
Discussion on Clinical Application of Iowa Model in TCM Nursing Care
*Corresponding Author(s):
Yufang HaoSchool Of Nursing, Beijing University Of Chinese Medicine, No 6, Wang Jing Zhong Huan South Road, Chaoyang District, Beijing 100102, China
Tel:+86 18911091028,
Email:haoyufang0903@sina.com
Abstract
Nursing science characterized by Traditional Chinese Medicine (TCM), is commonly named nursing in TCM or TCM nursing. It is an indispensable part of the nursing profession in China. While TCM nursing knowledge and techniques are mostly clinical expertise derived from ancient TCM classics, many of which lack standardization. TCM nursing is impeded from dissemination globally. It’s necessary to introduce evidence-based concept into TCM nursing for its standardization and globalization. The Iowa Model of Evidenced-Based Practice (EBP) to promote quality care, as a theoretical EBP implementation model, supports the use of case report and expert opinion as evidence, supports trialing of EBP changes. It is also simple, clear, concise, and application-oriented. Those features are what evidence-based TCM nursing requires and can possibly tackle the problems TCM nursing confronting with. It’s worth a try to adopt this model into TCM nursing units. This article will discuss the clinical application of Iowa Model in TCM nursing care with a specific case.
Keywords
INTRODUCTION
While researches have shown that papers in TCM nursing field are in poor quality generally. Multitudinous papers are the summarization of clinical experience and well-designed randomized controlled trial is scarce [7,8]. Besides, TCM nursing techniques are still not widely used in clinic [2,9]. 42.2% TCM nurses feel that they are devoid of TCM nursing knowledge [2]. These are serious obstacles hindering the advancement of TCM nursing.
Evidence-based nursing was introduced into China in the 1990s. It facilitates clinical nursing research significantly [10]. Evidence-based methodology provides us with a scientific way on nursing research, offers guides on clinical nursing practice and is an effective approach to solve the dilemma that TCM nursing faces [11]. In addition, many evidence-based practice models are available to help break down the complexity of challenge of translating evidence into clinical practice, like Iowa model, JBI model, Stetler model, ACE star model of knowledge transformation, PARIHS Framework etc. Each of them has their own features. Iowa Model [12] uses a flow chart, problem-solving steps and feedback loops to guide the change process, which makes the model simple