
Coronary Artery Fistula to Pulmonary Artery
*Corresponding Author(s):
Calero Rueda MJDepartment Of Cardiologist, Hospital Infanta Elena, Madrid, Spain
Tel:+34 902020068,
Email:mjose.calero@idcsalud.es
INTRODUCTION
Coronary artery fistula is an anomalous communication between the coronary arteries and the cardiac chambers or major vessels. They constitute approximately 14% of all coronary artery abnormalities [1]. The majority of coronary artery fistulas are congenital. They may also be acquired (infectious, due to complications during invasive cardiac procedures or trauma, due to inflammation, or collagen vascular disease [2]. The majority of adult patients are asymptomatic, and among symptomatic patients, chest pain is the most common symptom.
CASE REPORT
We are presenting the case of a 66 year old non-smoking male with past medical history of well controlled hypertension and dyslipidemia. Patient has history of cerebrovascular accident 2 years ago with subtle right residual hemiparesis. He was referred to the cardiologist because he had been experiencing moderate effort-induced angina for the past three months. He complained of no other symptoms. Labs studies were unremarkable. Electrocardiography showed a sinus rhythm. Heart rate 75/min with nonspecific repolarization alterations (Figure 1). Physical examination was normal. No murmurs were identified.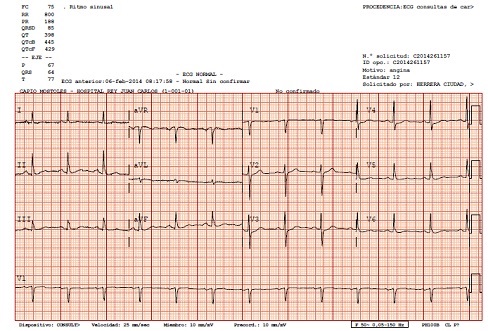
Figure 1: Electrocardiogram showing no specific repolarization changes.
Treadmill test was performed with the Bruce protocol but it was short and inconclusive (5 minutes. 6, 2 METS. Predicted maximum heart rate 72 %), clinically positive with chest pain but with no ischemic ECG changes. Due to persistent symptoms the patient underwent coronariography that revealed ectasia of the proximal portion of the anterior descending artery with nonsignificant surface irregularities. Arising from the middle third of the anterior descending artery there was a fistula connecting with the main pulmonary artery. Dominant right coronary and circumflex arteries showed non-significant irregularities (Figure 2). 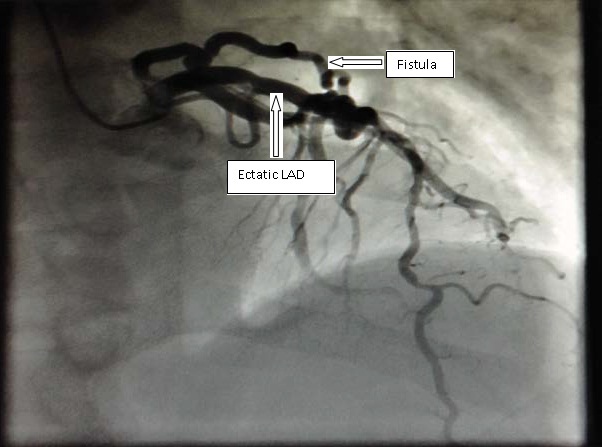
