
Distance Traveled for Intrapartum Care and Perinatal Outcomes in Eastern North Carolina
*Corresponding Author(s):
Kelly L Pieh HolderDepartment Of Obstetrics And Gynecology, East Carolina University, Greenville, North Carolina, United States
Tel:+1 2527444669,
Email:kellylholder@gmail.com
Abstract
Background
Current data suggests that women who travel outside of their community for perinatal care are at an increased risk of adverse outcomes.
Objectives
The objective of this study was to compare outcomes between women who live adjacent to a tertiary care center and women who need to travel for this care.
Methods
Data for all deliveries from June 2010 through October 2013 were extracted from the Delivery Database at Vidant Medical Center in Greenville, North Carolina. Subjects included women who were term, admitted for labor and residents of eastern North Carolina. Distances from the patient’s residence to the hospital were calculated and evaluated for the impact on perinatal outcomes. Analysis was performed using Chi-square, T-tests, ANOVA and Kruskal-Wallis.
Results
A total of 12,071 deliveries occurred during the study period with a total of 3,955 subjects included in the final analysis. Women who traveled for care had an increased risk of cesarean sections, operative deliveries and postpartum hemorrhage. Overall neonatal outcomes were comparable across distances.
Conclusion
The results from this study support improving access to maternity services for women from rural and remote communities.
INTRODUCTION
While the optimal travel distance for maternity care has not been established, data from a recent study by Rayburn and Richardson noted that access to perinatal care is not equal across the United States. Access to a maternity center is within a 30-minute drive for 87.5% of the US population (43.6 million) and within a 60-minute drive for 97.3% of the US population (48.4 million). Hospitals with capabilities to provide care for more complicated cases (level II or III) are less accessible within a 30-minute drive (78.6% of the population; 39.1 million) and a 60-minute drive (93.1% of the population; 46.4 million). Centers providing the most comprehensive maternal and newborn care (level III) are least accessible and located only in metropolitan areas (60.8% or 30.3 million of the population within a 30-minute drive; 80.1% or 39.9 million of the population within a 60-minute drive) [12].
More information regarding perinatal outcomes as they relate to travel distance to the hospital will improve our understanding of how to improve pregnancy outcomes in regions of limited access to adequate perinatal care. The objective of this study was to compare perinatal outcomes between women presenting in labor who live adjacent to a tertiary care center and women presenting in labor who need to travel for this care. The hypothesis was that geographic disparity exists among women delivering at a tertiary care facility and that longer distances traveled have a negative impact on perinatal outcomes.
METHODS
Driving distance from home residence to the hospital was estimated using the zip code of the woman’s residence and the zip code Vidant Medical Center. Direct line distance and driving distance were then calculated using Zipcode Database & Demographic Data and Google Maps. The distance was defined from the central location of each zip code to Vidant Medical Center. Distances were then divided into catchment areas based on proximity to the hospital. NCSS 97 software was used for statistical calculation. The Chi-square, Fisher’s exact test was used for analysis of categorical data using. T-tests and analysis of variance routines were used for numeric data and normality of data distribution was always considered. T-tests, or Student Newman Kuels tests, were used on normally distributed data. Mann-Whitney U test was used with T-testing of non-normal data.
