
Journal of Non Invasive Vascular Investigation Category: Clinical
Type: Research Article
Clinical-Imaging Features of Venous Strokes
*Corresponding Author(s):
Belova Liudmila AnatolyevnaDepartment Of Neurology, Neurosurgery, Physical Therapy And Physiotherapy Exercises, Ulyanovsk State University (FSEI HE USU), FSEI HE USU; 42, L. Tolstoy St., Ulyanovsk, 4320176, Russian Federation
Tel:+79084905015,
Email:labelova@mail.ru
Received Date: Jun 06, 2016
Accepted Date: Aug 30, 2016
Published Date: Sep 13, 2016
Abstract
Purpose: To define clinical and neuroimaging characteristics of venous stroke.
Materials and methods: 84 patients with clinical signs of acute stroke and constitutional venous insufficiency were examined. Clinical criteria constitutional venous insufficiency was the presence of complaints caused by venous cerebral blood circulation, the presence of several typical localizations of venous pathology (varicose and thrombosis of the veins of the lower extremities, hemorrhoids, varicocele and varicose veins of the esophagus), family “venous” history. It was revealed that 20 of them are suffering from venous stroke and 64 - from arterial stroke. Verification of diagnosis was made out by the methods of neuroimaging.
Results: The age in the studied groups was statistically significant and different in the group of patients with venous stroke [52, 7 (41; 64) years] in comparison with arterial stroke [65, 3 (45; 80) years] in distribution of patients on sex the prevalence of women has been revealed in comparison with men in the venous stroke group. The onset of clinical manifestations occurred in the compared groups unequally: sub acute, slow progression of the disease within more than 48 hours was noted in the group of patients with venous stroke in 80% and in the group of patients with arterial stroke in 25% cases. The main symptom, along with focal symptoms, was a headache. During venous stroke it had diffuse character and progressed within a few days or even weeks. Patients with arterial stroke showed complaints to headaches “as a hoop”, pressing or the gripping character more often. However, the severity of headaches in patient with venous stroke was statistically significantly higher than in patients with arterial stroke (?< 0.05). During venous stroke there is a trend of relatively rapid regression of general cerebral symptoms. In the clinical picture of the disease of patients with venous stroke a significant place is occupied by the symptoms that indicate cerebral venous circulatory distress. According to magnetic resonance imaging findings, parietal-occipital region are most commonly tends to affect in the group of patients with venous stroke (in 70% cases). Magnetic resonance signal lesion venous stroke is in most cases heterogeneous. A distinctive feature of venous stroke is the presence of signs of vasogenic cerebral edema by magnetic resonance modes DWI and ADC-mapping in the first days of the disease (in 80% cases in patients with venous stroke and in patients with arterial stroke - in 39.4%).
Conclusion: Venous stroke developed in patients at rather young age and more often in women. The clinical picture of a venous stroke is characterized by: a sub acute, slow development of clinical manifestations; the prevalence of cerebral symptoms and signs over focal; the presence of symptoms testifying to venous cerebral discirculation; a tendency to relatively fast regress of cerebral symptoms and signs. According to magnetic resonance imaging findings, in case of a venous stroke the localization of venous stroke does not coincide with blood supply “districts” of the main intracranial arteries; the shape of foci is irregular and boundaries are uneven and indistinct. The signs of cerebral venous discirculation are visualized as well as intracranial venous stasis and vasogenic edema.
Materials and methods: 84 patients with clinical signs of acute stroke and constitutional venous insufficiency were examined. Clinical criteria constitutional venous insufficiency was the presence of complaints caused by venous cerebral blood circulation, the presence of several typical localizations of venous pathology (varicose and thrombosis of the veins of the lower extremities, hemorrhoids, varicocele and varicose veins of the esophagus), family “venous” history. It was revealed that 20 of them are suffering from venous stroke and 64 - from arterial stroke. Verification of diagnosis was made out by the methods of neuroimaging.