Figure 2: Coronariography showing the fistula arising from the anterior descending artery.
LAD: Left Anterior Descending artery
Coronary CT and coronary angiography findings were concordant confirming the main pulmonary artery as the site of drainage (Figure 3). Perfusion stress test was then performed (with 99mTc labeled sestamibi) and showed no signs of ischemia in spite of patient symptoms (Figure 4). Finally patient underwent a cardiac MRI and the pulmonary to systemic blood flow ratio (Qp/Qs) obtained was 1, which excluded the possibility of significant left to right shunt. The patient is now stable with antianginal treatment with bisoprolol and ranolazine in class II of the Canadian Cardiovascular Society Angina Classification. Interventional measures had been postponed due to clinical stability and the absence of significant ischemia in the isotopic study.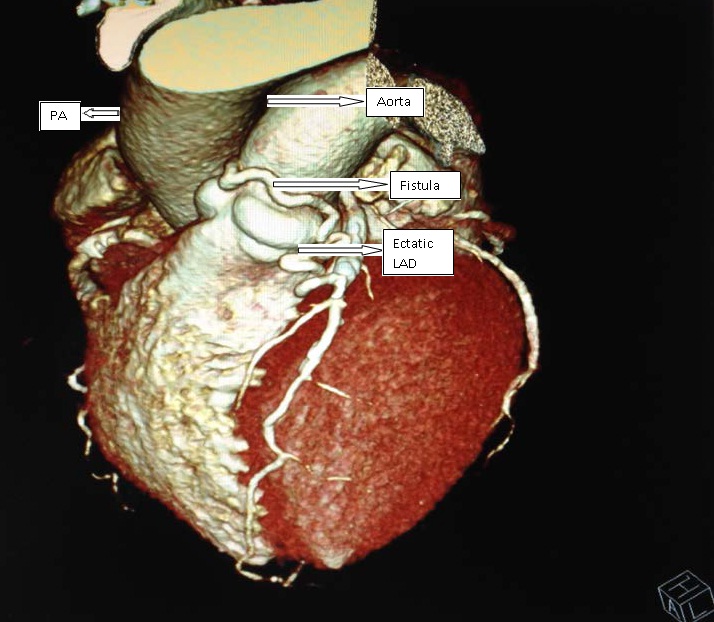
Figure 3: CT volume rendering confirming the main pulmonary artery as the site of drainage.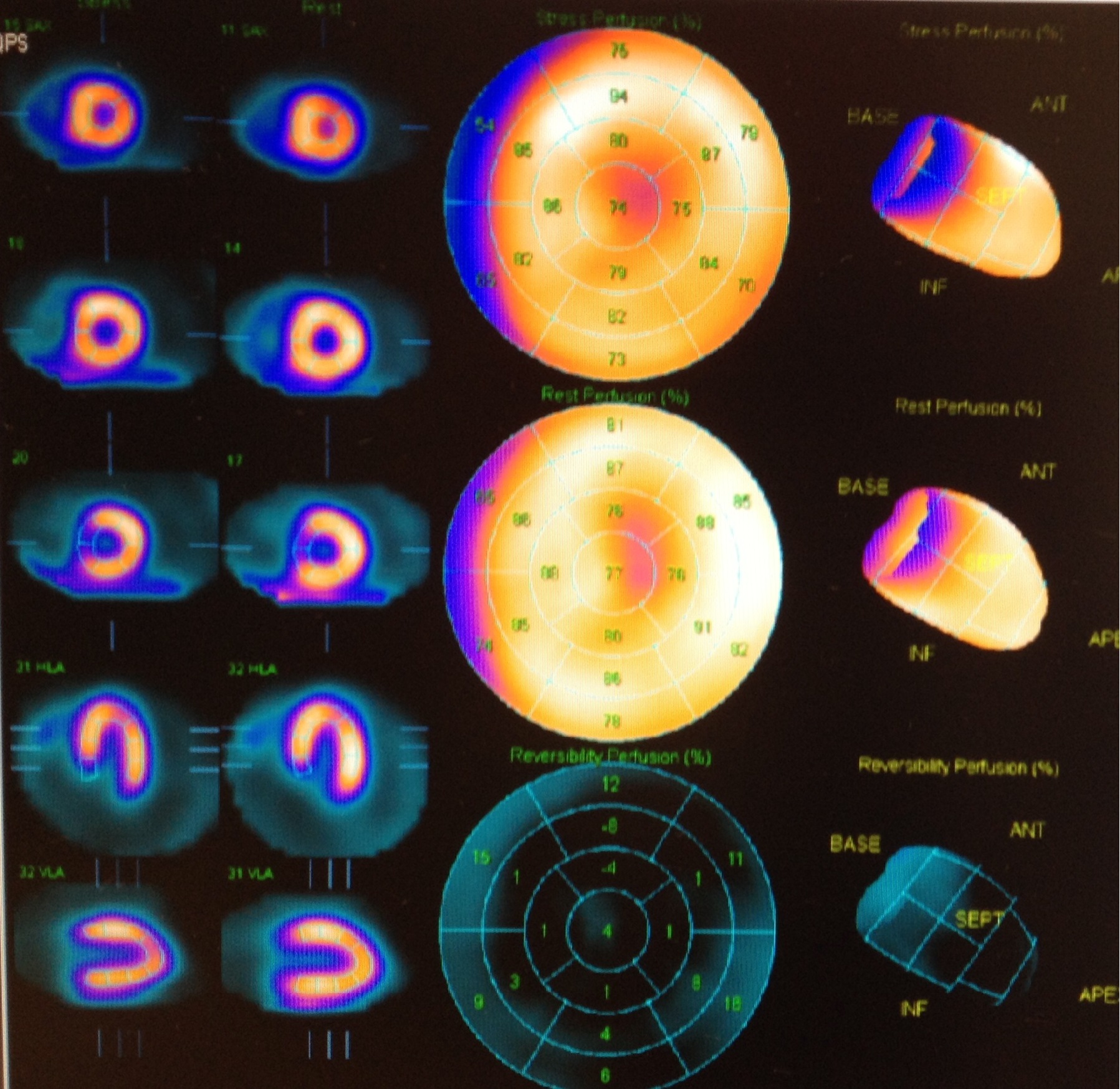
Figure 4: Perfusion stress test with 99mTc labeled sestamibi with no signs of ischemia.
DISCUSSION
Coronary artery fistulas are rare congenital coronary abnormalities. They are observed in 0.002% of the general population. Its prevalence is around 0.08-0.4% among all congenital heart diseases and 0.3-0.8% in catheterization laboratories. This abnormal communication seems to be consecutive to an embryologic persistence of primitive intratrabecular spaces [3]. Major sites of origin of fistula are the right coronary artery (55%), left coronary artery (35%), and both coronary arteries (5%). Major termination sites are the right ventricle (40%), right atrium (26%), pulmonary arteries (17%), and less frequently the superior vena cava or coronary sinus, and least often the left atrium and left ventricle [4].