For ANOVA analysis on non-normal data, the Kruskal-Wallis ANOVA, corrected for ties and Kruskal-Wallis multiple comparison Z value tests were used. Statistical significance was considered when P<0.05. Possible confounding factors were analyzed separately for interactions. Ethical considerations for this project were in accordance with the Vidant Medical Center and East Carolina University Institutional Review Board’s criteria for research with human subjects. All identifiable information was stripped from the data set prior to final analysis. The authors declare that there is no conflict of interest regarding the publication of this paper
RESULTS
|
Demographics |
Total |
0-15 Miles |
15-60 miles |
>60 miles |
P-Value |
|
Marital Status |
3966 |
0.116 |
|||
|
Married |
1806 (45.5%) |
925 (44%) |
781 (47%) |
100 (49%) |
|
|
Single |
2160 (54.5%) |
1175 (56%) |
881 (53%) |
104 (51%) |
|
|
Age |
3972 |
0.976 |
|||
|
Young maternal age (<19) |
399 (10%) |
209 (9.9%) |
171 (10.3%) |
19 (9.3%) |
|
|
Adult (20-34) |
3190 (80.3%) |
1685 (80.2%) |
1339 (80.4%) |
166 (81%) |
|
|
Advanced maternal age (>35) |
383 (9.6%) |
207 (9.9%) |
156 (9.4%) |
20 (9.8%) |
|
|
Parity |
3966 |
<0.001 |
|||
|
Primiparous |
1607 (40.5%) |
911 (43.4%) |
601 (36.1%) |
95 (46.6%)* |
|
|
Multiparous |
2359 (59.5%) |
1187 (56.6%) |
1063 (63.9%) |
109 (53.4%)* |
|
|
BMI |
3945 |
<0.001 |
|||
|
Normal (18.5-24.9) |
411 (10.4%) |
233 (11.1%) |
156 (9.4%) |
22 (10.8%) |
|
|
Overweight (25-29.9) |
1359 (34.4%) |
747 (35.7%) |
547 (33%) |
65 (32%) |
|
|
Obese (30-39.9) |
1750 (44.3%) |
898 (42.9%) |
766 (46.3%) |
86 (42.4%) |
|
|
Morbid obesity (40-49.9) |
363 (9.2%) |
184 (8.8%) |
161 (9.7%) |
18 (8.9%) |
|
|
Super morbid obesity (>50) |
67 (1.7%) |
29 (1.4%) |
26 (1.6%) |
12 (5.9%)* |
|
|
Race |
3995 |
<0.001 |
|||
|
Asian |
133 (3%) |
102 (5%) |
26 (2%) |
5 (2%) |
|
|
African american |
1588 (40%) |
944 (45%) |
590 (36%)* |
54 (25%)* |
|
|
Hispanic |
475 (12%) |
210 (10%) |
251 (15%) |
14 (6.9%)* |
|
|
White |
1759 (44%) |
825 (40%) |
793 (48%)* |
131 (64%)* |
|
|
Insurance Status |
3972 |
<0.001 |
|||
|
Medicaid |
2214 (55.7%) |
1145 (54.5%) |
984 (59.1%) |
85 (41.5%)* |
|
|
Private |
1641 (41.3%) |
887 (42.2%) |
638 (38.3%) |
116 (56.6%)* |
|
|
Self/Other |
117 (2.9%) |
69 (3.3%) |
44 (2.6%) |
4 (2%) |
|
Intrapartum Variables |
Total |
0-15 Miles |
15-60 miles |
>60 miles |
P-Value |
|
Reason for Admission |
3972 |
0.867 |
|||
|
Labor |
2094 (52.7%) |
1111 (52.9%) |
872 (52.3%) |
111 (54.1%) |
|
|
“Rule out Labor” |
1878 (47.3%) |
990 (47.1%) |
794 (47.7%) |
94 (45.9%) |
|
|
Presentation |
3958 |
0.04 |
|||
|
Breech |
36 (0.9%) |
23 (1.1%) |
8 (0.5%)* |
5 (2.5%)* |
|
|
Compound |
101 (2.6%) |
55 (2.6%) |
40 (2.5%) |
6 (3%) |
|
|
Cephalic |
3821 (96.5%) |
2018 (96.3%) |
1611 (97.1%)* |
192 (94.6%) |
|
|
Admit Dilation |
3968 |
0.101 |
|||
|
0-3 cm |
1218 (30.7%) |
646 (30.8%) |
496 (29.8%) |
76 (37.1%) |
|
|
4 cm or greater |
2750 (69.3%) |
1452 (69.2%) |
1169 (70.2%) |
129 (62.9%) |
|
|
Admit Dilation (Secondary Analysis) |
3960 |
0.975 |
|||
|
0-5 cm |
2890 (73%) |
1530 (73%) |
1210 (72.8%) |