clear and concise. It supports the use of case study and expert opinion as evidence, supports pilot trial before implementation occurs across system, and designs as an interdisciplinary approach. Those key features seem appropriate for TCM nursing practice. This paper will explore the reasons why evidence-based concept is necessary for TCM nursing; the reasons for the suitability of Iowa Model application into TCM nursing practice. It will also illustrate the utilization of this model into TCM nursing with a specific TCM nursing case figure 1.
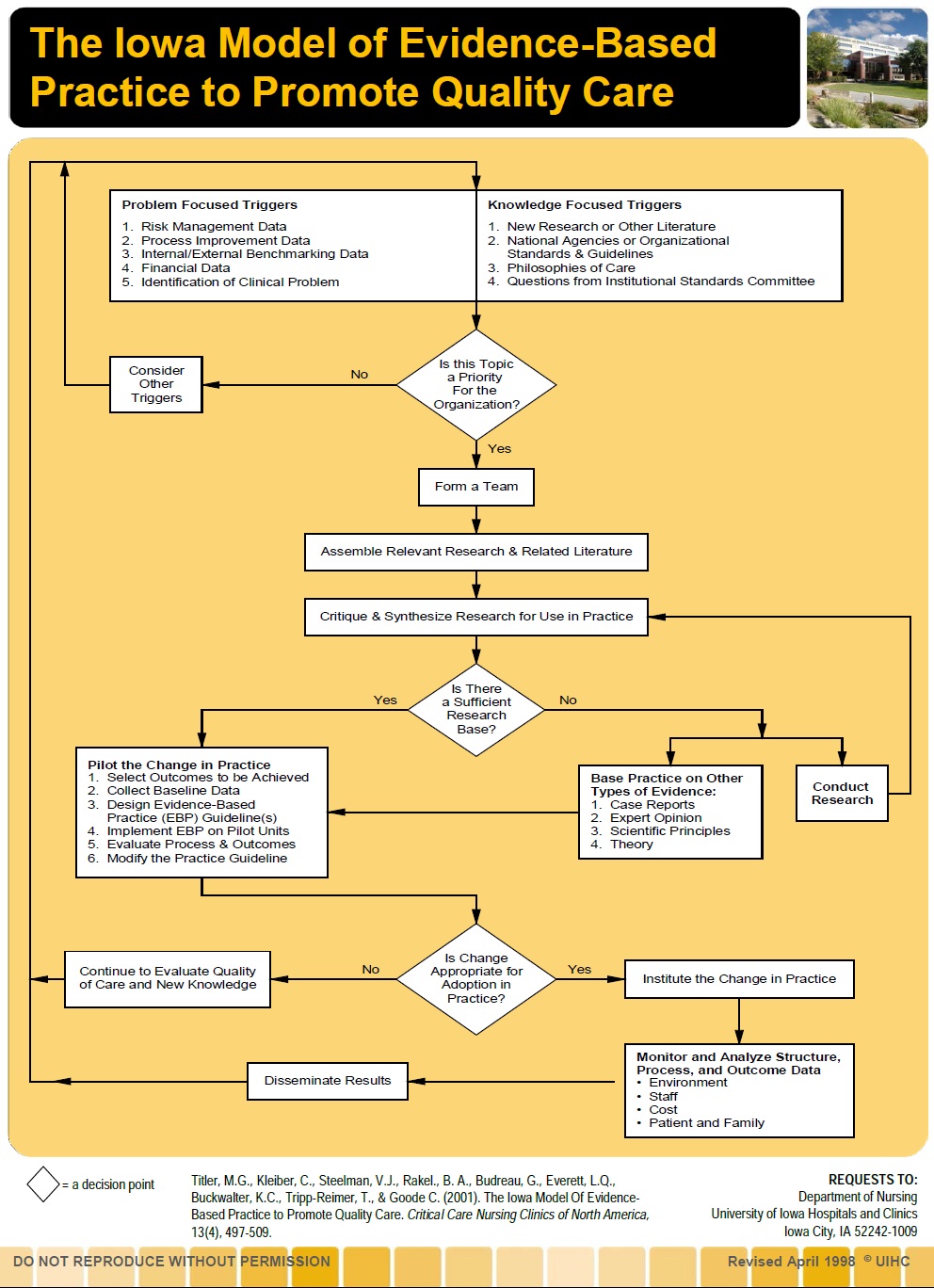 Figure 1: Flow chart - The Iowa Model of Evidence-Based Practice to promote quality care.
Figure 1: Flow chart - The Iowa Model of Evidence-Based Practice to promote quality care.THE NECESSITY OF EVIDENCE-BASED TCM NURSING
For the standardization of TCM nursing
On TCM nursing literature review
By introducing evidence-based nursing methodology into TCM nursing, TCM nurses can have a better grasp of the basics of how various types of study are conducted and how to interpret the results of each study. They can also understand how good data are obtained and how to avoid incorrect conclusions. What’s more they may know different ways of collecting samples and how to choose an appropriate research design. This evidence-based concept triggers nurses to find evidence, make use of evidence, appraise TCM nursing literature critically, and try to design more rigorous clinical trials so as to facilitate the boost on TCM nursing research.
On health education
Advantages of TCM nursing include health education based on theories and techniques of traditional chinese medicine [1]. Recently TCM nursing techniques become quite popular in care for patients with chronic diseases and health education with TCM nursing characteristics plays a pivot role in the process. While a tough problem nursing educators facing is “Why?” “Why should patients follow the advice?” most clinical health education materials are obtained from TCM textbooks, especially books on life cultivation and rehabilitation. However, those books are basically extractions from various TCM classics and mostly are the summarization of ancient clinical experience. Therefore, knowledge can be very diverse in a specific nursing field, and different textbooks sometimes provide inconsistent even incompatible views on a same matter, leading to the dilemma in determining the reliability of health education knowledge. Obviously, lack of evidence becomes an obstacle hindering the acceptability of those health education materials.
