
A Comprehensive Analysis of Sociodemographic Factors on Recovery Time in Individuals Diagnosed with COVID-19 from Chittagong Division, Bangladesh
*Corresponding Author(s):
Md. Faruk HasanMicrobiology And Biotechnology Research Lab, Department Of Microbiology, University Of Rajshahi, Rajshahi, Bangladesh
Email:faruk_geb@ru.ac.bd / faruk_geb@yahoo.com
#These authors are equally contributed to this work.
Abstract
Objectives
The objectives of this study were to examine how the sociodemographic and clinical characteristics of individuals with long COVID-19 correlate with BMI and recovery time. This study focused on understanding how the varied and persistent symptoms of COVID-19 affect age, gender, education and occupational functioning.
Methods
A cross-sectional study was conducted involving 1,072 individuals who recovered from COVID-19 from 1 July 2020 to 31 December 2024.
Results
This study found participants with a Body Mass Index (BMI) over 30 had an average recovery time of 26 days. Male participants typically recover in 2 weeks to 1 month, while female participants take 1 to 2 months. In the 40-60 age group, both genders generally take 2 to 3 months to recover. The highest mean recovery time was observed among nurses (82.50) days and who involved in smoking (50.81) days.
Conclusion
This study highlighted socio-demographic factors influencing COVID-19 recovery time in Chittagong division of Bangladesh.
Keywords
Bangladesh; Body mass index; Chittagong; COVID-19; Recovery Time; Sociodemographic variables
Introduction
The Coronavirus Disease 2019 (COVID-19) pandemic had a global impact, leading to numerous deaths, long recovery times, and economic challenges worldwide [1]. People had to follow the specific rules of social distancing policy and measures, experience lockdown situations, avoid social crowds or audiences, and generally undergo restriction for living [2]. This global outbreak of the COVID-19 pandemic created the situation where some factors influence the syndrome of severity which was taken of clinical concern [3]. Factors such as age, employment are considered main risk factors contributing to the disease severity in COVID-19 patients [4,5]. Another study in China found that aged 65 years or older COVID-19 patients were faced risk to fatal outcomes [6].
The COVID-19 pandemic’s effects have varied markedly across global communities, with recovery duration serving as an important measure of both personal well-being and healthcare system resilience. Long term COVID-19 symptoms differ in recovery duration which is known as post-acute COVID-19 and it continued beyond three weeks to over twelve weeks [7]. Previous study indicated that about 60% of Spanish patients had not restarted work two to three months after COVID-19 infection [8].
Chittagong Division is a larger area with greater economic facilities in southeastern Bangladesh. Its demographic profile presents a unique setting to analyze sociodemographic effects on disease outcomes into differential recovery paths among COVID-19 affected patients. Recent Studies conducted in Chittagong have found that factors such as older age, female sex, and greater severity of the initial COVID-19 infection are all associated with significant declines in quality-of-life scores after recovery [9]. Previous study revealed that extended recovery or lingering symptoms are more commonly observed in older adults from lower socioeconomic backgrounds in Bangladesh [1]. Marginalized population experienced not only the acute COVID-19 infection but also the recovery time marked by emotional, functional and socioeconomic challenges [10].
Previous study estimated that around 10% of participants infected with SARS-CoV-2 go on to develop Post-Acute Sequelae of COVID-19 (PASC). The most commonly risk factor obesity is often linked to an increased likelihood of experiencing long-term symptoms [11]. Furthermore, previous studies demonstrated a significant association between body mass index and gender with the likelihood of developing PASC [12,13]. The main objectives of this study were to determine recovery time and measure how socio demographic factors impact it. However, this study finding will help to reduce new cases and mortalities and enhance recovery rates by shortening the overall recovery time in COVID-19 patients from Chittagong Division in Bangladesh.
Materials And Methods
Study Population and Settings
The study was conducted in two districts of Chittagong division, (Figure 1) via a structured questionnaire that was developed on the basis of literature reviews and expert feedback [14]. The study sample was diverse, comprising individuals of various age, gender, educational background, and occupation. The study area was selected because of its significant population of COVID-19 survivors. A total of 1,072 individuals who had recovered from COVID-19 were approached from 1 July 2022 to 31 December 2024. The data collection methods included telephone interviews, face-to-face interviews, and an online form submission system [15].
