Marijuana Use Predicts Cannabis Withdrawal in Adolescents: A Model of Psychological Dysregulation
*Corresponding Author(s):
Jennifer HarrisDepartment Of Social, Behavioral And Human Sciences Division, University Of Washington, 1900 Commerce St, Tacoma, WA 98402, United States
Tel:+1 5097237757,
Email:harris13@uw.edu
Abstract
Keywords
INTRODUCTION
THE NEUROBEHAVIORAL DISINHIBITION THEORY
Affect dysregulation (e.g., emotional reactivity, arousal, and irritability) has been empirically supported as a risk factor associated with developing substance use disorders [13]. Emotional dysregulation has been shown to be a predisposing factor in perpetuating the use of marijuana [14]. Specifically, depression and irritability predict higher levels of marijuana use in adolescents [15]. Adolescents who exhibit cannabis use disorder have shown high comorbity rates of mood and anxiety disorders, which include substantial amounts of withdrawal symptoms as part of their diagnostic criteria.
Behavioral dysregulation includes inattention, hyperactivity, aggressivity, impulsivity, as well as sensation-seeking behaviors [16,17]. Tarter and colleagues [12] found that adolescents whom exhibit behavioral dysregulation predicted higher frequency of marijuana use than those without the trait. In addition, recent analyses have found that adolescents with behaviors reflective of inattention and hyperactivity - such as Attention Deficit Hyperactive Disorder (ADHD), Operational Defiant Disorder, and Conduct Disorder - were at higher risk for using marijuana [18]. In a study conducted by Jester and colleagues [19], aggression predicted marijuana problems while hyperactivity and inattention established earlier onset of use. Furthermore, the combination of aggressivity and inattention influenced severity of marijuana use. Sensation-seeking behaviors, such as impulsivity in childhood, manifest as positive or negative urgency; these have been correlated with increased marijuana use and a higher risk of continuing sensation-seeking within adolescence [20]. It was determined that impaired impulse control during early adolescence, such as delayed response or response inhibition, may contribute to the increased probability of marijuana use.
Cognitive dysregualtion includes the aspects of cognitive inflexibility as well as the inability to make a plan, carry out a plan, and/or learn from mistakes [16]. Giancola and Tarter [10] found that executive cognitive functioning through the aspects of making a plan, carrying out a plan, and cognitive flexibility were linked to marijuana use. Adolescent marijuana-users also exhibit poor performance in decision making abilities and tend to choose an option that gives them immediate gratification, regardless of the consequences they experience over time. Also, physical and relational aggression in early adolescence was correlated with a greater likelihood of marijuana use later in adolescence [21]. The aforementioned affective, behavioral, and cognitive factors contribute to the transition from recreational use to problematic drug seeking behaviors associated with withdrawal symptoms [22]. These predisposing symptoms are similar to the withdrawal symptoms that arise in response to disruptions in marijuana use. The same psychological factors that precipitate use may help explain the severity of withdrawal.
CANNABIS WITHDRAWAL IN ADOLESCENTS
Adolescents who engage in high frequency marijuana use are at risk for withdrawal similar to adults. Research has found adolescent participants experienced acute withdrawal symptoms such as “craving for marijuana, depressed mood, irritability, restlessness, sleep difficulty, increased anger, decreased appetite, increased aggression, nervousness/anxiety, and headache” [23]. Duffy and Milin [24] recognized a withdrawal syndrome characterized by insomnia, irritable mood, and drug craving within adolescent case studies prior to the DSM-5 inclusion of cannabis withdrawal. Another adolescent case study found anxiety/irritability, decreased appetite, and abdominal pain were significant within hours of abstinence from cannabis [17]. Restlessness, cravings, and appetite change were found to be experienced by adolescents through the third week following the interruption in marijuana use [25]. High comorbidity rates of mood disturbances in chronic cannabis using adolescents demonstrates an association with symptoms of withdrawal [26]. The period of withdrawal seems to fluctuate; however, chronic marijuana use has been shown to elicit withdrawal symptoms as early as one day after cannabis cessation. At this point, the withdrawal symptoms peak and predict a series of indicative responses that became perpetuating factors to reinitiate use [1]. Understanding the factors that intensify withdrawal is important.