Results: The age in the studied groups was statistically significant and different in the group of patients with venous stroke [52, 7 (41; 64) years] in comparison with arterial stroke [65, 3 (45; 80) years] in distribution of patients on sex the prevalence of women has been revealed in comparison with men in the venous stroke group. The onset of clinical manifestations occurred in the compared groups unequally: sub acute, slow progression of the disease within more than 48 hours was noted in the group of patients with venous stroke in 80% and in the group of patients with arterial stroke in 25% cases. The main symptom, along with focal symptoms, was a headache. During venous stroke it had diffuse character and progressed within a few days or even weeks. Patients with arterial stroke showed complaints to headaches “as a hoop”, pressing or the gripping character more often. However, the severity of headaches in patient with venous stroke was statistically significantly higher than in patients with arterial stroke (?< 0.05). During venous stroke there is a trend of relatively rapid regression of general cerebral symptoms. In the clinical picture of the disease of patients with venous stroke a significant place is occupied by the symptoms that indicate cerebral venous circulatory distress. According to magnetic resonance imaging findings, parietal-occipital region are most commonly tends to affect in the group of patients with venous stroke (in 70% cases). Magnetic resonance signal lesion venous stroke is in most cases heterogeneous. A distinctive feature of venous stroke is the presence of signs of vasogenic cerebral edema by magnetic resonance modes DWI and ADC-mapping in the first days of the disease (in 80% cases in patients with venous stroke and in patients with arterial stroke - in 39.4%).
Conclusion: Venous stroke developed in patients at rather young age and more often in women. The clinical picture of a venous stroke is characterized by: a sub acute, slow development of clinical manifestations; the prevalence of cerebral symptoms and signs over focal; the presence of symptoms testifying to venous cerebral discirculation; a tendency to relatively fast regress of cerebral symptoms and signs. According to magnetic resonance imaging findings, in case of a venous stroke the localization of venous stroke does not coincide with blood supply “districts” of the main intracranial arteries; the shape of foci is irregular and boundaries are uneven and indistinct. The signs of cerebral venous discirculation are visualized as well as intracranial venous stasis and vasogenic edema.
Keywords
Functional state; Magnetic resonance imaging; Neurologic deficiency; Venous stroke
INTRODUCTION
A Venous Stroke (VS) is considered to be “relatively unknown cerebrovascular disease” [1] and occurs, according to recommendations of the American Heart Association/American Stroke Association, in 0.5-1% of all strokes [2]. In 78% of cases venous strokes occur in patients to 50 years of age and in 3 times more often in females [3].
Thrombophilia, oncological diseases, inflammatory diseases, postoperative period, injuries, dehydration, CNS infections, arteriovenous malformation, polycythemia, thrombocytemia, anemia, vasculitis, systemic lupus erythematosus, rheumatoid arthritis, sarcoidosis, diseases of the thyroid gland are referred to states and conditions which are the risk factors of developing cerebral venous thrombosis [2,4-6].
The disability level with this pathology is about 5-10% of patients, mortality rate from 3 to 15% [7].
VS morphologically differs from arterial one in the fact that congestion, stasis, diapedetic hemorrhages and also small foci of necrosis characterizing it are not accompanied by pathological changes of arteries in the affected area. Ischemia bears a secondary character associated with externally caused vessel constriction feeding the area of stasis [8]. Edema which in case of VS has a more marked character is the factor predisposing to hemorrhage. Pathophysiological mechanisms of the brain injury in the acute period of VS are characterized by congestion and vasogenic edema unlike ischemia and cytotoxic edema in case of an arterial stroke [9]. Some authors number manifestations of vasogenic edema earlier than cytotoxic one among the features of VS [10].
Typical of VS is early hemorrhagic transformation associated with venous stasis and development of vasogenic edema of the brain [10] which is registered 3 times more often in case of VS than in case of Arterial Stroke (AS) [11,12].
Diagnosis of cerebral venous thrombosis and VS is based on the clinical data and confirmation by neuroimaging methods [2].
Magnetic Resonance Imaging (MRI) of the brain in combination with MR-venography are the most sensitive examination methods for detecting cerebral venous thromboses in acute, sub acute and chronic phases [5,13,14].
