
A Case Series of Children with ADHD and Restless Sleep
*Corresponding Author(s):
Janet LamDepartment Of Neurology And Developmental Medicine, Kennedy Krieger Institute, Johns Hopkins University, Baltimore, United States
Tel:+1 4439239580,
Fax:4439239540
Email:lam@kennedykrieger.org
Abstract
Children with ADHD may be misdiagnosed if their symptoms are actually secondary to a sleep disorder. Restless Legs Syndrome (RLS) and Periodic Limb Movements of Sleep (PLMS) may disrupt sleep, leading to fragmented sleep and daytime fatigue. This in turn may appear as inattentive symptoms in children and adolescents. Further, children with RLS and PLMS may fidget during the day if they experience discomfort in their legs when sitting still. The first line of treatment for RLS and PLMS is iron supplementation due to the key role iron plays in the dopamine synthesis pathway. In this pilot study, children with ADHD and a history of restlessness were recruited to have a polysomnogram and to check serum iron levels. Even in the small sample size for this pilot study, ferritin levels were negatively correlated with PLMS. This study highlights the relationship between ADHD, iron levels, and Periodic Limb Movements of Sleep (PLMS).
Keywords
ADHD; Children; Iron; Restless sleep
Introduction
Attention-Deficit/Hyperactivity Disorder (ADHD) affects 5% to 15% of school-aged children, in both developed and developing countries [1]. It then persists into adulthood in 30% to 50% of patients [2]. Some behavioral manifestations of ADHD include poor attention, distractibility, hyperactivity, impulsiveness, altered executive functions, or behavior problems at either home or at school [2,3]. ADHD has a particularly high comorbidity of Restless Leg Syndrome (RLS) [4], which also has symptoms difficulty staying still and disrupted sleep [4]. Furthermore, elevated Periodic Limb Movements during Sleep (PLMS) are commonly present in children with ADHD [5]. PLMS can cause significant sleep disruption, leading to reduced quality of life; they are characterized by brief, periodic jerks of the arms or legs that last between 0.5 seconds and 10.0 seconds with 5-90 seconds between movements [6]. These periodic jerks can be accompanied by transient arousals from sleep identified and measured by polysomnography [5]. They are found on sleep studies in 80% of patients with RLS [6]. Both RLS and PLMS are commonly found in children with ADHD [5]. Beyond this, Restless Sleep Disorder (RSD), a more recently defined diagnosis, has a high prevalence in children with RLS and ADHD. RSD is characterized by sleep disruption and frequent nocturnal body movements of large muscle groups, symptoms similar to RLS [7].
Since ADHD shows a high prevalence of comorbidity with other disorders involving restlessness, it is important to target common factors of all these diagnoses. One common observance across them are low serum ferritin levels [2,4], which supports checking iron studies in patients with ADHD and restlessness. Iron deficiency is one of the most prevalent nutritional problems today among children, and there is strong evidence suggesting its critical role for neurological function and development [1]. Furthermore, iron deficiency is linked to increased risk of ADHD [1]. While the pathophysiology of ADHD is not yet fully understood, evidence strongly suggests an imbalance in the dopaminergic and noradrenergic systems [8]. Iron modulates dopamine and noradrenaline production by acting as a cofactor for tyrosine hydroxylase which catalyzes the rate-limiting step of monoamine synthesis [4,8]. Iron deficiency in animal models decreases dopamine receptor density and activity as well as monoamine transporter function, resulting in alternations of monoamine uptake and catabolism [8]. Thus, brain iron stores are expected have influence on the monoamine-dependent functions that are altered with ADHD [8]. In children with ADHD, those with the most severe iron deficiencies expressed the most extreme symptoms [2]. Maintaining serum ferritin above 50 ng/mL has been shown to be beneficial for not only ADHD, but also for RLS and PLMS. Konofal et al., have shown a clear benefit of iron supplementation therapy in ADHD children with a significant improvement on hyperactive/impulsive and inattentive subscales of the ADHD Rating Scale. Additionally, RLS symptoms were improved [8].
Materials and Methods
After receiving approval from the Institutional Review Board at Johns Hopkins University, subjects were recruited from the Sleep Clinic at Kennedy Krieger Institute. Inclusion criteria were a prior diagnosis of ADHD and symptom report of restlessness at night. Exclusion criteria were inability to obtain a sleep study and age greater than 18 years. Patients completed an overnight sleep study at the Sleep Center at Kennedy Krieger Institute (Baltimore, MD). Iron labs (iron level, TIBC, ferritin, transferrin, % sat) were ordered on all subjects.