PSYCHOLOGICAL DYSREGULATION MODERATES CANNABIS USE AND WITHDRAWAL SYMPTOMS
THE CURRENT STUDY
METHOD
Participants
Marijuana use
Psychological dysregulation
The DI has been found to have sound psychometric properties including satisfactory to superior internal consistency (alpha = .88 for affect; alpha = .92 for behavior; alpha = .71 for cognition), split-half reliability (r = .86 for affect; r = .81 for behavior; r = .68 for cognition), and inter-rater reliability [16]. The inventory has established strong construct and concurrent validity.
Withdrawal
PROCEDURE
RESULTS
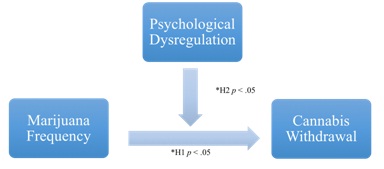
Multiple regressions were used to analyze the effects of marijuana frequency on withdrawal. The results of this analysis R2 = .05, F (1, 121) = 6.85, p < .05, indicate that marijuana frequency significantly predicted cannabis withdrawal. Psychological dysregulation was added as a second step. Psychological dysregulation accounted for a significant amount of the variance, R2 = .08, F (1, 120) = 11.68, p < .05. Therefore, psychological dysregulation appeared to moderate the relationship between marijuana use and withdrawal symptoms - as illustrated in figure 1.
| Variables | Mean | Standard Deviation |
| Marijuana frequency (per month) | 12.73 | 11.18 |
| Psychological dysregulation | ||
| Arousal | 4.77 | 2.74 |
| Emotional reactivity | 16.16 | 6.05 |
| Irritability | 8.88 | 5.26 |
| Impulsivity | 9.21 | 4.00 |
| Inattention | 15.58 | 5.46 |
| Hyperactivity | 8.87 | 4.28 |
| Aggression | 8.63 | 5.42 |
| Make a plan | 9.19 | 4.22 |
| Do a plan | 8.73 | 3.78 |
| Learn from experience | 9.68 | 3.29 |
| Cognitive flexibility | 10.31 | 3.33 |
| Drug withdrawal | 0.52 | 0.50 |
| Variables | Withdrawal |
| Marijuana frequency | .28** |
| Psychological dysregulation | |
| Arousal | .22** |
| Emotional reactivity | .22** |
| Irritability | .24** |
| Impulsivity | .27** |
| Inattention | .26** |
| Hyperactivity | .20** |
| Aggression | .24** |
| Make a plan | 0.12 |
| Do a plan | .17* |
| Learn from experience | .16* |
| Cognitive flexibility | .14* |
DISCUSSION
Marijuana use and related withdrawal symptoms were independently and significantly correlated with psychological dysregulation [20,26]. Specifically, these variables were related to emotional reactivity, affective arousal, irritability, impulsivity, inattention/hyperactivity, aggressivity, ability to carry out a plan, ability to learn from mistakes, and cognitive flexibility. The ability to make a plan was the only measure of psychological dysregulation that was not significantly correlated with marijuana use and cannabis withdrawal symptoms. One explanation for the lack of significance may be related to the age of the participants and their developing prefrontal cortexes, which affects long-term thinking abilities utilized in making a plan [32]. Furthermore, the structure of the DSM-5 classification of withdrawal does not include many cognitive symptoms [9]. This helps explain why ability to make a plan may not be related to withdrawal.
The variance in people’s experiences with cannabis withdrawal are further clarified here in. Substance use treatment facilities would find benefits from heeding clients’ psychological dysregulation and their frequency of marijuana use. This information will prepare practitioners in addressing the cannabis withdrawal symptoms as they arise during the course of treatment. Inversely, a participants’ heightened experience of cannabis withdrawal symptoms may indicate trait psychological dysregulation. This scenario would call for an appropriate mental health assessment, possibly an alteration in their treatment plan, and a referral to a specialized mental health practitioner. Paying attention to particular markers within clients will lead to more holistic treatment and possibly better outcomes.