Determination of the venous character of a stroke leads to a change of the therapy tactics [15] therefore suspicions of this disease that may arise already at the evaluation stage of a clinical picture is an important component of diagnostics and subsequent neuroimaging has to provide the diagnosis verification [9].
Proceeding from all the aforesaid, the purpose of our study was to determine clinical-imaging features of VS.
Thrombophilia, oncological diseases, inflammatory diseases, postoperative period, injuries, dehydration, CNS infections, arteriovenous malformation, polycythemia, thrombocytemia, anemia, vasculitis, systemic lupus erythematosus, rheumatoid arthritis, sarcoidosis, diseases of the thyroid gland are referred to states and conditions which are the risk factors of developing cerebral venous thrombosis [2,4-6].
The disability level with this pathology is about 5-10% of patients, mortality rate from 3 to 15% [7].
VS morphologically differs from arterial one in the fact that congestion, stasis, diapedetic hemorrhages and also small foci of necrosis characterizing it are not accompanied by pathological changes of arteries in the affected area. Ischemia bears a secondary character associated with externally caused vessel constriction feeding the area of stasis [8]. Edema which in case of VS has a more marked character is the factor predisposing to hemorrhage. Pathophysiological mechanisms of the brain injury in the acute period of VS are characterized by congestion and vasogenic edema unlike ischemia and cytotoxic edema in case of an arterial stroke [9]. Some authors number manifestations of vasogenic edema earlier than cytotoxic one among the features of VS [10].
Typical of VS is early hemorrhagic transformation associated with venous stasis and development of vasogenic edema of the brain [10] which is registered 3 times more often in case of VS than in case of Arterial Stroke (AS) [11,12].
Diagnosis of cerebral venous thrombosis and VS is based on the clinical data and confirmation by neuroimaging methods [2].
Magnetic Resonance Imaging (MRI) of the brain in combination with MR-venography are the most sensitive examination methods for detecting cerebral venous thromboses in acute, sub acute and chronic phases [5,13,14].
Determination of the venous character of a stroke leads to a change of the therapy tactics [15] therefore suspicions of this disease that may arise already at the evaluation stage of a clinical picture is an important component of diagnostics and subsequent neuroimaging has to provide the diagnosis verification [9].
Proceeding from all the aforesaid, the purpose of our study was to determine clinical-imaging features of VS.
MATERIALS AND METHODS
84 patients with clinical manifestations of acute stroke have been examined. There were 32 males among them aged from 41 to 80 years (mean age of 60±10.9 years) and 52 females aged from 48 to 80 years (mean age 62±10.3 years). The mean age of all patients was 61±10.4 years.
VS was diagnosed in 20 of 84 patients by means of MRI methods, the remaining number of 64 patients had AS.
The severity assessment of neurologic symptoms and signs in patients was carried out by means of the stroke scale of the National Institute of Health (NIHSS-National Institutes of Health Stroke Scale). Barthel Index (BI) was applied to determine the level of life activity. To assess a functional condition of patients the Rankin Scale (RS) was used. A subjective assessment of severity of headaches was carried out by means of the Visual Analog Scale (VAS) (Huskisson EC, 1974).
Verification of the diagnosis was performed by neuroimaging methods in all cases. MRI was carried out by means of the device siemens magnetom symphony equipped with the superconducting magnetic system with a field force of 1.5 Tesla. MR imaging was performed by a standard technique in axial, sagittal and coronal projections with application of pulse sequences T2, T1, FLAIR and DW programs.
Localization and boundaries of the focus, the relation of the intracranial vessels to districts were determined, the signs of volumetric influence and midline shift, the amount of damage were assessed by T2VS, FLAIR, DWI and according to ADC cards (b=0, 500, 1000), the characteristics of edema in the focus (vasogenic or cytotoxic) according to measurement of the MR signal of DWI and ADC cards.
To analyze tomographic images the data were used in the DICOM 3.0 format. Measurement of rectilinear distances was taken by means of standard software of the graphic station “eFilmWorkstation 3.4”.
