
100 Months Experiences with VenaSeal® Vein Glue: Long Time Follow - Up Study Conducted on 2912 Truncal Saphenous Veins in 1509 Cases
*Corresponding Author(s):
Ulf Th ZierauSaphenion Vein Care Centers, Berlin, Germany
Tel:+049 1708302447,
Email:dr.zierau@yahoo.de
Abstract
The paper is about long - time experiences in treatment of truncal varicose veins with the vein glue VenaSeal®: 100 months - follow up of 1509 cases and 2912 truncal varicose veins. Since 1999 years by now, varicosis has been increasingly treated endovenously. At the start, the rather inconvenient VNUS® Closure plus - procedure and the more convenient linear laser procedure were used, and these were followed in 2007 by the bipolar RFITT® catheter, the VNUS® Closure Fast system and the radial laser. These endovenous treatment techniques were followed by the Clarivein System and the VenaSeal® System in 2011/2012. Thus, in the course of the last few years, plenty of experience has been gathered with endoluminal therapy, quality criteria have been defined and standards for the different techniques have been developed.
The presented actual paper sheds light on the advantages and disadvantages of the vein glue VenaSeal® and presents the 100-months results of a single-center praxis study with prospective design.
We will report about our experiences and results of a prospective comparative study of VenaSeal® - Closure in the treatment of 2512 saphenous veins (1949 GSV, 731 SSV, VSAL in 110 cases, VSAM in 87cases, femoropopliteal vein in 33 cases and Giacomini’s vein in 2 cases). Also ulcera crures were included in 17 cases (Figure 1).
INTRODUCTION

Figure 1: Dr. Ulf Zierau in Saphenion® Vein Care Center Berlin.
It the base of varicose vein therapy, that all varicose veins should be treated actively. This we can find in nearly all guidelines worldwide. An insufficient varicose vein is working like a downpipe - the blood pressure at the lower leg is increased chronically. All the specialists know, that mobilization and compression all one cannot normalize the venous function of outflow venous blood from the leg. If we are passive in our treatment options, we get the typical chronique venose disease. Nearly 70% of all adults in europe have clinical signs of this CVD.
Since 22 years by now, varicosis has been increasingly treated endovenously. Before this, the varicose veins were treated geradically with the “stripping” - method, a 114 years old radical surgery method.
At the start, the rather inconvenient VNUS® Closure Plus procedure and the more convenient linear laser procedure were used, and these were followed in 2006/2007 by the bipolar RFITT® catheter, the VNUS® ClosureFast system and the radial laser. These endovenous treatment techniques were followed by the Clarivein System and the VenaSeal® System in 2011/2012.
Thus, in the course of the last nine years, plenty of experience has been gathered with endoluminal therapy, quality criteria have been defined and standards for the different techniques have been developed [1-21].
One very important technical development combined with the beginning of the endovenous therapy was the colour ultrasound (duplex) - we can see the catheter inside the veins, the glue and we can control the tip of catheter, the work inside the vessel and the effects inside the body - without any radiation and without i.v. contrast agents. These is an very important fact, because working with an endovenous catheter without ultrasound isn`t a fully noninvasive therapy because of using phlebography. Ratzek, et al. have described exactly the sonographic appearances of common disorders of all tissues. They have worked about the high sensitivity of ultrasound in tissue diagnostics [22-24].
In addition, 18 years ago in 2003, far from the beaten tracks of radio wave and laser, the development of a fascinatingly simple, yet nevertheless highly effective method of sealing veins - the VenaSeal® - Closure technique - was initiated. After CE - approval had been granted in the autumn of 2011, a number of vein centers in Germany and Europe started using the VenaSeal® - system. By now, 25 centers are working successfully with the new therapy system in Germany alone. Today there is an approval in all countries, also in USA since 2 / 2015.
The author has applied Venaseal® for the first time in a great saphenous vein on 1st. August 2012 (Figure 2). 
Figure 2: VenaSeal® - Closure technique.