The ultimate goal of EBP programs and projects is to improve quality of care by incorporating the best and most recent research evidence into the clinical care practice. If we embed transparent evidences into the health education process, patients would think the education resources more authentic, and would become more satisfied with nurses job, meanwhile gain health-related knowledge. Health education based on evidence can promote a more consistent, safe and cost-effective approach to patient care [14].
On TCM nursing techniques standardization
Research has found that most staff nurses’ practice based on what they were taught by senior nurses and not based on what has been proven to work [15]. When making clinical decisions, nurses use other sources of evidence, such as reflection on their own experiences, rather than EBP [16]. This is what TCM nursing techniques confront with. With the characteristics of simpleness, convenience, effectiveness and low-cost, TCM nursing techniques are favored and admired among citizens. While most of those TCM nursing techniques lack standardization. Although government has promulgated TCM nursing handbooks and guidelines on those techniques, they are made at the experience level without support from scientific and rigorous research findings. With the assistance of evidence-based nursing methods, TCM nursing techniques can possibly be standardized. The variability in conducting those techniques can be diminished.
For the globalization of TCM nursing
Globalization is the further step after standardization. If TCM nursing clinical practice guidelines are evidence-based, it can be widely accepted and furthermore disseminated to other regions and countries. And nurses abroad can have the chance to learn the most reliable and standardized TCM nursing techniques. This can be of great avail for the globalization of TCM nursing knowledge and techniques.
OVERVIEW OF IOWA MODEL
Problem identification
Identify a topic stemming from either problem-focused triggers such as risk management data, process improvement data, internal/external bench-marking data, financial data, or knowledge-focused triggers such as new research or other literature, national agencies or organizational standards and guidelines, philosophies of care, questions from institutional standards committee.
Determine whether the problem identified is a priority for the organization. Those problems that may have higher volume or higher costs associated likely will have higher priority from the organization [19].
Forming a team
The team is responsible for development, implementation and evaluation [20]. The composition of the team should be directed by the chosen topic and include all interested stakeholders [17].
Critique of relevant research
After topic selection and team formation, a brainstorming session should be held to identify available sources and key terms to guide the search for evidence. And this would be an excellent time to enlist a medical librarian who can help search for and retrieve studies to aid in choosing an intervention or answer to the problem or knowledge-focused question [19].
Critique the available studies to determine whether the study with the tested intervention is scientifically sound. Not every research articles published in a professional journal has appropriate scientific merit. Sometimes articles have a small sample size or perhaps use a tool lacking reliability or validity, so critiquing every article prior to considering the results of that study for implementation into a practice change is important.
Decide whether sufficient research exists to implement a practice change. How to determine whether the evidence is sufficient or not? Titler et al., suggested the following criteria: (a) consistent findings exist from numerous studies to support the change, (b) the type and quality of the studies, (c) the clinical relevance of the findings, (d) the number of studies with similar sample characteristics, (e) the feasibility of the findings in practice, and (f) the risk-benefit ratio [12]. If most of the criteria can be met, then pilot the change into practice; if not, conduct research studies.
Implementing practice change
Pilot the change in one small unit. See whether the change is feasible and can bring improved outcome for patients. It involves: selecting the outcomes to be achieved, collecting baseline data, developing a written EBP guideline, testing the guideline on one or more units or with a small number of patients, evaluating the process and outcomes of the trial, and modifying the guideline based on process and outcome data [12].
Dissemination of findings
If the pilot proves successful, it can be extended to an organization practice change. Meanwhile, the team should continue to evaluate the practice change.