The statistical analysis of the obtained results was carried out with use of a package of the Statistical 10.0 application programs. The obtained data were presented in the form [Me (25%; 75%)].
VS was diagnosed in 20 of 84 patients by means of MRI methods, the remaining number of 64 patients had AS.
The severity assessment of neurologic symptoms and signs in patients was carried out by means of the stroke scale of the National Institute of Health (NIHSS-National Institutes of Health Stroke Scale). Barthel Index (BI) was applied to determine the level of life activity. To assess a functional condition of patients the Rankin Scale (RS) was used. A subjective assessment of severity of headaches was carried out by means of the Visual Analog Scale (VAS) (Huskisson EC, 1974).
Verification of the diagnosis was performed by neuroimaging methods in all cases. MRI was carried out by means of the device siemens magnetom symphony equipped with the superconducting magnetic system with a field force of 1.5 Tesla. MR imaging was performed by a standard technique in axial, sagittal and coronal projections with application of pulse sequences T2, T1, FLAIR and DW programs.
Localization and boundaries of the focus, the relation of the intracranial vessels to districts were determined, the signs of volumetric influence and midline shift, the amount of damage were assessed by T2VS, FLAIR, DWI and according to ADC cards (b=0, 500, 1000), the characteristics of edema in the focus (vasogenic or cytotoxic) according to measurement of the MR signal of DWI and ADC cards.
To analyze tomographic images the data were used in the DICOM 3.0 format. Measurement of rectilinear distances was taken by means of standard software of the graphic station “eFilmWorkstation 3.4”.
The statistical analysis of the obtained results was carried out with use of a package of the Statistical 10.0 application programs. The obtained data were presented in the form [Me (25%; 75%)].
RESULTS
The diagnosis of VS is based on the clinical data confirmed by MRI images. A clinical picture was associated with an increase of the intra cranial pressure caused by venous outflow impairment and focal neurologic symptoms and signs. The character and prognosis of the disease are influenced, as a rule, by age and sex of a person.
The age in the studied groups was statistically significant and different in the group of patients with VS [52.7 (41; 64) years] in comparison with AS [65.3 (45; 80) years] (? <0.05). Thus, VS, unlike AS, develops in patients at a younger age.
In distribution of patients on sex the prevalence of women has been revealed in comparison with men in the VS group (?< 0.05) (Figure 1).
The age in the studied groups was statistically significant and different in the group of patients with VS [52.7 (41; 64) years] in comparison with AS [65.3 (45; 80) years] (? <0.05). Thus, VS, unlike AS, develops in patients at a younger age.
In distribution of patients on sex the prevalence of women has been revealed in comparison with men in the VS group (?< 0.05) (Figure 1).
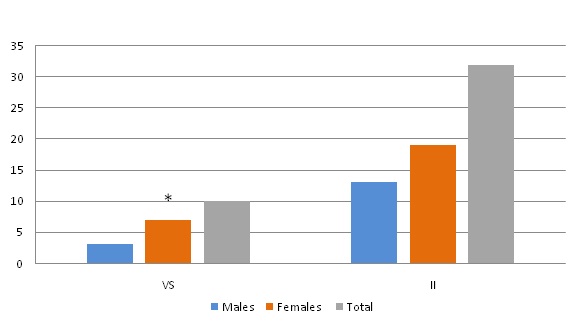
Figure 1: Sex distribution of patients.
The onset of clinical manifestations occurred in the compared groups unequally: sub acute, slow progression of the disease within several days (more than 48 hours) was noted in the group of patients with VS in 80%, and in the group of patients with AS in 25% cases.
Complaints of a headache often occurred in patients with VS and AS equally (p<0.05). The headache was the most common symptom of VS and was present in all patients. In case of VS it had a diffusion character and in case of AS progressed within several days or even weeks. In patients with VS in 63.4% of cases the headache was limited to the occipital area, in 34.2% of patients was of a diffusion character, in 12.4% - bursting headache. In 52.8% of cases the headache was dull and monotonous. Patients with AS, made complaints of hoop-like headaches (33.4%) of pressing (44.9%) or squeezing (51.1%) character. However, headache pain severity in patients with VS was much higher than in patients with AS. In case of VS the score point was 7.5 (3; 9), in case of AS it was 4.9 (1; 7) on the VAS (?< 0.05).