MATERIAL AND METHOD
In consideration of the manufacturer’s application instructions, and with own modifications of the sealing technique sealing with the VenaSeal - system was started 1-1,5 cm from the saphenofemoral junction, and a spot of glue was applied at intervals of 2 - 3 cm, depending on the diameter and the flow and pressure of the vein. We measure this pressure with an endovenous catheter before application of glue inside the vein. Thick branch - offs of auxiliary side branches were additionally treated with a single - shot glue. The maximal diameter of treated truncal veins was 2,3 cm, also venous aneurysmas, ectatic veins and perforators were treated (Figure 3).
The follow - up observation period in our study was up to 100 months.
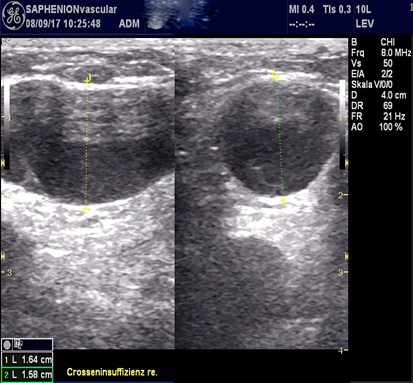 Figure 3: Venous aneurysm nearly the ilio-femoral junction of GSV, ultrasound in transverse and longitudinal examination after VenaSeal®-therapy, (marker is showing the diameter of vein).
Figure 3: Venous aneurysm nearly the ilio-femoral junction of GSV, ultrasound in transverse and longitudinal examination after VenaSeal®-therapy, (marker is showing the diameter of vein).
The great saphenous vein was treated in 1949 cases (Figure 4), in 731 cases the small saphenous vein was treated and in 197 cases the trunc of an inguinal accessoric vein was sealed. Two Giacomini veins and 33 femoro-popliteal veins also were treated.

Figure 4: Typical ultrasound of GSV after sealing.
VenaSeal® interventions were performed under light sedation with Dormicum or local anesthesia for venous access accompanied by music therapy, In 203 cases (13,5%) the patients dispensed and did’nt got any anaesthesia. One patient performed pain acupuncture on herself on point G4.
All patients are given a follow - up examination by duplex sonography in the scope of a prospective study (our own quality management) on the 1st / 14 - 30th. / 70 - 90th day as well as after 6 and 12 months. After this we controlled every following year. The most of all duplex sonography examinations post intervention were done by another collegue, not by the vascular surgeon treated the truncal varicose veins.
RESULTS
During the time period from 1st.September 2012 to 31st. December 2020 (100 months), Venaseal® was used for treatment of truncal varicose veins to achieve closure in 2912 truncal veins (Table 1). In 428 patients one saphenous vein were treated; in 820 patients two saphenous veins were treated; in 207 patients 3 saphenous veins were treated. In 48 cases 4 truncal veins, and in five cases 5 veins, in one case 6 truncal veins were treated simultaneously. So nearly 72% of all patients have got a treatment of truncal varicose veins simultaneously in one session.
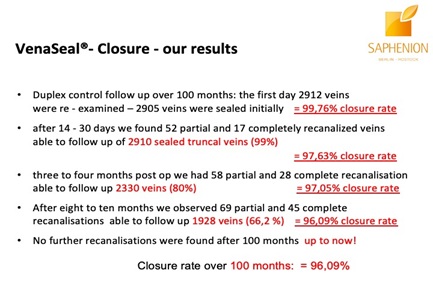
Table1: Follow up - results after Venaseal®.
Grade 2 - 4 varicosis of the GSV according to Hach, and in the case of the SSV grade 2 - 3 saphenous varicosis acc. to Hach, was the inclusion criterium. In accessoric veins we treatet the inguinal trunc in length between 12-25 cm (Figure 5).
