder WW, Hofland LJ (1996) Octreotide. N Engl J Med 334: 246-254.
- Ho KW, Wong CC, Balalla B, Diamond T (2006) Malignant insulinomas with hepatic metastases successfully treated with selective internal radiation therapy. Clin Endocrinol (Oxf) 65: 410-411.
- Kennedy AS, Dezarn WA, McNeillie P, Coldwell D, Nutting C, et al. (2008) Radioembolization for unresectable neuroendocrine hepatic metastases using resin 90Y-microspheres: early results in 148 patients. Am J Clin Oncol 31: 271-279.
- Sato KT, Lewandowski RJ, Mulcahy MF, Atassi B, Ryu RK, et al. (2008) Unresectable chemorefractory liver metastases: radioembolization with 90Y microspheres--safety, efficacy, and survival. Radiology 247: 507-515.
- Hirshberg B, Cochran C, Skarulis MC, Libutti SK, Alexander HR, et al. (2005) Malignant insulinoma: spectrum of unusual clinical features. Cancer 104: 264-272.
- Kouvaraki MA, Ajani JA, Hoff P, Wolff R, Evans DB, et al. (2004) Fluorouracil, doxorubicin, and streptozocin in the treatment of patients with locally advanced and metastatic pancreatic endocrine carcinomas. J Clin Oncol 22: 4762-4771.
- Baratelli C, Brizzi MP, Tampellini M, Scagliotti GV, Priola A, et al. (2014) Intermittent everolimus administration for malignant insulinoma. Endocrinol Diabetes Metab Case Rep 2014: 140047.
- Bozkirli E, Bakiner O, Abali H, Andic C, Yapar AF, et al. (2013) A case of inoperable malignant insulinoma with resistant hypoglycemia who experienced the most significant clinical improvement with everolimus. Case Rep Endocrinol 2013: 636175.
- Grozinsky-Glasberg S, Franchi G, Teng M, Leontiou CA, Ribeiro de Oliveira A Jr, et al. (2008) Octreotide and the mTOR inhibitor RAD001 (everolimus) block proliferation and interact with the Akt-mTOR-p70S6K pathway in a neuro-endocrine tumour cell Line. Neuroendocrinology 87: 168-181.
- Marlink RG, Lokich JJ, Robins JR, Clouse ME (1990) Hepatic arterial embolization for metastatic hormone-secreting tumors. Technique, effectiveness, and complications. Cancer 65: 2227-2232.
- Makis W, McCann K, McEwan AJ (2016) Metastatic Insulinoma Pancreatic Neuroendocrine Tumor Treated With 177Lu-DOTATATE Induction and Maintenance Peptide Receptor Radionuclide Therapy: A Suggested Protocol. Clin Nucl Med 41: 53-54.
Citation: Portelance L, Llorente R, Venkat S, Doshi M (2019) Y-90 Selective Internal Radiation Therapy to Control Hypoglycemia Caused by Liver Metastases from Malignant Insulinoma. Int J Case Rep Ther Stud 1: 002.
Copyright: © 2019 Ricardo Llorente, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.