Assessing “venous” complaints [16], it was found that in the VS group in comparison with AS these symptoms occurred more often among statistically significant (?< 0.05) (Table 1).
The onset of clinical manifestations occurred in the compared groups unequally: sub acute, slow progression of the disease within several days (more than 48 hours) was noted in the group of patients with VS in 80%, and in the group of patients with AS in 25% cases.
Complaints of a headache often occurred in patients with VS and AS equally (p<0.05). The headache was the most common symptom of VS and was present in all patients. In case of VS it had a diffusion character and in case of AS progressed within several days or even weeks. In patients with VS in 63.4% of cases the headache was limited to the occipital area, in 34.2% of patients was of a diffusion character, in 12.4% - bursting headache. In 52.8% of cases the headache was dull and monotonous. Patients with AS, made complaints of hoop-like headaches (33.4%) of pressing (44.9%) or squeezing (51.1%) character. However, headache pain severity in patients with VS was much higher than in patients with AS. In case of VS the score point was 7.5 (3; 9), in case of AS it was 4.9 (1; 7) on the VAS (?< 0.05).
Assessing “venous” complaints [16], it was found that in the VS group in comparison with AS these symptoms occurred more often among statistically significant (?< 0.05) (Table 1).
| Complaints | VI (n=20) | AI(n=64) |
| n (%) | n (%) | |
| Symptom of «tightcollar» | 8 (80)* | 14 (43.75) |
| Symptom of «highpillow» | 9 (90)* | 15 (46.9) |
| Symptom «sand in the eyes» | 9 (90)* | 17 (53.1) |
| Edema of the face and eyelids in the morning hours | 8 (80)* | 13 (40.6) |
The focal neurologic symptoms and signs have been caused by topography of the focal injury of the brain. Any focal symptoms typical of VS only have not been revealed. Nevertheless the onset of the disease in three patients was characterized by the cognitive functions impairment. Relatives paid attention to a decrease of mental activity within several weeks, deterioration in time and space orientation, “strange behavior” in their relatives. It made them ask for assistance and at MRI examination the signs of symmetric cerebral venous thrombosis in the field of thalamus.
It is known that drainage function disorder from the deep vein system can lead to a bilateral thalamic infarction with alteration in the level of consciousness without the presence of focal neurologic signs and symptoms. At the same time neuropsychological disorders can have a persistent character. At the same time restoration, as a rule, is favorable [2,16].
Statistically significant differences in neurologic deficit severity and functional state of patients in the compared groups have not been obtained (?> 0.05) (Table 2).
| Criteria | VS (n=20) | AS (n=64) | |
| NIHSS scale | on admission | 9.0 (6;13) | 11 (7;16) |
| on discharge | 4.0 (2;5) | 6.5 (3;9) | |
| Rankin scale | on admission | 4.0 (3;6) | 5.5 (3;8) |
| on discharge | 3.0 (1;4) | 3.5 (1;6) | |
| Barthel index | on admission | 38.0 (12;68) | 41 (10;71) |
| on discharge | 75 (45;90) | 65 (40;90) | |
In progression of VS the tendency to faster regress of focal and cerebral signs and symptoms has been noted [2]. On discharge of patients we assessed quality indicators by four criteria: improvement, without dynamics, deterioration and death. There was a tendency to more frequent cases of improvement in a patient’s state in case of VS (80%) in comparison with AS (65.7%). However, statistically significant differences were not revealed by these criteria between groups (?>0.05).
In the group of VS a focal lesion of the brain was localized in 30% in the frontal and parietal areas and in 70% of parietal and occipital lobes of the brain.