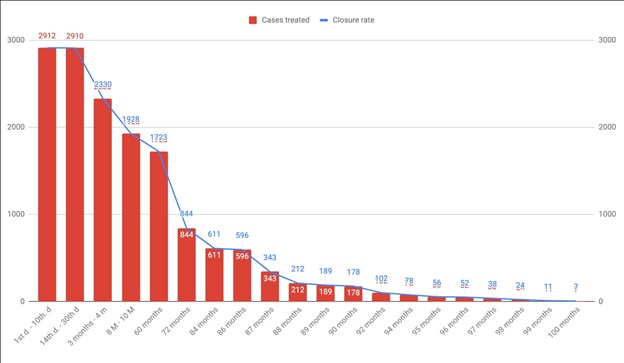
Figure 5: 100 months VenaSeal® in 2912 veins and 1509 cases - the closure rate in time line.
On the 1st day 2912 veins were checked (2905 veins were closed initially = 99,76 %) in the scope of follow - up, and up to the 30th. day, partial recanalization was found in 52 veins, and complete recanalization was found in 17 veins. This corresponds to a closure rate of 97,63%.
Over a time period of 3 months up to 4 month after the treatment, we were able to follow up 2330 saphenous veins (80% of all veins that had been treated), and here we found 58 partial and 28 complete recanalizations. The closure rate is thus 97,05%.
Followed up over a 6 - 8 month time period were 1928 saphenous veins (66,2%), and 69 partial and 45 complete recanalizations were found, resulting in an effectiveness of 96,09%.
No further recanalizations were found after 100 months. In the follow - up period of 5 years after therapy we controlled 1723 truncal varicose veins (59,2%) up to now.
All 17 leg ulcers were healed until to 20 weeks after intervention. 2912 truncal varicose veins having been sealed with Venaseal®, the results achieved over the entire time period of 100 months are equivalent to a closure rate of 96.09%.
The pain score (range 1-10) for subjectively felt pain on the 1st. day post - sealing was between 1,6 and 3,4 (2.1) - in RFITT between 3,8 and 4,1.
In 218 treated veins (7,5%), we observed a postoperative unspecific inflammatory skin reaction after approx. 10 - 14 days in the Venaseal group; with appropriate antiphlogistic treatment with ibuprofen and cooling dressings, this subsided within 3 - 5 days.
In all other cases subjected to follow - up examinations, no complications of any kind, no paresthesias or hypesthesias, no permanent skin reactions, no phlebitis or thrombosis or infections were observed (Table 2).
Only in 26 cases (0,9%) we have seen a lymphatic fistula at the peripherial punktion. In particular, even subcutaneously situated saphenous veins could be glued without any significant skin reaction (reddening, swelling).
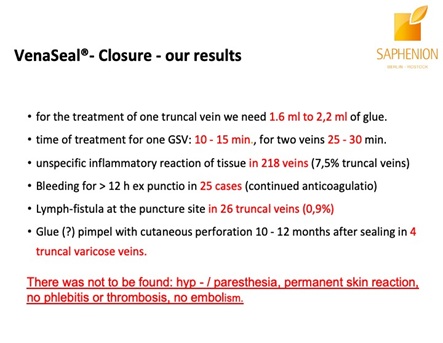 Table 2: Side effects after Venaseal®-therapy.
Table 2: Side effects after Venaseal®-therapy.
We also clearly prefer VenaSeal® in treatment of SSV (Figure 6), and now also in GSV due to the large number of neurological sensations in connection with treatment by Laser and Radiofrequency [23,24].
 Figure 6: VenaSeal® is first choice in sealing SSV.
Figure 6: VenaSeal® is first choice in sealing SSV.
Nearly all patients were greatly surprised at the fully ambulatory intraoperative procedure and the brief and pleasant postoperative convalescence phase.
All patients were able to leave the office between 30 and 120 minutes after the intervention.
In the case of VenaSeal, we have up to now refrained from applying compression therapy in over 90% of all cases. We prefer to use compression stockings only in cases, the diameter of the treated vein ist over 1,5 cm or in treatment of venous aneurysm or ectatic varicous veins.
DISCUSSION
In the last 21 years, the necessary quality criterias for endovascular interventions on veins with varicose changes were largely laid down, and several comparative studies on functional efficiency of radical stripping surgery on the one hand and endovenous treatments on the other hand were furthermore conducted. They also have clinical advantages and quite significantly reduce side effects and complications such as still occur regularly today as in the past in connection with the conventional surgical technique.