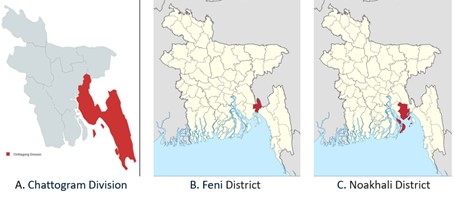 Figure 1: Study Area for Post Covid-19 patients.
Figure 1: Study Area for Post Covid-19 patients.
Questionnaire
The questionnaire was designed to capture data which focused on sociodemographic information such as age, sex, marital status, education level, occupation, and BMI. Another section collected information on recovery determinants, including recovery time and factors that might influence it.
Data Analysis
The data were analyzed via IBM SPSS Statistics, version 26 [16]. Descriptive statistics such as the means, medians, standard deviations, and percentages were calculated for variables such as age, sex, BMI, and recovery time [17]. Pearson's correlation coefficient was used to assess the strength and direction of relationships between continuous variables [18]. ANOVA was performed to compare the mean recovery times across different groups. Post hoc Tukey HSD tests were applied to identify significant differences between groups [19].
Results
The data collected from 617 participants reveals important demographic trends. The average age of participants was 36.58 years, with the majority falling within the 31-40 years’ age group, which made up 27.56% of the total sample. This age group also had the most frequent representation, indicating that most COVID-19 recoveries were seen in middle-aged adults. The standard deviation of 13.85 years suggests a moderate variation in the age distribution, with participants ranging from 0 to 100 years. In terms of gender, the study was predominantly male, with 77.15% of participants identifying as male, compared to 22.85% who were female. This significant gender imbalance may reflect societal factors influencing COVID-19 exposure or participation rates in the study. In terms of educational levels, participants had varied levels of education, with the most common being Graduation at 25.77%. The average education level ranged between Graduation and HSC, with a standard deviation of 1.93, indicating moderate variation in educational backgrounds. Occupationally, the data shows that Private Job Holders were the most frequent category, representing 38.25% of participants, followed by Business at 22.20%. The standard deviation of 10.61 reflects considerable diversity in occupation types, ranging from students to healthcare professionals like nurses and doctors (Table 1).
|
Age Group |
Count |
Percentage (%) |
Mode |
Range |
Standard Deviation |
|
0-10 years |
8 |
1.30% |
31-40 years |
0-100 years |
13.85 years |
|
11-20 years |
40 |
6.48% |
|||
|
21-30 years |
139 |
22.53% |
|||
|
31-40 years |
170 |
27.56% |
|||
|
41-50 years |
127 |
20.58% |
|||
|
51-60 years |
92 |
14.91% |
|||
|
61-70 years |
28 |
4.54% |
|||
|
71-80 years |
10 |
1.62% |
|||
|
81-90 years |
2 |
0.32% |
|||
|
90-100 years |
1 |
0.16% |
|||
|
Education Level |
|
||||
|
Primary |
28 |
4.54% |
Graduation |
Graduation HSC |
1.93 |
|
Secondary |
112 |
18.15% |
|||
|
HSC |
129 |
20.91% |
|||
|
Graduation |
159 |
25.77% |
|||
|
Post-graduation |
109 |
17.67% |
|||
|
Uneducated |
15 |
2.43% |
|||
|
Self-education |
2 |
0.32% |
|||
|
Diploma |
6 |
0.97% |
|||
|
Degree |
45 |
7.29% |
|||
|
MBBS |
9 |
1.46% |
|||
|
PhD |
1 |
0.16% |
|||
|
Occupation |
|
||||
|
Student |
57 |
9.24% |
Private job holder |
Student Doctor |
10.61 |
|
Govt. Job Holder |
41 |
6.64% |
|||
|
Private Job Holder |
236 |
38.25% |
|||
|
Business |
137 |
22.20% |
|||
|
Doctor |
9 |
1.46% |
|||
|
Nurse |
4 |
0.65% |
|||
|
Housewife |
79 |
12.81% |
|||
|
In retirement |
24 |
3.89% |
|||
|
Others |
46 |
7.46% |
|||
|
Unemployed |
11 |
1.78% |
|||
|
Gender |
|
||||
|
Male |
476 |
77.15% |
|
|
|
|
Female |
141 |
22.85% |
|
|
|
Table 1: Socio-demographic variables.