In the group of AS localization of the lesion focus was dependent on the vascularization zone of the affected artery: when the median cerebral artery was occluded the focus was localized in the parietal lobe (18.8%) and in parietal and temporal areas (31.3%), in subcortical nuclei - (18.8%); with occlusion of the anterior cerebral artery - in frontal and parietal areas (15.6%); with the posterior cerebral artery occlusion - in the occipital lobe (9.4%).
In 80% of cases on MR images (T2VI, FLAIR) the focus shape of VS was irregular, and the boundaries were uneven and indistinct. Relatively equal boundaries of the VS foci were noted only in 2 cases. In case of AS the boundaries of the foci in most cases were equal and distinct.
A non-uniform character of the foci with the mixed signal at VS was observed in 70% of cases. There were hypo intensive sites in the setting of the hyper intensive focus in general. Hypo intensive sites were localized both in the focus center (57%), and on the periphery (43%). At AS the MR-signal was mainly uniform (in 75% of cases).
The infarction focus sizes have been determined on all diagnostic tomographic images (T2VI, FLAIR, DWI, ADC) obtained in the study. The focus size at VS was 7.5 cm2 (1.85; 15.8), in case of AS 9.5 cm2 (1.5; 30.5). Statistically significant differences in relation to the area of the brain infarction focus in the VS group in comparison with AS were not revealed (?> 0.05).
A distinctive feature of the lesion focus at VS was the presence of vasogenic edema symptoms according to MRI in the first days of disease. According to the DWI MR-modes and ADC mapping in 80% cases in patients with VS the symptoms of vasogenic edema were observed in the first days of disease, in patients with AS - in 39.4% (?< 0.05).
In the analysis of results of MRI technique directed towards the examination of the venous bed variants of the structure in the system of cerebral venous outflow have been revealed. Statistically significant results were found more often in groups with VS (100%) and in comparison with AS (66.6%) (p<0.05) (Table 3).
| MRI features | VS (n=20) | AS (n=64) | |
| n (%) | n (%) | ||
| Symmetry of branches in transverse and sigmoid sinuses | - | 4 (6.25) | |
| Anatomic variants of the structure | 20 (100) | 60 (93.75) | |
| Asymmetry | Total | 8 (40) | 22 (36.7) |
| D>S | 6 (75)" | 14 (63.6) " | |
| S>D | 2 (25) | 8 (36.4) | |
| Hypoplasia | Total | 12 (60) | 38 (63.3) |
| Right sinuses | 4 (33.3) | 12 (31.6) | |
| Left sinuses | 8 (66.6) # | 26 (68.4) # | |
Note: # -statistically significant differences with hypoplasia of the right transverse sinus; " - statistically significant differences with S>D
Hypoplasia of the left transverse sinus in comparison with hypoplasia of the right transverse sinus occurred more often in all the groups, at the same time differences reached statistical importance in VS and AS groups (?<0.05) (Table 3).
In asymmetry of transverse sinus the prevalence of the right transverse sinuses over left was revealed in both compared groups (?<0.05). Diameter reductions of transverse and sigmoid sinuses were followed by a compensatory dilatation of contralateral venous structures (Table 4). Size alterations of sigmoid sinuses completely corresponded to that of transverse sinuses. The symmetric structure of transverse and sigmoid sinuses remained statistically significant more often in patients with AS (?<0.05).
Superficial veins of the brain (including v.Rolandi, v.Trolard and inferior anastomotic veins) in patients with VS were more significant statistically compared with AS (p<0.05). In the VS group also an increase in the sizes of tentorial sinus (p<0.05) was established (Table 4).
| MRI features | VS(n=10) | AS(n=32) |
| Superiorsagittal sinus (mm) | 6.3 (5.2; 7.5) | 6.3 (5.1;7.3) |
| Superficial cerebral veins (mm) | 4.6 (3.4;5.6)* | 3.8 (2.6; 4.9) |
| Tentorial sinus (mm) | 2.8 (1.8; 3.5)* | 1.8 (1.1; 2.4) |
| Right transverse sinus (mm) | 6.5 (3.0;10.4) | 6.8 (2.9;10.5) |
| Left transverse sinus (mm) | 6.0 (3.2; 9.1) | 6.1 (2.8; 9.4) |
| Right sigmoid sinus (mm) | 7.9 (3.9; 12.0) | 7.7 (4.0; 11.4) |
| Left sigmoid sinus (mm) | 7.0 (3.7; 10.8) | 7.2 (3.8; 11.0) |
Note: * - p<0.05- statistically significant differences of values between the groups.