The majority of adult patients are asymptomatic, because most coronary artery fistulae are small, and the lesion is detected as an incidental finding during coronary angiography for an unrelated diagnosis. However, there may be coronary artery steal, with resultant ischemia of the segment of myocardium perfused by the coronary artery distal to the fistula and compensatory dilatation in the adjacent proximal vessel segment. Steal can be caused by physiologic factors that increase shunting flow into the fistula at the expense of nutrient flow [5].
Among symptomatic patients, dyspnea and chest pain represent a frequent clinical symptom in adults (71%) while in the pediatric age group the majority are silent (79%) [1]. Other symptoms have also been reported including congestive heart failure, pulmonary hypertension, hemoptysis, rupture, or thrombosis of fistula or an associated arterial aneurysm.
The presence of fistula-induced ischemia cannot always be demonstrated: Stress TI-201 Myocardial Perfusion Gated Spect Scintigraphy was performed to investigate the presence of ischemia in 23 patients with no significant stenosis noted in the vessel of origin. While perfusion defect was observed in 7 (30.4%) patients, no evidence of ischemia was found in 16 (69.6%) [6].
Physical examination in patients with coronary fistulas usually found continuous murmur in the left sternal border. Notwithstanding, the location on the chest wall where the murmur is the loudest depends on where the fistula enters the heart. Eventhough clinical history, physical examination, ECG with signs of overload, abnormal shadow on chest X-ray and echocardiogram with abnormal flow by color doppler imaging and dilatation and aneurysm of the donor vessel can lead to the diagnosis, coronary angiography and coronary CT are the imaging modalities of choice for the diagnosis of coronary fistula.
Classically the cornerstone in establishing the diagnosis was conventional coronary angiography [7]. Recent publications after the introduction of multi-detector computed tomography proved that coronary computed tomography angiography is more detailed than conventional selective coronary angiography yielding a better assessment of the connections between the fistula and the adjacent structures [8].
The management of coronary fistulae must be individualized on the basis of the presence or absence of cardiovascular symptoms, the magnitude of the volume load on the heart, and the presence or absence of myocardial ischemia or ventricular dysfunction. General approach guidelines recommend closure of all large coronary artery fistulae regardless of symptomatology. Closure of small to moderate fistulae only in the presence of symptoms (including ischemia, arrhythmia and unexplained systolic or diastolic dysfunction). Closure of small, asymptomatic coronary artery fistulae is not recommended [9].
In those cases were treatment is indicated, percutaneous (transcatheter embolization techniques using coils, bags, or other devices) or surgical closure is a Class I recommendation [9]. The choice of treatment method depends on the anatomy and morphologic features of the fistula.
REFERENCES
- Said SA, el Gamal MI, van der Werf T (1997) Coronary arteriovenous fistulas: collective review and management of six new cases--changing etiology, presentation, and treatment strategy. Clin Cardiol 20: 748-752.
- Gasser S, Gasser R, Bareza N, Klein W (2003) Iatrogenic coronary artery fistula in post transplant patients: Pathogenesis, clinical features and therapy. J Clin Bas Cardiol 6: 19-21.
- Gowda RM, Vasavada BC, Khan IA (2006) Coronary artery fistulas: clinical and therapeutic considerations. Int J Cardiol 107: 7-10.
- Hoffman JI (1995) Congenital anomalies of the coronary vessels and the aortic root. In: Emmanoulides GC, Riemenschneider TA, Allen HD, Gutgesell HP (eds.). Heart disease in infants, children and adolescents. (5thedn), Williams and Wilkins, Baltimore, USA. Pg: 780.
- Angelini P (2002) Coronary artery anomalies--current clinical issues: definitions, classification, incidence, clinical relevance, and treatment guidelines. Tex Heart Inst J 29: 271-278.
- Yigit Canga, Kazim Serhan Ozcan, Ayse Emre, Seref Kul, Tolga Sinan Guvenc, et al. (2012) Coronary artery fistula: review of 54 cases from single center experience. Cardiol J 19: 278-286.
- Said SA (2011) Current characteristics of congenital coronary artery fistulas in adults: A decade of global experience. World J Cardiol 3: 267-277.
- Early SA, Meany TB, Fenlon HM, J Hurley J (2008) Coronary artery fistula; coronary computed topography - The diagnostic modality of choice. Journal of Cardiothoracic Surgery 3:41.
- Warnes CA, Williams RG, Bashore TM (2008) ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Adults with Congenital Heart Disease). J Am Coll Cardiol. 52: 1-121.
Citation: Calero Rueda MJ, Arjonilla López A, Sánchez-Aquino R, Herrera F, Sanz P, et al. (2014) Coronary Artery Fistula to Pulmonary Artery. J Clin Stud Med Case Rep 1: 002.
Copyright: © 2014 Calero Rueda MJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