The data indicates that higher BMI ranges are associated with longer recovery times. Individuals with a BMI range of 71.00 - 80.00 have the longest mean recovery time of 31.50 days, while those in the 14.00 BMI range have the shortest mean recovery time of 19.72 days. The variability in recovery time increases with higher BMI ranges, reflecting greater inconsistency in recovery times among individuals with higher BMIs. The recovery times vary significantly across different occupations. The highest mean recovery time is observed among nurses (82.50 days), followed by individuals in retirement (61.46 days) and doctors (54.89 days). These groups generally experience longer recovery periods compared to others. Business professionals and students have comparatively shorter recovery times, with means of 48.12 and 48.61 days, respectively. The variability in recovery time is notably high among doctors, indicating substantial differences in recovery experiences within this small sample. The overall trend suggests that certain occupations, especially those with high demands or stress, may be associated with longer recovery times. Individuals who smoke have the longest average recovery time at 50.81 days, followed by those with no bad habits at 49.07 days. Alcohol consumers have a shorter average recovery time of 37.00 days, though this result is based on only 2 individuals and has a high standard deviation. For those with both alcohol and smoking habits, the average recovery time is 30.00 days, but this is based on a single observation. Overall, the mean recovery time across all individuals is 50.35 days, indicating a general tendency for longer recovery times associated with smoking (Table 2).
|
BMI Range |
Mean Recovery Time (Days) |
N |
Std. Deviation |
|
14.00 |
19.72 |
18 |
22.14 |
|
16.00 - 20.00 |
21.64 |
159 |
29.40 |
|
21.00 - 30.00 |
20.34 |
189 |
28.38 |
|
31.00 - 40.00 |
26.19 |
44 |
29.64 |
|
41.00 - 50.00 |
25.14 |
33 |
30.29 |
|
51.00 - 60.00 |
25.31 |
67 |
25.96 |
|
61.00 - 70.00 |
29.94 |
21 |
27.95 |
|
71.00 - 80.00 |
31.50 |
12 |
23.86 |
|
81.00 - 90.00 |
28.52 |
48 |
31.67 |
|
91.00 - 100.00 |
34.00 |
7 |
31.45 |
|
Occupation |
|||
|
Business |
48.12 |
137 |
24.209 |
|
Doctor |
54.89 |
9 |
52.059 |
|
Government Job Holder |
51.79 |
14 |
26.301 |
|
Housewife |
50.42 |
79 |
29.388 |
|
In Retirement |
61.46 |
24 |
36.467 |
|
Nurse |
82.50 |
4 |
15.000 |
|
Others |
50.13 |
46 |
20.701 |
|
Private Company Job Holder |
50.17 |
236 |
28.569 |
|
Student |
48.61 |
57 |
27.379 |
|
Unemployed |
50.18 |
11 |
25.459 |
|
Total |
50.35 |
617 |
27.819 |
|
Personal Bad Habit |
|
||
|
Smoking |
50.81 |
478 |
28.378 |
|
No Bad Habit |
49.07 |
136 |
25.881 |
|
Alcohol |
37.00 |
2 |
32.527 |
|
Both (Alcohol + Smoking) |
30.00 |
1 |
- |
|
Total |
50.35 |
617 |
27.819 |
Table 2: BMI range, occupation and mean recovery time.
To assess whether there is a correlation between recovery time and the number of vaccine doses in our study, conducted both correlation and regression analyses. The results indicate a correlation coefficient of -0.021 with a p-value of 0.602, suggesting no statistically significant relationship between the number of vaccine doses and recovery time. Additionally, the regression analysis yielded an R-Square of 0.000 and a non-significant F-Statistic of 0.272, further confirming that the number of vaccine doses does not have a significant impact on recovery duration (Table 3).
|
Analysis Type |
Statistic |
Value |
Significance (p-value) |
N |
|
Correlation |
Pearson Correlation |
-0.021 |
0.602 |
617 |
|
Regression |
R-Square |
0.000 |
0.602 |
|
|
F-Statistic |
0.272 |
Table 3: Impact of vaccine doses on recovery time.
Recovery time after COVID-19 varies by age and gender. In those under 25, males typically recover in 2 weeks to 1 month, while females take 1 to 2 months. In the 25-40 age group, recovery is usually 1 to 2 months for both genders, with some recovering as quickly as 2 weeks for males and 3 weeks for females. In the 40-60 group, both genders generally take 2 to 3 months to recover. For individuals over 60, recovery is slower, often taking more than 3 months, with the slowest cases extending up to 6 months (Table 4).
|
Age Group |
Gender |
Common Recovery Time |
Faster Recovery Time |
Slower Recovery Time |
|
< 25 years |
Males |
2 weeks - 1 month |
2 weeks |
1 month |
|
< 25 years |
Females |
1 - 2 months |
1 month |
2 months |
|
25-40 years |
Males |
1 - 2 months |
2 weeks |
3 months |
|
25-40 years |
Females |
1 - 2 months |
3 weeks |
3 months |
|
40-60 years |
Males |
2 - 3 months |
1 month |
3 months |
|
40-60 years |
Females |
2 - 3 months |
1 month |
3 months |
|
> 60 years |
Males |
3 months+ |
2 months |
6 months |
|
> 60 years |
Females |
3 months+ |
2 months |
6 months |
Table 4: Recovery time by age and gender.