150 (73.5%) |
|
|
6 cm or greater |
1070 (27%) |
565 (27%) |
451 (27.2%) |
54 (26.5%) |
|
|
Labor Duration |
3972 |
0.02 |
|||
|
163 4.1 |
83 (4%) |
65 (3.9%) |
15 (7.3%)* |
||
|
30 min - 6 hrs |
1376 (34.6%) |
728 (34.7%) |
598 (35.9%) |
50 (24.4%)* |
|
|
6-12 hours |
1443 (36.3%) |
767 (36.5%) |
596 (35.8%) |
80 (39%) |
|
|
>12 hours |
990 (24.9%) |
523 (24.9%) |
407 (24.4%) |
60 (29.3%)* |
|
|
Augmentation |
3948 |
0.362 |
|||
|
Pitocin |
1541 (39%) |
828 (39.7%) |
628 (37.8%) |
85 (41.7%) |
|
|
No augmentation |
2407 (61%) |
1256 (60.3%) |
1032 (62.2%) |
119 (58.3%) |
|
|
Analgesia |
3558 |
0.218 |
|||
|
Epidural |
1924 (54.1%) |
979 (54.3%) |
841 (53.6%) |
104 (55.9%) |
|
|
IV sedation |
402 (11.3%) |
220 (12.2%) |
163 (10.4%) |
19 (10.2%) |
|
|
Local |
31 (0.9%) |
13 (0.7%) |
14 (0.9%) |
4 (2.2%) |
|
|
None |
1201 (33.8%) |
592 (32.8%) |
550 (35.1%) |
59 (31.7%) |
|
|
Support persons |
3968 |
0.03 |
|||
|
Spouse/ Significant other |
3017 (76%) |
1604 (76.5%) |
1274(76.5%) |
139 (67.8%)* |
|
|
Parent/Guardian |
442 (11.1%) |
241 (11.5%) |
171 (10.3%) |
30 (67.8%)* |
|
|
None/Staff only |
509 (12.8%) |
252 (12%) |
221 (13.3%) |
36 (17.6%)* |
|
Maternal Outcomes |
Total |
0-15 Miles |
15-60 miles |
>60 miles |
P-Value |
|
Lacerations |
3505 |
0.263 |
|||
|
None |
1674 (47.8%) |
879 (47.2%) |
723(48.9%) |
72 (43.9%) |
|
|
First or Second |
1751 (50%) |
946 (50.8%) |
720 (48.7%) |
85 (51.8%) |
|
|
Third or Fourth |
80 (2.3%) |
38 (2%) |
35 (2.4%) |
7 (4.3%) |
|
|
Delivery Mode |
3965 |
<0.001 |
|||
|
Spontaneous |
3308 (83.4%) |
1744 (83.2%) |
1415 (85%) |
149 (72.7%)* |
|
|
Operative |
173 (4.4%) |
101 (4.8%) |
59 (3.5%) |
13 (6.3%) |
|
|
Cesarean section |
484 (12.2%) |
251 (12%) |
190 (11.4%) |
43 (21%)* |
|
|
VBAC |
249 |
0.201 |
|||
|
Successful |
194 (77.9%) |
70 (72.2%) |
107 (81.1%) |
17 (85%) |
|
|
Failed |
55 (22.1%) |
27 (27.8%) |
25 (18.9%) |
3 (15%) |
|
|
Estimate Blood Loss |
3958 |
0.05 |
|||
|
<500cc |
3411 (86.2%) |
1806 (86.2%) |
1443 (87%) |
162 (79.8%) |
|
|
500-1000cc |
478 (12.1%) |
257 (12.3%) |
187 (11.3%) |
34 (16.7%) |
|
|
>1000cc |
69 (1.7%) |
33 (1.6%) |
29 (1.7%) |
7 (3.4%) |
Maternal outcomes for comparison included route of delivery, length of labor, labor analgesia, perineal lacerations and augmentation of labor and presence of support persons. For all subjects, the mode of delivery (cesarean, operative or vaginal) was significantly associated with distance from the hospital (p<0.001). Women who lived greater than 60 miles were more likely to have been delivered by cesarean section or operative delivery. The most common indications for cesarean delivery included, in order of frequency, arrest of descent or arrest of dilation, abnormal fetal heart tracing, malpresentation, active HSV infection or HIV. Indications for cesarean section were not significantly associated with travel distance to the hospital. Further analysis revealed that for women with a history of a cesarean section, the travel distance to the hospital was not significantly associated with success or failure of a trial of labor after a cesarean section (p=0.210) (Table 2).