STRENGTHS AND LIMITATIONS
One limitation of the study was a lack of verification method to confirm participants’ reports of current substance use (e.g., urinalysis); however, the utilization of confidentiality encouraged participants to be honest. Comorbidity of mental health disorders was not analyzed concurrently and may present a confounding variable within the analyses. While the majority of adolescents were referred to the study following a school-reported substance related incident, several students self-referred or referred their peers to the program. Adolescents who were referred by a third party may have had significant differences than those who self-refer. The sample was predominately male (76%) and may not be indicative of the experiences of female substance users. Finally, the demographics of the study were representative of students who attend public schools in Western Washington and may under represent populations within other ethnicities, genders, and socioeconomic statuses.
FUTURE RESEARCH
CONCLUSION
Prior to the release of the DSM-5 in 2013, cannabis withdrawal was not identified as a substance induced disorder. This research confirmed that chronic cannabis use among adolescents predicts accelerated withdrawal symptoms. Psychological dysregulation is a predisposing factor in cannabis use [22]. Furthermore, individuals who demonstrate trait psychological dysregulation are not only at greater risk for chronic cannabis use, but experience more severe withdrawal symptoms. The current research is not only consistent with the neurobehavioral disinhibition theory, but extends understanding of how high frequency cannabis users experience greater salience of withdrawal symptoms.
REFERENCES
- Agrawal A, Pergadia ML, Lynskey MT (2008) Is there evidence for symptoms of cannabis withdrawal in the national epidemiologic survey of alcohol and related conditions? Am J Addict 17: 199-288.
- Allsop DJ, Norberg MM, Copeland J, Fu S, Budney AJ (2011) The Cannabis Withdrawal Scale development: patterns and predictors of cannabis withdrawal and distress. Drug Alcohol Depend 119: 123-129.
- Budney AJ, Hughes JR (2006) The cannabis withdrawal syndrome. Curr Opin Psychiatry 19: 233-238.
- Budney AJ, Hughes JR, Moore BA, Vandrey RA (2004) Review of the validity and significance of cannabis withdrawal syndrome. American Journal of Psychiatry 161: 1967-1977.
- Budney AJ, Moore BA, Vandrey R (2008a) Handbook of the medical consequences of alcohol and drug abuse. In: Brick J (ed.). Health consequences of marijuana use, (2nd edn), The Haworth Press/Taylor and Francis Group, New York, USA. Pg No: 251-301.
- Budney AJ, Moore BA, Vandrey R (2008b) Health consequences of marijuana use. In: Brick J (ed.).Handbook of the Medical Consequences of Alcohol and Drug Abuse, (2nd edn.), The Haworth Press/Taylor and Francis Group, New York, USA. Pg no: 251-301.
- Chung T, Martin CS, Cornelius JR, Clark DB (2008) Cannabis withdrawal predicts severity of cannabis involvement at 1-year follow-up among treated adolescents. Addiction 103: 787-799.
- Cornelius JR, Chung T, Martin C, Wood DS, Clark DB (2008) Cannabis withdrawal is common among treatment-seeking adolescents with cannabis dependence and major depression, and is associated with rapid relapse to dependence. Addict Behav 33: 1500-1505.
- American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders (DSM–5), (5th edn), American Psychiatric Association, Arlington, USA.
- Giancola PR, Tarter RE (1999) Executive cognitive functioning and risk for substance abuse. Psychological Science 10: 203-2015.
- Tarter RE, Vanyukov M, Giancola P, Dawes M, Blackson T, et al. (1999) Etiology of early age onset substance use disorder: a maturational perspective. Dev Psychopathol 11: 657-683.
- Tarter RE, Kirisci L, Mezzich A, Cornelius JR, Pajer K, et al. (2003) Neurobehavioral disinhibition in childhood predicts early age at onset of substance use disorder. Am J Psychiatry 160: 1078-1085.
- Cheetham A, Allen NB, Yücel M, Lubman DI (2010) The role of affective dysregulation in drug addiction. Clin Psychol Rev 30: 621-634.
- Bonn-Miller MO, Vujanovic AA, Zvolensky MJ (2008) Emotional dysregulation: association with coping-oriented marijuana use motives among current marijuana users. Subst Use Misuse 43: 1653-1665.