Thromboses of transverse and sigmoid sinuses in a chronic stage have been visualized and have been statistically significant more often in VS groups and in comparison with AS (p<0.05) (Figure 2).
Thromboses of transverse and sigmoid sinuses in a chronic stage have been visualized and have been statistically significant more often in VS groups and in comparison with AS (p<0.05) (Figure 2).

Figure 2: Thrombosis of transverse and sigmoid sinuses in a chronic stage.
Typical MR images of the patients with venous stroke are shown in the figures 3-6.
Typical MR images of the patients with venous stroke are shown in the figures 3-6.
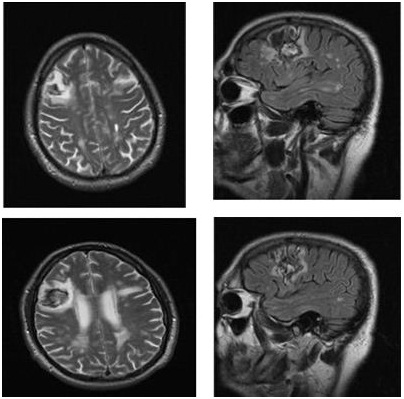
Figure 3: Patient G., 58 years old. A venous infarction of the right frontal lobe. Modes T2 and FLAIR. In the white and the gray matter of the right parietal lobe there is an irregular-shaped area of uneven and indistinct contours and a heterogeneous signal in all modes with the signs of hemosiderin presence (hemorrhagic transformation), surrounded by a vasogenic edema.
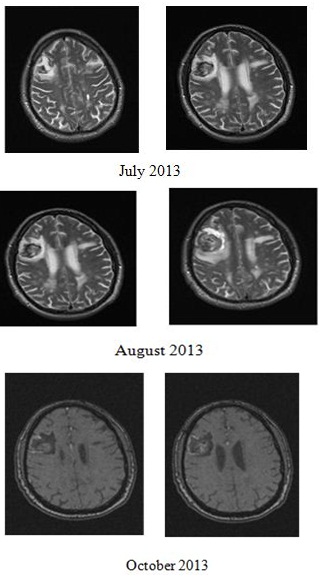
Figure 4: Patient G., 58 years old. A venous infarction of the right frontal lobe. Follow-up (after 1.2 and 4 months). In the area of infarction there is a gradual regression of the vasogenic edema and the cystic glial changes.

Figure 5: Patient B., 38 years old. A venous infarction of the left parietal lobe. In the white and the gray matter of the left parietal lobe there is an irregular-shaped area of with uneven and indistinct contour and a heterogeneous signal in all modes with the signs of hemosiderin presence (an increase of the signal in modes T1 and FLAIR, a reduction in T2 mode), surrounded by a vasogenic edema, and accumulating a contrast preparation according to a gyral type. ADC-mapping shows an increase of a signal from the right parietal lobe (vasogenic edema sign).
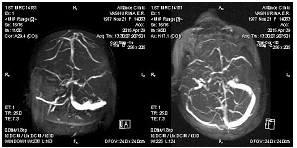
Figure 6: Patient B., 38 years old. An early chronic stage of the left vena Trolard thrombosis, marked by an asymmetry of the cerebral venous network mostly in the left hemisphere, hypoplasia of the transverse and the right sigmoid sinuses, the right internal jugular vein. MR-venography (2D-TOF technique).
The presented results have been obtained by Ulyanovsk State University in the course of performing the state assignment of the RF Ministry of Education and Science.