By now, it has emerged as an undeniable fact that endovenous interventions do not only exhibit a merely cosmetic advantage as was hitherto assumed.
Thus, the colleagues who work with endovenous procedures meanwhile have reliable criteria for a high - quality therapy [1-4, 6-9, 10-12, 13, 15, 16-19,25,26,].
The VenaSeal® - closure procedure is one of the new technical developments in the series of endovenous therapeutic procedures. Although it is a catheter - based procedure in terms of the basic principle of the therapeutic approach, it differs fundamentally with regard to the closure technique. The procedure is not a thermal one, while the glue likewise gives rise to a certain temperature (approx. 40 - 45°C). Side effects as those known to occur in connection with laser and radio wave therapy ultimately play no significant role here. The necessary reliable closure is achieved by means of a non tumescent, non thermal cyanoacrylate glue. The basic chemical formula of which has been known since 1949. First being used in operative medicine in the early 60s as tissue adhesive or replacement of wound sutures.
Today is being used in nearly all operative disciplines, i.e., dermatology, ophthalmology, orthopedics, surgery, orthodontics. Interventional radiologists use this cyanoacrylate glue in the treatment of vascular malformations since 1981.
We also worked with this glue since 1988 in vascular surgery at the Charitè - hospital Berlin.
We do not need anesthesias anymore and can in most cases do without postoperative compression therapy. Elastic stockings should nevertheless by all means be recommended after the treatment of thicker saphenous varicose veins measuring > 1,2 cm. They become compulsory where we intend to apply gluing therapy in larger lumens measuring 1.5 cm and more, ectatic veins, junction aneurysmas and also perforator veins [4,15,-19].
The significantly reduced side effects and a well - nigh negligible pain score are also clear advantages in comparison with laser and radio wave therapy. No paresthesias, no hypesthesias, no phlebitis, extremely rare occurrence of skin pigmentations are only a few of the important advantages of the VenaSeal® - procedure.
In the final analysis, the new procedure has to meet solely the hard criterion of efficacy, namely the permanence of an effective vein closure. And as far as this aspect is concerned, both the first results of the eSCOPE study [13] and the results of single - center studies, and also currently of the VeClose study [11] and last but not least, the German Multicenter study 2020 are very good [7]. The closure rate is similarly high as that achieved with radio waves, namely between 93 - 100% when all results are summarized.
Thus, the VenaSeal® - procedure appears to be on the same level with, or even superior to the high - frequency radio wave system [10,27). In the time periods between 12 and 36 months covered by follow - up examinations up to now, both procedures have proven quite clearly superior (99,6%) to laser therapy in terms of effectiveness [4,12,18,27,33].
The results of first comparative studies show that the VenaSeal® -glue is clearly superior with regard to postoperative side effects though. Both the pain score and the rate of side effects are very low in comparison [4, 15,18]. Particularly pain as well as the neurological side effects no longer play any significant role at all. These are the main problem associated with laser and radio wave therapy though.
By now, VenaSeal® has undeniably become at SAPHENION the therapy of first choice for the treatment of the SSV. Here, we meanwhile consider the well - known risk of neurological side effects and complications associated with application of the laser and radio frequency techniques as being too high [4-8,27,14-19,21,28].
In the light of the 19 years of experience we have gathered by now, we recommend that every vein center that applies endovenous treatment should have at least 2 alternative treatment procedures at its disposal. For us, this means that in practical work with VenaSeal®, all insufficient saphenous veins should as far as possible always be treated in one session [4, 16-21].
Independently of this and including all experiences with modifications of the sealing technique we at SAPHENION® meanwhile regard Venaseal® - closure as treatment of first choice in the range of catheter - supported therapeutic procedures for GSV and SSV or VSAA - varicosis. Also in obese patients and older patients we see great advantages in using VenaSeal® - Closure (Figure 7).