THE SUITABILITY OF APPLYING IOWA MODEL INTO TCM NURSING
Support the use of case report, expert opinions as evidence
This principle is particularly vital for TCM nursing. TCM nursing theories and techniques are mostly clinical expertise originated from ancient TCM physicians and classics, many of which are truly effective in clinic while lack of scientific base(without the confirmation from high quality trials, like randomized controlled trial RCT). TCM nursing care is based on the principle of holism and syndrome differentiation, and is often the combination of various interventions. So the classic RCT with placebo is not suitable for the evaluation of this “complex intervention”. Besides, TCM nursing emphasizes the profound effect of the humanistic factors like emotion, spirit and relationship etc. Those factors can hardly be evaluated by the classic quantitative research and entail the involvement of qualitative research methods in sociology. While these qualitative research methods have not been applied to the classification of evidence grading system on intervention effect evaluation. That is one of the deficits of traditional evidence grading system. Experts suggest that although high quality evidence is scarce in TCM nursing, case reports, expert opinions, ancient TCM classics and historical data can also be regarded as the best available evidence currently [21]. We can make full use of those evidence, develop evidence-based TCM nursing protocols, practice in line with the protocol in daily care and be confident that patients are receiving nursing care that is based on best available evidence.
Simple, clear and concise
Evidence-based TCM nursing just springs up in recent years. Most clinical nurses have little knowledge on EBP. These features of Iowa model make itself intuitively understandable for TCM nurses, even novice nurses can understand the process. They need a simple, clear and concise implementation model to help them gain more information and knowledge on EBP and see the benefit from implementing this model so as to enhance their confidence on EBP.
Application-oriented
Developed by practitioners for practitioners, the Iowa Model is feasible for use. It offers a systematic and application-oriented road map and problem-solving steps for EBP that organization uses extensively to guide nursing practice and EBP educational programs [23,24]. It provides some specific guidance to the difficult steps of implementation and offers detailed implementation strategies and dissemination tips.
For TCM nursing, this model is considerate and, to some extent, comprehensive. It’s never easy to make and sustain changes. EBP needs the involvement of various parties in the healthcare system, like nurses, doctors, patients, other healthcare providers and hospital manager etc. Difficulties are fraught in changing their attitude, knowledge and behavior since they have get used to the traditional practice way. At this time, we could turn to those specific tips, resources and materials for help.
Supports trialing of EBP changes
An additional strength of Iowa Model is the inclusion of a trial of the practice change before making the decision about implementation [18]. The team would not conduct a full practice change for the entire organization, but rather would implement a pilot change in one or two smaller practice areas first. The team needs to ensure the change is feasible and will result in improved outcomes before full-scale implementation [19]. It was well-advised that sometimes pilot not be implemented until an infrastructure was in place that would support nurses’ efforts [25]. And the pilot can be tried out, stopped and reversed if it does not work [26].
The pilot change is necessary for evidence-based TCM nursing practice. Since TCM nursing intervention are complicated with aspects of diet nursing, emotional nursing, medication nursing, special TCM nursing techniques, health education and so on, we can’t ascertain the efficacy and feasibility of a specific TCM nursing innovation if those complex nursing interventions are all involved. So it’s indispensable for evidence-based TCM nursing involving such a pilot before full-scale implementation.
EXAMPLE ON THE UTILIZATION OF IOWA MODEL
Though TCM foot bath is effective on the treatment of grade 0 DFU, it lacks standardized nursing procedure and evidence-based clinical guideline to support this TCM nursing technique. For instance, how long should feet soak in the herb? How high should the bath water temperature be? What kind of Chinese medicine shall be chosen? Those questions trigger nurses to develop evidence-based nursing care protocol on the treatment of grade 0 DFU with TCM foot bath.