Length of labor and dilation at admission was significantly associated with the distance women traveled to the hospital (p<0.001). Women who were dilated 4 cm or greater at the time of admission were less likely to have labor lasting greater than 12 hours. Secondary analysis was performed using 6cm dilation which revealed similar results. Length of labor from time of admission to delivery increased as travel distance increased and the longer a woman was in labor, the more likely she was to deliver by cesarean section (Figure 1). The duration of labor was significantly associated with travel distance to the hospital (p=0.02) and women who delivered via cesarean section or operative delivery were more likely to be in labor for greater 12 hours. Women who lived >60 miles were more likely to labor 12 hours (Table 2).
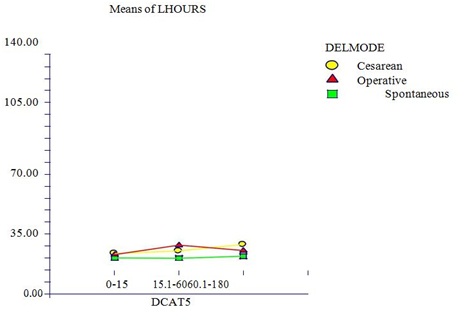 Figure 1: Length of labor, mode of delivery and distance traveled for intrapartum care in Eastern North Carolina.
Figure 1: Length of labor, mode of delivery and distance traveled for intrapartum care in Eastern North Carolina.There was an association noted between Estimated Blood Loss (EBL) and travel distance to the hospital (p=0.05). Women who traveled greater distances to the hospital were noted to have an increased risk of a postpartum hemorrhage. Women who experienced a postpartum hemorrhage with an EBL >1000cc were more likely to live >60 miles from the hospital. Lacerations were not significantly associated with distance although women who lived >60 miles, but women who traveled for care did have twice as many third- and fourth-degree perineal lacerations as those who lived in close proximity to the hospital (Table 3). A median of 39% of subjects required pitocin augmentation across all distances. There were no significant differences regarding augmentation of labor regardless of the distance traveled for Intrapartum care. There was a variety of use of pain medications and combinations of pain medications. Use of pain medication revealed no significant differences in relationship to travel distance to the hospital (p=0.218). Twice as many women who lived greater than 60 miles were more likely to lack support during labor (p=0.03) (Table 2).
Neonatal outcomes for comparison included Apgar scores, nursery admission, birth weight and estimated gestational age. Apgar scores are universally used as an indicator of the neonate’s condition in the first few minutes after delivery. An apgar score of less than seven is frequently associated with the need for resuscitative measures. Therefore, analysis was performed using an apgar score of seven. A one minute apgar score of less than seven was noted to be significantly associated with increased travel distance to the hospital (p<0.001). Women coming from >60 miles were more likely to have 5 minute apgar scores of less than seven versus those who lived 60 miles did have a higher percentage of infants admitted to the intermediate unit and neonatal intensive care unit. Infants were subdivided into three categories based on birth weight: low birth weight (4000 grams). Infants were also divided into four categories based on gestational age: early term (37-38.6 weeks), term (39-40.6 weeks), late term (41-41.6 weeks) and post-term (>42 weeks). Neither gestational age nor birth weight was significantly associated with travel distance to the hospital. Further analysis did show that super morbidly obese patients were more likely to have infants >4000 grams (p<0.001) (Table 4).