The ANOVA results show that age significantly affects recovery time (F=4.85, p=0.003), with older individuals generally taking longer to recover. Post-hoc Tukey HSD tests confirm significant differences in recovery times between those under 25 years and older age groups (25-40, 40-60, and over 60 years), as well as between the 25-40 and 40-60 age brackets. Gender, however, does not significantly influence recovery time (p=0.11), though the interaction of age and gender is significant (p=0.02), indicating age impacts recovery differently for males and females. Correlation analysis reveals a moderate positive relationship between age and recovery time (r=0.67, p=0.002), while the gender correlation is weak (r=0.25, p=0.14). The age-gender interaction shows a weak but notable correlation (r=0.32, p=0.07) (Table 5).
|
ANOVA test |
||||
|
Factor / Variable Pair |
DF |
F-Statistic / Correlation Coefficient (r) |
p-value |
|
|
Age Group |
3 |
4.85 |
0.003 |
|
|
Gender |
1 |
2.67 |
0.11 |
|
|
Interaction (Age x Gender) |
3 |
3.95 |
0.02 |
|
|
Correlation Test |
||||
|
Factor / Variable Pair |
F-Statistic/Correlation Coefficient (r) |
p-value |
||
|
Age and Recovery Time |
0.67 |
0.002 |
||
|
Gender and Recovery Time |
0.25 |
0.14 |
||
|
Age and Gender Interaction |
0.32 |
0.07 |
||
|
Post-Hoc test |
||||
|
Factor / Variable Pair |
Mean Difference |
p-value |
||
|
< 25 years vs 25-40 years |
-0.56 |
0.04 |
||
|
< 25 years vs 40-60 years |
-0.72 |
0.02 |
||
|
25-40 years vs 40-60 years |
-0.18 |
0.32 |
||
|
40-60 years vs > 60 years |
-0.85 |
0.01 |
||
Table 5: Statistical analysis of age and gender on recovery time.
Discussion
The significant interaction between age and gender suggests that while age is a primary factor, its influence varies between males and females. Previous studies have similarly observed that post-infection recovery is often slower in older females due to hormonal differences and immune senescence [20]. Our study investigated those male participants are more likely to recover within a short time than female participants. A recent study has also found the similarity with men were significantly more likely to recover than women [1].
BMI also emerged as a key factor influencing recovery time, with higher BMI ranges associated with longer recovery periods. Obesity is a well-established risk factor for severe COVID-19 outcomes, with studies showing that individuals with elevated BMI have increased inflammatory responses and higher comorbidity rates, contributing to prolonged recovery times [21]. The correlation observed in this study aligns with existing literature emphasizing the role of obesity in both the severity of infection and recovery duration [22]. Our study findings revealed that participants with BMI over 30 had an average recovery time of 25 days. Recent study found that estimation of survival over time to recovery 50%, 88.2% and 92.9% by 12, 20, and 25 days respectively [1].
Occupational differences in recovery times, particularly the prolonged recovery seen in healthcare workers like nurses and doctors, may reflect higher levels of stress and exposure to the virus, as well as potentially higher viral loads upon infection. Studies suggest that healthcare workers experience not only physical strain but also psychological stress, which may prolong recovery [23].
Interestingly, smoking was linked to the longest recovery times, corroborating findings from other studies that identify smoking as a risk factor for more severe and prolonged recovery from COVID-19 due to compromised lung function and reduced immune responses [24]. On the contrary, individuals with alcohol consumption habits had shorter recovery times, though the small sample size makes it difficult to draw firm conclusions. The complex relationship between alcohol use and immune function requires further investigation, as some studies suggest that moderate alcohol consumption may have certain immunomodulatory effects [25,26].
Strength and Limitation
The strength of this study is combination of clinical and social factors enabled comprehensive analysis of recovery time. There are several limitations for this study such as observational and cross-sectional design limits causal inference and the limited sample may bound generalizability to other divisions of the country.