Firstly an interdisciplinary team with nursing researchers, clinical nurses, nursing leaders, epidemiologist, and hospital manager was built to work together on this project. A comprehensive literature retrieval from MEDLINE, EMbase, CNKI, VIP and Wanfang Data was then conducted with the terms Chinese medicine/Chinese herb/Chinese herbal medicine, diabetic foot/diabetes foot, foot soak/foot bath and following the search, 439 papers were identified as potentially meeting the inclusion criteria. After the screening process and critical appraisal, a total of 9 papers (853 samples) [29-37] were included in the review finally, in which 3 papers are randomized controlled trials and 6 are quasi-experimental studies. Meta-analysis showed that the efficacy of TCM foot bath on patients with grade 0 DFU is better than routine nursing care. However, large-scale randomized controlled trials of higher quality are needed to confirm this result (OR=5.82, 95%CI (3.97, 8.53), P<0.001) [38]. When it comes to developing the evidence-based protocol, though short of research base, expert opinions, TCM nursing handbook and TCM nursing guideline (consensus-based) released by the administration of traditional chinese medicine are made full use of, for example patient observation during foot bath, whether the patient has the symptom of erythema, pruritus, palpation, perspiration and dizziness etc. (level of evidence IV, level of recommendation B); applying skincare to the feet after the bath(level of evidence IV, level of recommendation B); drinking warm-boiled water after foot bath(level of evidence IV, level of recommendation B). Those are all recommendations from expert opinions in this protocol [39]. The next three steps are pilot study in a peripheral vessel disease department in one TCM hospital, determining whether the protocol on grade 0 DFU treatment with TCM foot bath is feasible in clinic and then practice the change.
REFERENCES
- Hao Y, Liu H, Yue S, Liu X (2011) Introducing traditional Chinese nursing: a review of concepts, theories and practices. Int Nurs Rev 58: 319-327.
- Wang JJ, Yang YW, Wang LJ, Bian XM, Li PJ, et al. (2009) Investigation on the status quo of Chinese medicine nursing clinical application. Chin J Nurs 44: 1020-1022.
- Shen Q, Sun QH (2012) Investigation of Chinese medicine care in Zhejiang Province Situation and Development Prospects of. J Zhejiang Chinese Med Univ 36: 215-218.
- Bunk S (2001) Mainstreaming CAM .The Scientist, Ontario, Canada.
- Wang JJ, Wang LJ, Bian XM (2009) Advantages and prospect of Chinese medicine nursing skills. Journal of Traditional Chinese Medicine Management 17: 589-591.
- Ministry of Health of People’s Republic of China (2012) China Nursing Development Plan (2011-2015). Chin J Nurs 47: 286-288.
- Ya-wei S, Li-jiao Y, Yu-fang H (2014) Bibliometric development status of Chinese medicine in China nursing analysis. Chin J Nurs Educ 11: 565-570.
- Hua-ping W, Yong-gang L, Wei-gang Y, Jun-qiang N, Jin-hui T (2012) Situation development of Chinese Nursing Research and Analysis. Education of Chinese Medicine 31: 67-69.
- Wu WF, Li MJ (2012) Progress on therapy Nursing Technology Application. Medical Journal of Chinese People's Health 25: 81-83.
- Hu Y (2005) A correct understanding of evidence-based nursing and promoting the development of nursing practice. Chin J Nurs 40: 714-717.
- Yu-fang H, Wei W, Hui-jun N, Jing M (2012) Thinking of the road of development of TCM colleges and universities care. Chin J Nurs Educ 9: 448-450.
- Titler MG, Kleiber C, Steelman VJ, Rakel BA, Budreau G, et al. (2001) The Iowa Model of Evidence-Based Practice to Promote Quality Care. Crit Care Nurs Clin North Am 13: 497-509.
- Brown SJ (2014) Evidence-based nursing: the research-practice connection (3rdedn). Jones & Bartlett Learning, Massachusetts, USA.
- Crosby E (2013) Review article: the role of practice guidelines and evidence-based medicine in perioperative patient safety. Can J Anaesth 60: 143-151.
- Kin YW, Mordiffi SZ, LiangS, Ang ENK, Xue Z, et al. (2013) Nurses’ perception towards evidence-based practice: a descriptive study. Singapore Nurs J 40: 34-41.
- Rolfe G, Segrott J, Jordan S (2008) Tensions and contradictions in nurses’ perspectives of evidence-based practice. J Nurs Manag 16: 440-451.
- Doody CM, Doody O (2011) Introducing evidence into nursing practice: using the IOWA model. Br J Nurs 20: 661-664.
- Schaffer MA, Sandau KE, Diedrick L (2013) Evidence-based practice models for organizational change: overview and practical applications. J Adv Nurs 69: 1197-1209.
- Brown CG (2014) The Iowa Model of Evidence-Based Practice to Promote Quality Care: an illustrated example in oncology nursing. Clin J Oncol Nurs 18: 157-159.
