
A Black Ear in A HIV Patient
*Corresponding Author(s):
Andrea CuevaDermatology Resident, Dermatology Universidad Tecnica Equinoccial, Ecuador
Abstract
Cutaneous adverse drug reactions (CADR) can present multiple morphologies and differential diagnoses. As HIV, patients are on multiple drugs CADR should always be suspected when new skin rashes appear. Here we discuss the diagnostic process of a CADR secondary to antiretroviral therapy in a male patient with HIV.
Keywords
Adverse Drug Reaction; Antiretroviral therapy; Emtricitabine
Introduction
Drug reactions can appear with multiple morphologies; Cutaneous adverse drug reactions (CADR) are more common in HIV patients than in the general population. [1] This may be related to the drugs these patients receive; not only antiretrovirals, but also medication for other comorbidities such as antivirals, antibiotics, chemotherapy, antineoplastics, anticonvulsants among others. Furthermore, as their immunity lessens, these patients could have a larger susceptibility to develop any type of drug reactions [2].
Case Report
We present a 61-year-old male patient, with a 4-year history of HIV, receiving treatment with Tenofovir and Emtricitabine. He consults for purplish spots on his ears, nose, arms, legs and dorsum of the hands, which appeared about 2 months ago without any other accompanying symptoms. Upon examination symmetric, bilateral violaceous and gray macules of about 1 to 6cm in diameter were observed in the anterior pillar of the ear helix, preauricular region, nasal dorsum, arms, and legs. In the hands, the patient presented violaceous and gray scaly papules and plaques (Figures 1 & 2). No mucosal changes were seen and the patient did not refer any accompanying symptoms.
A biopsy of the helix was performed that returned inconclusive, so a second sample was taken from the anterior surface of the right forearm, which reported epidermis covered by basket-weave orthokeratosis with isolated patches of parakeratosis, irregular elongation of the rete ridges, multiple foci of spongiosis and extensive vacuolar damage to the interface with pigmentary incontinence (Figures 3 & 4). Also, on the dermis, moderate superficial and interstitial perivascular inflammatory infiltrate composed of lymphocytes, histiocytes and occasional eosinophils and dilated capillaries (Figure 5). These histological findings are compatible with a cutaneous reaction to drugs, probably due to emtricitabine, so a change to medication was suggested.
 Figures 1 & 2: Clinical images, hyperpigmented, violaceous papules and plaque.
Figures 1 & 2: Clinical images, hyperpigmented, violaceous papules and plaque.
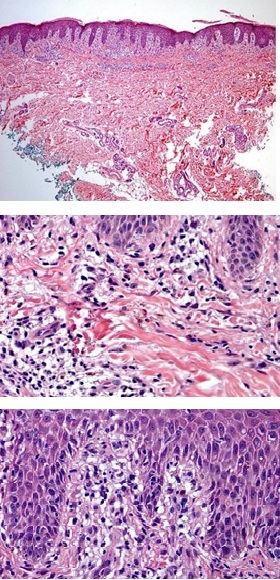 Figures 3,4 and 5: Histology images.
Figures 3,4 and 5: Histology images.
Discussion
The World Health Organization defines an Adverse Drug Reaction (ADR) as “any response to a drug which is noxious and unintended, and which occurs at doses used in man for prophylaxis, diagnosis or treatment” [3].
ADRs are classified into 4 categories, A, B, C and D; Type A are expected effects, dose dependent, while B are unexpected effects, more dangerous and do not depend on the dose. Type C is secondary to the duration of exposure to a certain medication, and category D includes teratogenic drugs. In this case, the drug reaction is considered type C due to the history and evolution of the clinical symptoms.
Initially the differential diagnoses were contact dermatitis versus psoriasis; however, due to the patient's history, a CADR secondary to antiretrovirals was suspected, which was confirmed with the histopathological report. Emtricitabine is known to cause hyperpigmentation as an adverse effect, either as maculopapular rashes or as a palmoplantar dyspigmentation. Furthermore, a similar case of hyperkeratotic papules and hyperpigmentation on the hands has been reported in the literature as a CADR secondary to emtricitabine. A change in pharmacological regimen was suggested and topical betamethasone and prednisone were sent in decreasing doses.
References
- Felix KH, Sangueza O, Feldman SR, Mariencheck M (2020) A hyperkeratotic drug reaction in a patient on antiretroviral therapy. JAAD Case Reports. 6: 1239-1241.
- Blanes M, Belinchón I, Portilla J (2009) Reacciones cutáneas adversas a fármacos en los pacientes con infección por el VIH en la era TARGA. Actas Dermo-Sifiliográficas. 100: 253-265.
- Velasco MA, Velasco SM (2018) Reacciones Adversas Medicamentosas (RAM). Interacciones Medicamentosas. An Real Acad Med Cir Vall. 55: 243-267.
Citation: Felix C, Basantes A, Caceres P, Hidalgo A, Cueva A, et al. (2024) A Black Ear in A HIV Patient. J Clin Stud Med Case Rep 11:233
Copyright: © 2024 Camila Félix, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