- Supple AJ, Aquilino WS, Wright DL (1999) Collecting Sensitive Self-Report Data With Laptop Computers: Impact on the Response Tendencies of Adolescents in a Home Interview. Journal of Research on Adolescence 9: 467-488.
- Mezzich AC, Tarter RE, Giancola PR, Kirisci L (2001) The Dysregulation Inventory: A New Scale to Assess the Risk for Substance Use Disorder. Journal of Child & Adolescent Substance Abuse 10: 35-43.
- Chesney T, Matsos L, Couturier J, Johnson N (2013) Cannabis withdrawal syndrome: An important diagnostic consideration in adolescents presenting with disordered eating. Int J Eat Disord 47: 219-223.
- Storr CL, Accornero VH, Crum RM (2007) Profiles of current disruptive behavior: association with recent drug consumption among adolescents. Addict Behav 32: 248-264.
- Jester JM, Nigg JT, Buu A, Puttler LI, Glass JM, et al. (2008) Trajectories of childhood aggression and inattention/hyperactivity: differential effects on substance abuse in adolescence. J Am Acad Child Adolesc Psychiatry 47: 1158-1165.
- Dougherty DM, Mathias CW, Dawes MA, Furr R, Charles NE, et al. (2013) Impulsivity, Attention, Memory, and Decision-Making among Adolescent Marijuana Users. Psychopharmacology 226: 307-319.
- Skara S, Pokhrel P, Weiner MD, Sun P, Dent CW, et al. (2008) Physical and relational aggression as predictors of drug use: gender differences among high school students. Addict Behav 33: 1507-1515.
- Mezzich AC, Tarter RE, Feske U, Kirisci L, McNamee RL, et al. (2007) Assessment of risk for substance use disorder consequent to consumption of illegal drugs: psychometric validation of the neurobehavior disinhibition trait. Psychology of Addictive Behaviors 21: 508-515.
- Vandrey R., Budney AJ, Kamon JL, Stanger C (2005) Cannabis withdrawal in adolescent treatment seekers. Drug Alcohol Depend 78: 205-210.
- Duffy A, Milin R (1996) Case study: withdrawal syndrome in adolescent chronic cannabis users. J Am Acad Child Adolesc Psychiatry 35: 1618-1921.
- Milin R, Manion I, Dare G, Walker S (2008) Prospective assessment of cannabis withdrawal in adolescents with cannabis dependence: a pilot study. J Am Acad Child Adolesc Psychiatry 47: 174-178.
- Dorard G, Berthoz S, Phan O, Corcos M, Bungener C (2008) Affect dysregulation in cannabis abusers. European Child & Adolescent Psychiatry 17: 274-282.
- Van Dam NT, Bedi G, Earleywine M (2012) Characteristics of clinically anxious versus non-anxious regular, heavy marijuana users. Addictive behaviors 37: 1217-1223.
- Smith PH, Homish GG, Leonard KE, Collins R (2013) Marijuana withdrawal and aggression among a representative sample of U.S. marijuana users. Drug Alcohol Depend 132: 63-68.
- Brown SA, Myers MG, Lippke L, Tapert SF, Stewart DG, et al. (1998) Psychometric evaluation of the Customary Drinking and Drug Use Record (CDDR): a measure of adolescent alcohol and drug involvement. J Stud Alcohol 59: 427-438.
- White HR, Labouvie EW (1989) Towards the assessment of adolescent problem drinking. J Stud Alcohol 50: 30-37.
- Miller WR, Rollnick S (2013) Motivational interviewing: Helping people change, Guilford Press, New York, USA. Pg no: 482.
- Wetherill R, Tapert SF (2013) Adolescent brain development, substance use, and psychotherapeutic change. Psychol Addict Behav 27: 393-402.
Citation: Harris J, Stewart DG, Johnson BD, Stanton BC, Charuhas JP, et al. (2016) Marijuana Use Predicts Cannabis Withdrawal in Adolescents: A Model of Psychological Dysregulation J Alcohol Drug Depend Subst Abus 3: 007
Copyright: © 2017 Jennifer Harris, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.