Results And Discussion
Given that this was a pilot study, ten patients were recruited which met the goals of this trial. The majority of these subjects (90%) were males. The mean age was 11 +/- 3.8 hrs. Total iron levels ranged from 49-209 with an average level of 85 +/- 51.2.
Ferritin levels ranged from 37-102 with an average level of 74 +/- 23.7. Seven patients completed iron labs and 3 patients failed to obtain iron labs despite reminders (Table 1). These patients were advised to take a multivitamin with iron.
|
Subject |
Age (mean +/- std dev) 11 +/-3.8 |
Sex |
Total iron (mean +/- std dev) 85 +/- 51.2 |
TIBC (mean +/- std dev) 340 +/- 53.4 |
%sat (mean +/- std dev) 24 +/- 12.8 |
Ferritin (mean +/- std dev) 64 +/- 23.7 |
Transferrin (mean +/- std dev) 276 +/- 43.8 |
|
1 |
11 |
M |
73 |
304 |
24 |
37 |
|
|
2 |
12 |
M |
209 |
391 |
53 |
66 |
251 |
|
3 |
11 |
M |
49 |
436 |
11 |
47 |
349 |
|
4 |
7 |
M |
|
|
|
|
|
|
5 |
19 |
M |
60 |
310 |
15 |
102 |
310 |
|
6 |
16 |
M |
63 |
354 |
18 |
97 |
283 |
|
7 |
12 |
M |
69 |
314 |
22 |
53 |
251 |
|
8 |
10 |
M |
73 |
269 |
27 |
48 |
215 |
|
9 |
5 |
F |
|
|
|
|
|
|
10 |
11 |
M |
|
|
|
|
|
Table 1: Iron Lab Results.
All patients completed a polysomnogram, or sleep study, (Table 2). The sleep efficiency average was 86 +/-7.2%. The PLM index ranged from 0-15 with only one subject in the abnormal range at 15.That subject also had more arousals (1.9/hr) associated with leg movements. While all patients or their parents had reported restlessness at night, this study did not find that the majority of them had significant leg movements on polysomnogram. This supports other studies which indicate that parents may misreport symptoms [9]. A history of paresthesias or leg pain is difficult to elicit from pediatric patients. Therefore, it is possible that many of these children are undetected and may be misdiagnosed with hyperactivity in ADHD.
|
Subject |
SE 86 +/- 7.2 |
WASO (min) 61.5 +/- 41 |
PLMS 16.9 +/- 32.2 |
PLMSi 1.9 +/- 4.4 |
PLMS arousal 0.24 +/- 0.6 |
AHI 3.8 +/- 4.0
|
|
1 |
89.8% |
52.5 |
111 |
15 |
1.9 |
1.2 |
|
2 |
93.8% |
32.5 |
0 |
0 |
0 |
13.3 |
|
3 |
73.8% |
116.4 |
0 |
0 |
0 |
0.8 |
|
4 |
90% |
8.5 |
9 |
0 |
0 |
0.7 |
|
5 |
78.1% |
121.7 |
0 |
0 |
0 |
2.3 |
|
6 |
76.2% |
123 |
0 |
0 |
0 |
0.4 |
|
7 |
94.3% |
26.2 |
24 |
2 |
0.3 |
5.2 |
|
8 |
89.9% |
30.5 |
6 |
1 |
0.1 |
0.8 |
|
9 |
91.1% |
40 |
11 |
0 |
0 |
5.4 |
|
10 |
83% |
64 |
8 |
1 |
0.1 |
7.6 |
Table 2: Polysomnogram Results.
SE= Sleep Efficiency; WASO= Wake after Sleep Onset; PLMS= Periodic Limb Movements in Sleep; PLMSi= Periodic Limb Movement in Sleep Index; AHI= Apnea Hypopnea Index.
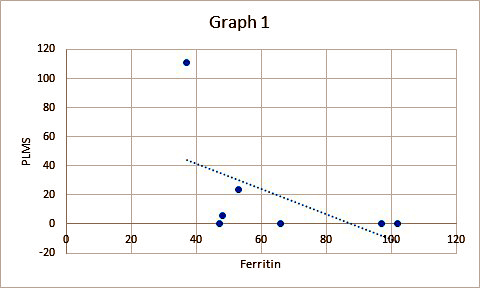
There was a negative association between ferritin levels and PLMS. In other words, higher ferritin levels are associated with less PLMs (Graph 1). This supports other studies which recommend iron treatment for PLMD. One of the benefits of this study is the objective measure of leg movements by polysomnogram. The practice parameter for the American Academy of Sleep Medicine recommends that polysomnography is the only way to establish the diagnosis of PLMD. Further, it is not routinely indicated for RLS unless there is uncertainty of the diagnosis [10].