|
Neonatal Outcomes |
Total |
0-15 Miles |
15-60 miles |
>60 miles |
P-Value
|
|
Nursery Care |
3971 |
0.078 |
|||
|
Newborn |
3658 (92.1%) |
1941 (92.4%) |
1538 (92.3%) |
179 (87.3%) |
|
|
Intermediate |
218 (5.5%) |
106 (5%) |
94 (5.6%) |
18 (8.8%) |
|
|
NICU |
95 (3.9%) |
53 (2.5%) |
34 (2%) |
8 (3.9%) |
|
|
One Minute APGAR Score |
3966 |
<0.001 |
|||
|
<7 |
450 (11.3%) |
255 (12.2%)* |
158 (9.5%) |
37 (18%)* |
|
|
>7 |
3516 (88.7%) |
1842 (87.8%)* |
1506 (90.5%) |
168 (82%)* |
|
|
Five Minute APGAR Score |
3971 |
0.064 |
|||
|
<7 |
75 (1.9%) |
41 (2%) |
26 (1.6%) |
8 (3.9%) |
|
|
>7 |
3896 (98.1%) |
2060 (98%) |
1639 (98.4%) |
197 (96.1%) |
|
|
Birth Weight |
3959 |
0.537 |
|||
|
100 (2.5%) |
51 (2.4%) |
41 (2.5%) |
8 (3.9%) |
||
|
2500-4000 grams |
3585 (90.6%) |
1908 (91.1%) |
1497 (90.2%) |
180 (88.2%) |
|
|
>4000 grams |
274 (6.4%) |
136 (6.5%) |
122 (7.3%) |
16 (7.8%) |
|
|
Estimated Gestational Age |
3972 |
0.285 |
|||
|
Early term (37-38.6) |
1176 (29.6%) |
602 (28.7%) |
507 (30.4%) |
67 (32.7%) |
|
|
Term (39-40.7) |
2592 (65.3%) |
1397 (66.5%) |
1068 (64.1%) |
127 (62%) |
|
|
Late term (41-41.6) |
198 (5%) |
101 (4.8%) |
86 (5.2%) |
5 (0.3%) |
|
|
Post term (>42 weeks) |
6 (0.2%) |
1 (0%) |
5 (0.3%) |
0 (0%) |
DISCUSSION
The results from this study show that women who travel greater distances for Intrapartum care have an increased risk of adverse perinatal outcomes. For example, women traveling greater than 60 miles were at a higher risk for a cesarean section or operative delivery and postpartum hemorrhage. As mentioned above, the most common indications for cesarean delivery in this study included arrest of descent of arrest of dilation, abnormal fetal heart tracing, malpresentation or active HSV infection or HIV. These results are consistent with a 2011 population-based study which noted that the most common indications for primary cesarean delivery included labor dystocia, abnormal fetal heart rate tracing, fetal malpresentation, multiple gestation and suspected fetal macrosomia [16].
The presence of a support person during labor has been associated with improved perinatal outcomes. A Cochrane review including 23 trials involving more than 15,000 women concluded that women who receive continuous labor support are more likely to have a spontaneous vaginal delivery, less likely to use pain medications and have slightly shorter labors and to have infants who were also less likely to have low five minute apgar scores [17]. The decreased support during labor which was noted among women traveling greater distances for Intrapartum care may have been a contributing factor to the increased risk of cesarean section among this population. Maternal obesity has also been associated with adverse perinatal outcomes such as increased risk of cesarean and operative deliveries [18]. In this study, increasing maternal obesity was associated with greater distances from the hospital and may have contributed to the increased risk of cesarean and operative deliveries among this population. In addition to the increased risk of operative delivery, maternal obesity has been associated with an increased risk of postpartum hemorrhage [19]. In this study, women who traveled greater than 60 miles for Intrapartum care had an increased risk of a postpartum hemorrhage. In addition to maternal obesity, the increased risk of cesarean sections and operative deliveries, the increased risk of rapid or prolonged labor and the increased percentage of third and fourth degree perineal lacerations among this population may have also contributed to the increased in postpartum hemorrhages.
Race was noted to be associated with travel distance to the hospital in this study and the racial disparities were similar to what has previously been reported. Prior studies have noted that Native-American women had the lowest percentage of living within a 30-minute drive (68.2%) or a 60-minute drive (83.2%) of the nearest perinatal center, while Hispanic and African American women lived the closest to targeted hospitals [12]. Similarly, in this study Caucasian women were more likely to live >60 miles from the hospital while Asian, African American and Hispanic women tended to live <60 miles from the hospital.
The strengths of this study include the use of a large database to investigate the association between travel distance to the hospital and perinatal outcomes. Another strength is that this study included subjects from a variety of providers including academic obstetricians and family medicine physicians, private obstetricians and nurse-midwives, therefore taking into account various practice patterns. Because the exact location of the onset of labor was unknown, the zipcode of the location of residence on the delivery record was used for calculating distance to the hospital. The type of transportation used (i.e., car versus ambulance) and individual situations are unknown and could not be taken into account. Therefore, actual travel times may be variable. The associations found in a study such as this are not necessarily causal. It is possible that the effects of some important confounding factors such as maternal or fetal comorbidities were missed, although this is less likely in women presenting in labor at term. Finally, this study population from Eastern North Carolina may not be representative of the population as a whole.