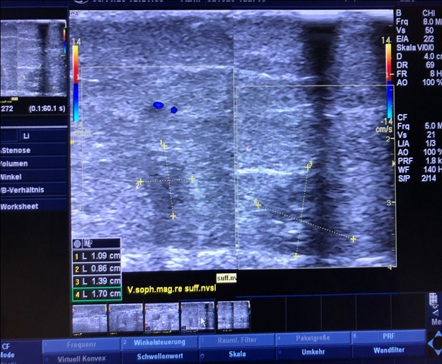 Figure 7: VenaSeal® is first choice in therapy of obese patients.
Figure 7: VenaSeal® is first choice in therapy of obese patients.
REFERENCES
- Abdel Razek AA, Al Belasy F, Ahmed W, Haggag M (2015) Assessment of articular disc displacement of temporomandibular joint with ultrasound. J Ultrasound 18: 159-163.
- 2. Almeida JI, Min RJ, Raabe R, McLean DJ, Madsen M (2011) Cyanoacrylate adhesive for the closure of truncal veins: 60-day swine model results. Vasc Endovasc Surg 45: 631-635.
- Almeida JI, Mackay EG, Bautista C, Proebstle T (2012) Cyanoacrylate glue great saphenous vein ablation: preliminary 180 - day follow up of a first - in - man feasibility study of a no-compression - no - local anaesthesia technique. J Vasc Surg 55: 297.
- Almeida JI, Murray SP, Romero ME (2019) Saphenous vein histopathology 5.5 years after cyanoacrylate closure. J Vasc Surg Venous Lymphat Disord 8: 280-284.
- Creton D, Rea B, Pittaluga P, Chastanet S, Allaert FA (2012) Evaluation of the pain in varicose vein surgery under tumescent local anaesthesia using sodium bicarbonate as excipient without any intravenous sedation. Phlebology 27: 368-373.
- Elias S, Raines JK (2012) Mechanochemical tumescentless endovenous ablation: final results of the initial clinical trial. Phlebology 27: 67-72.
- Fuchs J, Zierau UT, Fuchs J, Bernheim C (2020) Long-term results of cyanoacrylate closure for the treatment of incompetent saphenous veins: A German multi-center experiencez. J Phlebol Lymphol 13: 1-4.
- Huisman LC, Bruins RMG, van den Berg M, Hissink RJ (2009) Endovenous laser ablation of the small saphenous vein: prospective analysis of 150 patients, a cohort study. Eur J Vasc Endovasc Surg 38: 199-202.
- Gibson K, Morrison N, Kolluri R, Vasquez M, Weiss R, et al. (2018) Twenty-four month results from a randomized trial of cyanoacrylate closure versus radiofrequency ablation for the treatment of incompetent great saphenous veins. J Vasc Surg Venous Lymphat Disord 6: 606-613.
- Ivanova, Patricija: Post procedere neuropathy: comparison of surgery, EVLA and glue; Presentation on 2nd. NEEF, Riga.
- Keel D, Goldman MP (1999) Tumescent anaesthesia in ambulatory phlebectomy: Addition of epinephrine. Dermatol Surg 25: 371-372
- Kolluri R, Chung J, Kim S, Nath N, Bhalla BB, et al. (2020) Network meta-analysis to compare VenaSeal with other superficial venous therapies for chronic venous insufficiency. J Vasc Surg Venous Lymphat Disord 8: 472?481.
- Lawson J, S Gauw, C van Vlijmen, P Pronk, M Gaastra, et al. (2013) Sapheon: the solution? Phlebology 1: 1-8.
- Min RJ, Almeida JI, McLean DJ, Madsen M, Raabe R (2012) Novel vein closure procedere using a proprietary cyanoacrylate adhesive: 30-day swine model results. Phlebology 27: 398-403.
- Nick M, Gibson K (2014) Veclose Study: Preliminary Month 1 Data; 2nd Annual Cyanoacrylate Embolization Symposium, Mainz.
- Navarro-Triviño FJ, Cuenca-Manteca J, Ruiz-Villaverde R (2019) Allergic contact dermatitis with systemic symptoms caused by VenaSeal. Contact Dermatitis ;82: 185-187.