- Lo Biondo-Wood G, Haber J (2006) Nursing research: methods and critical appraisal for evidence-based practice (6thedn). Elsevier- Mosby, Philadelphia, USA.
- Liu JP (2007) [The composition of evidence body of traditional medicine and recommendations for its evidence grading]. Zhongguo Zhong Xi Yi Jie He Za Zhi 27: 1061-1065.
- Gawlinski A, Rutledge D (2008) Selecting a model for evidence-based practice changes: a practical approach. AACN Adv Crit Care 19: 291-300.
- Cullen L, Titler MG (2004) Promoting evidence-based practice: an internship for staff nurses. Worldviews Evid Based Nurs 1: 215-223.
- Cullen L, Titler MG, Rempel G (2011) An advanced educational program promoting evidence-based practice. West J Nurs Res 33: 345-364.
- Haxton D, Doering J, Gingras L, Kelly L (2012) Implementing skin-to-skin contact at birth using the Iowa model: applying evidence to practice. Nurs Womens Health 16: 220-229.
- Cullen L (2008) Moving from Model to Impact, 6th Annual Nursing Research Day, the Organization of Nurse Executives of New Jersey, Princeton, New Jersey, USA.
- Brod M (1998) Quality of life issues in patients with diabetes and lower extremity ulcers: patients and care givers. Qual Life Res 7: 365-372.
- Wagner FW Jr (1981) The dysvascular foot: a system for diagnosis and treatment. Foot Ankle 2: 64-122.
- Zhou WG, Xiao MY, Liang YK, Huang XY, Liu Y et al. (2015) 0 of 30 cases of diabetic foot four cents a vine decoction Foot Treatment. Guiding Journal of Traditional Chinese Medicine and Pharmacy 6: 32-35.
- Chen QQ (2014) Efficacy 0 diabetic foot three worms pink soup foot joint foot reflex zone massage. Journal of Nursing 12: 61-62.
- Zeng SY (2014) Chinese medicine Yuzu Moxibution foot massage for Wagner 0 Ji diabetic foot Efficacy. Diabetes New World 5: 25-26.
- Xing T, Qingqing C, Xuping Z (2014) Efficacy 0 diabetic foot three pink worm soup Foot Treatment. Journal of Zhejiang Chinese Medical University 5: 651-653.
- Zhen J, Ming-xin L, Yan-ling L, Xing-mei C, Shu-lin L (2013) Use of Chinese medicine external treatment of diabetic foot triple mode 0 Clinical Observation on 40 Cases. China Journal of Traditional Chinese Medicine and Pharmacy 2: 443-446.
- Zhang Q, Yang F, Xu H, Yang QY, Wang XH, et al. ( 2011) Nursing Intervention of heat and dampness detoxification square foot early diabetic foot. Clinical Journal of Traditional Chinese Medicine 23: 689-690.
- Kaylee (2011) Clinical Observation of 130 cases of diabetic foot medicine foot bath treatment. Guiding Journal of Traditional Chinese Medicine and Pharmacy 17: 40-41.
- Wang ZF, Wang BJ, Ma L (2010) Integrative Medicine at high risk of diabetic foot clinical observation. Chinese Journal of Information on Traditional Chinese Medicine 17: 53-54.
- Xu YP, Li YH (2008) Integrative treatment of diabetic foot Efficacy. China Modern Doctor 46: 73-74.
- Duan SL, Tang L, Liu Y, Chen W, Jiang YT (2016) 0 diabetic foot medicine foot care benefits Meta-analysis. Chinese Nursing Management 16: 159-163.
- Duan SL (2016) The construction of an evidence-based nursing practice protocol on the treatment of grade 0 diabetic foot ulcer with foot bath. Beijing University of Chinese Medicine, China.
Citation: Zhao J, Duan S, Liu X, Han L, Jiang Y et al. (2016) Discussion on Clinical Application of Iowa Model in TCM Nursing Care. J Altern Complement Integr Med 2: 011.
Copyright: © 2016 Junqiang Zhao, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