CONCLUSIONS
- VS develop in patients at rather young age and more often in women
- Sub acute, slow development of clinical manifestations is characteristic of VS
- In a clinical picture of VS cerebral symptoms and signs prevail over focal. Any focal symptoms inherent in VS only were not revealed. Focal neurologic deficiency is caused by focal damage topography of the brain
- The symptoms identifying venous cerebral discirculation occupy an essential place in patients with VS in a clinical picture of the disease
- A tendency of rather fast regress of cerebral symptoms and signs has been noted in progression of VS
- Localization of VS does not coincide with blood supply “districts” of the main intracranial arteries, the parietal and occipital area being affected more often
- The shape of the cerebral infarction foci in venous strokes, as a rule, is irregular, and the boundaries are uneven and indistinct. MR signal of the venous infarction focus in most cases is heterogeneous
- A distinctive feature of VIS is the presence of vasogenic edema symptoms according to MRI on the first days of the disease
REFERENCES
- Palena LM, Toni F, Piscitelli V, Maffei M, Leonardi M (2009) CT Diagnosis of Cerebral Venous Thrombosis: Importance of the First Examination for Fast Treatment. Neuroradiol J 22: 137-149.
- Saposnik G, Barinagarrementeria F, Brown RD Jr, Bushnell CD, Cucchiara B, et al. (2011) Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 42: 1158-1192.
- ?outinho JM, Ferro JM, Canhão P, Barinagarrementeria F, Cantú C, et al. (2009) Cerebral venous and sinus thrombosis in women. Stroke 40: 2356-2361.
- Amoozegar F, Ronksley PE, Sauve R, Menon BK (2015) Hormonal contraceptives and cerebral venous thrombosis risk: a systematic review and meta-analysis. Front Neurol 6: 7.
- Bousser MG (2000) Cerebral venous thrombosis: diagnosis and management. J Neurol 247: 252-258.
- McBane RD 2nd, Tafur A, Wysokinski WE (2010) Acquired and congenital risk factors associated with cerebral venous sinus thrombosis. Thromb Res 126: 81-87.
- Dentali F, Gianni M, Crowther MA, Ageno W (2006) Natural history of cerebral vein thrombosis: a systematic review. Blood 108: 1129-1134.
- Neymark EZ (1975) Thromboses of intra cranial sinuses and veins? Medicine.
- Semyonov SE, Shatokhina MG, Nekhorosheva AN, Khromov AA, Zhuchkova EA, et al. (2012) Role and CT and MRI features of focal hyperemia in the development and course of stroke. Bulletin of Siberian medicine 5: 23-26.
- Trufanov GE, Fokin VA, Pyanov IV (2005) An x-ray computer and magnetic and resonance imaging in the diagnosis of an ischemic stroke. SPb ELBI-SPb 192.
- Von Kummer R, Allen KL, Holle R, Bozzao L, Bastianello S et al. (1997) Acute stroke: usefulness of early CT findings before thrombolytic therapy. Radiology 205: 327-333.
- Ananyeva NI, Trofimova TN (2006) CT and MRI-diagnosis of acute ischemic strokes. St Petersburg, Russia.
- Lee SK, terBrugge KG (2003) Cerebral venous thrombosis in adults: the role of imaging evaluation and management. Neuroimag Clin N Am 13: 139-152.
- Leach JL, Fortuna RB, Jones BV, Gaskill-Shipley MF (2006) Imaging of cerebral venous thrombosis: current techniques, spectrum of findings, and diagnostic pitfalls. Radiographics 26: 19-43.
- Suslina ZA, Kistenev BA, Smirnova IN (1997) Thrombophlebitis of the internal jugular vein and sigmoid sinus in the acute period of a stem ischemic stroke. Neurologic journal.
- Belova LA, Mashin VV (2016) Venous discirculation in chronic forms of cerebrovascular pathology. Ulyanovsk University, Russia.
Citation: Yuryevich MM, Vladimirovich MV, Anatolyevna BL, Vyacheslavovna BN, Nickolaevich PA, et al. (2016) Clinical-Imaging Features of Venous Strokes. J Non Invasive Vasc Invest 1: 003.
Copyright: © 2016 Belova Liudmila Anatolyevna, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
© 2024, Copyrights Herald Scholarly Open Access. All Rights Reserved!