- Proebstle TM, Almeida JI, Javier JJ, Mackay Ed, Bautista C (2012) One - Year follow up of first human use of cyanoacrylate adhesive for treatment of saphenous vein incompetence.
- Proebstle TM, Vago B, Alm J, Go?ckeritz O, Lebard C, et al. (2008) Treatment of the incompetent great saphenous vein by endovenous radiofrequency powered segmental thermal ablation: first clinical experience. J Vasc Surg 47: 151-156.
- Proebstle TM, Alm J, Rasmussen L, Dimitri S, Lawson JA, et al. (2015) The European Multicenter Study On Cyanoacrylate Embolization Of Refluxing Great Saphenous Veins. J Vasc Surg Venous Lymphat Disord 3: 2-7.
- Proebstle TM, Alm J, Rasmussen L, Dimitri S, Whiteley M, et al. (2012) Cyanoacrylate Adhesive For Treatment of Great Saphenous Vein Incompetence without Tumescent Anesthesia and without Compression Therapy. Florida, USA.
- Rasmussen LH, Bjoern L, Lawaetz M, Lawaetz B, Blemings A, et al. (2010) Randomised clinical trial comparing endovenous laser ablation with stripping of the great Saphenous vein: clinical outcome and recurrence after 2 years. Eur J Vasc Endovasc Surg 39: 630-635.
- Razek AA, Fouda NS, Elmetwaley N, Elbogdady E (2009) Sonography of the knee joint. J Ultrasound 12: 53-60.
- Razek AA, El-Basyouni SR (2016) Ultrasound of knee osteoarthritis: interobserver agreement and correlation with Western Ontario and McMaster Universities Osteoarthritis. Clin Rheumatol 35: 997-1001.
- Rosen RJ, Contractor S (2004) The use of cyanoacrylate adhesives in the management of congenital vascular malformations. Sem Interv Radiol 21: 59-66.
- Shadid N, Ceulen R, Nelemans P, C Dirksen, J Veraart, et al. (2012) Randomized clinical trial of ultrasound-guided foam sclerotherapy versus surgery for the incompetent great saphenous vein. Br J Surg 99: 1062-1070.
- Shepherd AC, Gohel MS, Lim CS, Hamish M, Davies AH (2010) The treatment of varicose veins: an investigation of patient preferences and expectations. Phlebology 25: 54-65.
- Thum J (2019) Single Center Erfahrungen aus 234 Stammvenenbehandlungen mit viskösem n - Butyl - 2 - Cyanoacrylat- Verwendbarkeit, Akzeptanz, Ergebnisse; vasomed 1: 28-31.
- Ints Ü (2019) 6 years single center results, Baltic Vein Clinic“ of truncal varicose vein sealing; Presentation on 2nd. NEEF, Riga.
- Zierau UTh (2014) VenaSeal® - Therapie bei SAPHENION - 18 Monats - Ergebnisse an 379 Stammvenen. Vortrag auf dem 2. Symposium zur VenaSeal® - Closure-Therapie, Mainz.
- Zierau UT (2016) Venenverklebung versus Radiofrequenztherapie bei Varicosis - Verlaufsstudie über 36 Monate mit 1139 Behandlungen. 28: 212 - 216.
- Zierau UT (2018) Practice for vascular diseases and venous center. Vein Center Berlin, Berlin, Germany.
- Zierau UT, Martell L, Lahl W (2020) 8 years vein glue therapy with VenaSeal® - 8 special cases; J Clin Rev Case Rep 5: 481.
- Zierau UT (2020) 8 Jahre VenaSeal® - Therapie an Stammkrampfadern, eine Single Center - Studie; 62. Jahrestagung der DGP 2.- 5. 9. 2020, Leipzig.
Citation: Zierau UT (2020) 100 Months Experiences with VenaSeal® Vein Glue: Long Time Follow - Up Study Conducted on 2912 Truncal Saphenous Veins in 1509 Cases. J Angiol Vasc Surg 5: 054.
Copyright: © 2020 Ulf Th Zierau, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