 A recent development in our understanding of restlessness during sleep is the new diagnosis of “restless sleep disorder”. The major criteria for the diagnosis include complaint of restless sleep, observed large body movements during sleep, video-polysomnographic documentation of 5 or more large body movements/hour during sleep, occurrence at least three times per week for at least 3 months and clinically significant impairment [11]. It is possible that this diagnosis was missed during this study since large body movements were not measured and restlessness was measured by only leg movements from the typical limb leads during polysomnography. However, our results may be similar to those found by Kapoor et al., when evaluating the large body movements with video polysomography in a group of children with ADHD. The authors found only a small percentage, 9.1%, of these children met criteria for restless sleep disorder. They concluded that other comorbid factors (OSA, RLS, medication) may result in the restlessness reported by the majority of parents, 81.1% of children with ADHD [12].
A recent development in our understanding of restlessness during sleep is the new diagnosis of “restless sleep disorder”. The major criteria for the diagnosis include complaint of restless sleep, observed large body movements during sleep, video-polysomnographic documentation of 5 or more large body movements/hour during sleep, occurrence at least three times per week for at least 3 months and clinically significant impairment [11]. It is possible that this diagnosis was missed during this study since large body movements were not measured and restlessness was measured by only leg movements from the typical limb leads during polysomnography. However, our results may be similar to those found by Kapoor et al., when evaluating the large body movements with video polysomography in a group of children with ADHD. The authors found only a small percentage, 9.1%, of these children met criteria for restless sleep disorder. They concluded that other comorbid factors (OSA, RLS, medication) may result in the restlessness reported by the majority of parents, 81.1% of children with ADHD [12].
One of the limitations of this study is the small subject size due to its design as a pilot study. Obviously, a larger trial is needed to determine more of a cause-effect relationship. Also, the majority of the subjects were males and a future study needs to include an equal number of females. Another future direction would be a follow-up study after iron treatment to compare the amount of restlessness and daytime fatigue using objective measures.
References
- Bener A, Kamal M, Bener H, Bhugra D (2014) Higher prevalence of iron deficiency as strong predictor of attention deficit hyperactivity disorder in children. Ann Med Health Sci Res 4: 291-297.
- Konofal E, Lecendreux M, Arnulf I, Mouren MC (2004) Iron deficiency in children with attention-deficit/hyperactivity disorder. Arch PediatrAdolesc Med 158: 1113-1115.
- Felt BT, Biermann B, Christner JG, Kochhar P, Harrison RV (2014) Diagnosis and management of ADHD in children. Am Fam Physician 90: 456-464.
- Rosen GM, Morrissette S, Larson A, Stading P, Barnes TL (2019) Does improvement of low serum ferritin improve symptoms of restless legs syndrome in a cohort of pediatric patients? J Clin Sleep Med 15: 1149-1154.
- DelRosso LM, Mogavero MP, Baroni A, Bruni O, Ferri R (2021) Restless legs syndrome in children and adolescents. Child AdolescPsychiatrClin N Am 30: 143-157.
- Trotti LM (2017) Restless legs syndrome and sleep-related movement disorders. Continuum (MinneapMinn) 23: 1005-1016.
- DelRosso LM, Ferri R (2019) The prevalence of restless sleep disorder among a clinical sample of children and adolescents referred to a sleep centre. J Sleep Res 28: 12870.
- Konofal E, Lecendreux M, Deron J, Marchand M, Cortese S, et al. (2008) Effects of iron supplementation on attention deficit hyperactivity disorder in children. Pediatr Neurol 38: 20-26.
- Lam JC, Mark ME, Mason TBA, Scharf SM (2011) Defining the roles of actigraphy and parent logs for assessing sleep variables in preschool children. Behav Sleep Med 9: 184-193.
- Kushida CA, Littner MR, Morgenthaler T, Alessi CA, Bailey D, et al. (2005) Practice parameters for the indications for polysomnography and related procedures: An update for 2005. Sleep 28: 499-519.
- Delrosso LM, Ferri F, Allen RP, Bruni O, Garcia-Borreguero D, et al. (2020) Consensus diagnostic criteria for a newly defined pediatric sleep disorder: Restless Sleep Disorder (RSD). Sleep Med 75: 335-340.
- Kapoor V, Ferri R, Stein MA, Ruth C, Reed J, et al. (2021) Restless sleep disorder in children with attention-deficit/hyperactivity disorder. J Clin Sleep Med 17: 639-643.
Citation: Lam J, Ma J, Allen R (2021) A Case Series of Children with ADHD and Restless Sleep. J Neonatol Clin Pediatr 8: 088.
Copyright: © 2021 Janet Lam, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