CONCLUSION
Many rural women experience poor geographic access to adequate maternity care. A shortage and maldistribution of health care providers and the closing of many maternity care facilities across the country in rural communities are creating increasing disparities for rural women. The results from this study indicate that there may be an increased risk of either very short or prolonged duration of labor, an increased risk of cesarean and operative deliveries and an increased risk of postpartum hemorrhage. The results also indicated that overall neonatal outcomes were similar across all distances. Identification of travel distance for perinatal care as a potential health care disparity is one of the first steps toward directing interventions in order to improve access to maternity services for women from rural and remote communities and improve maternal and neonatal outcomes.
REFERENCES
- Grzybowski S, Stoll K, Kornelsen J (2011) Distance matters: A population based study examining access to maternity services for rural women. BMC Health Serv Res 11: 147.
- Ravelli AC, Jager KJ, de Groot MH, Erwich JJ, Rijninks-van Driel GC, et al. (2011) Travel time from home to hospital and adverse perinatal outcomes in women at term in the Netherlands. BJOG 118: 457-465.
- Mine Y, Babazono A (2004) [Regional differences in perinatal mortality rates in Japan--an investigation based on vital statistics]. Nippon Eiseigaku Zasshi 59: 342-348.
- Pilkington H, Blondel B, Drewniak N, Zeitlin J (2014) Where does distance matter? Distance to the closest maternity unit and risk of foetal and neonatal mortality in France. Eur J Public Health 24: 905-910.
- Dietsch E, Shackleton P, Davies C, Alston M, McLeod M (2010) 'Mind you, there's no anaesthetist on the road': Women's experiences of labouring en route. Rural Remote Health 10: 1371.
- Combier E, Chareire H, Le Vaillant M, Michaut F, Ferdynus C, et al. (2013) Perinatal health inequalities and accessibility of maternity services in a rural French region: closing maternity units in Burgundy. Health Place 24: 225-233.
- Kornelsen J, Moola S, Grzybowski S (2009) Does distance matter? Increased induction rates for rural women who have to travel for intrapartum care. J Obstet Gynaecol Can 31: 21-27.
- Kornelsen J, Stoll K, Grzybowski S (2011) Stress and anxiety associated with lack of access to maternity services for rural parturient women. Aust J Rural Health 19: 9-14.
- Declerque JL, Freedman JA, Verbiest S, Bondurant S (2004) North Carolina's infant mortality problems persist: Time for a paradigm shift. NC Med J 65: 138-142.
- Gould JB, Sarnoff, R, Liu H, Bell DR, Chavez G (1999) Very low birth weight births at non-NICU hospitals: the role of sociodemographic, perinatal, and geographic factors. J Perinatol 19: 197-205.
- Nesbitt T, Connell F, Hart G, Rosenblatt R (1990) Access to Obstetric Care in Rural Areas: Effect on Birth Outcomes. Am J Public Health 80: 814-818.
- Rayburn WF, Richards ME, Elwell EC (2012) Drive Times to Hospitals with Perinatal Care in the United States. Obstet Gynecol 119: 611-616.
- East Carolina University. Center for Health Systems Research and Development. Regional Health Status, Massachusetts, USA.
- Triche BJL (1991) Who Will Take Care of Our Mothers? Pg no: 1-25.
- Gray CL (2011) The Pregnancy Medical Home: use of the power of the Medicaid program to improve the standard of care across North Carolina. NC Med J 72: 232-233.
- Barber EL, Lundsberg LS, Belanger K, Pettker CM, Funai EF, et al. (2011) Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol 118: 29-38.
- Hodnett ED, Gates S, Hofmeyr GJ, Sakala C (2013) Continuous support for women during childbirth. Cochrane Database Syst Rev 7: 003766.
- Crane JM, Murphy P, Burrage L, Hutchens D (2013) Maternal and perinatal outcomes of extreme obesity in pregnancy. J Obstet Gynaecol Can 35: 606-611.
- Blomberg M (2011) Maternal obesity and risk of postpartum hemorrhage. Obstet Gynecol 118: 561-568.
Citation: Holder KLP (2019) Distance Traveled for Intrapartum Care and Perinatal Outcomes in Eastern North Carolina. J Reprod Med Gynecol Obstet 4: 016.
Copyright: © 2019 Kelly L Pieh Holder, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