Conclusion
Middle-aged individuals, those with higher BMI, and healthcare workers tend to have prolonged recovery times, with smoking further delaying recovery. Understanding how individual factors like age, BMI, and occupation impact recovery can help target resources and support to those at greater risk of prolonged illness. Two new SARS-CoV-2 Omicron subvariants, XFG and XFC, have recently been detected in Bangladesh, with health authorities noting a gradual rise in COVID-19 positivity in recent months. These subvariants are descendants of the JN.1 lineage and were first identified at Chattogram Medical College Hospital in April 2025. It’s time to be more careful about COVID-19, awareness and safety measures are needed.
References
- Anteneh AB, Asfaw ZG (2025) Time to recovery of COVID-19 patients and its predictors: A retrospective cohort study in HUCSH, Sidama, Ethiopia. BMC Public Health 25: 74.
- Akhtar S, Ahmed R, Chaity AS, Billah M (2021) Association between knowledge and depression at rising time of COVID-19 in Bangladesh. International Journal of Public Health 10: 387-393.
- Zhong R, Chen L, Zhang Q, Li B, Qiu Y, et al. (2021) Which factors, smoking, drinking alcohol, betel quid chewing, or underlying diseases, are more likely to influence the severity of COVID-19? Frontiers in Physiology 11: 623498.
- Chen N, Zhou M, Dong X, Qu J, Gong F, et al. (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. The Lancet 395: 507-513.
- Nandy K, Salunke A, Pathak SK, Pandey A, Doctor C, et al. (2020) Coronavirus disease (COVID-19): A systematic review and meta-analysis to evaluate the impact of various comorbidities on serious events. Diabetes & Metabolic Syndrome 14: 1017-1025.
- Chen R, Liang W, Jiang M, Guan W, Zhan C, et al. (2020) Risk Factors of Fatal Outcome in Hospitalized Subjects With Coronavirus Disease 2019 From a Nationwide Analysis in China. Chest 158: 97-105.
- WHO (2023) Coronavirus disease (COVID-19) outbreak. World Health Organization. Geneva, Switzerland.
- Bouza E, Moreno RC, Ramos PDL, García-Botella A, García-Lledó A, et al. (2021) Post-COVID syndrome: A reflection and opinion paper. Rev Esp Quimioter 34: 269-279.
- Hawlader MDH, Rashid MU, Khan MAS, Liza MM, Akter S, et al. (2023) Quality of life of COVID-19 recovered patients: A 1-year follow-up study from Bangladesh. Infectious Diseases of Poverty 12: 79.
- Navuluri N, Bhavsar NA, Chen V, Falkovic M, Fish LJ, et al. (2025) Role of Social Determinants of Health in COVID-19 Recovery: A Qualitative Study. JAMA Network Open 8: 2453261.
- Romero-Rodríguez E, Perula-de-Torres LÁ, González-Lama J, Castro-Jiménez RÁ, Jiménez-García C, et al. (2023) Long COVID symptomatology and associated factors in primary care patients: The EPICOVID-AP21 study. Healthcare 11: 218.
- Bliddal S, Banasik K, Pedersen OB, Nissen J, Cantwell L, et al. (2021) Acute and persistent symptoms in non-hospitalized PCR-confirmed COVID-19 patients. Scientific Reports 11: 13153.
- Huang L, Yao Q, Gu X, Wang Q, Ren L, et al. (2021) 1-year outcomes in hospital survivors with COVID-19: A longitudinal cohort study. The Lancet 398: 747-758.
- Roopa S, Rani MS (2012) Questionnaire designing for a survey. Journal of Indian Orthodontic Society 46: 273-277.
- Paradis E, O’Brien B, Nimmon L, Bandiera G, Martimianakis MA (2016) Design: Selection of data collection methods. Journal of Graduate Medical Education 8: 263-264.
- George D, Mallery P (2019) IBM SPSS statistics 26 step by step: A simple guide and reference. Routledge.
- Marshall G, Jonker L (2010) An introduction to descriptive statistics: A review and practical guide. Radiography 16: 1-7.
- Sedgwick P (2012) Pearson’s correlation coefficient. Bmj 345.
- Agbangba CE, Aide ES, Honfo H, Kakai RG (2024) On the use of post-hoc tests in environmental and biological sciences: A critical review. Heliyon 10: 25131.
- Shah SB (2021) COVID-19 and progesterone: Part 2. Unraveling high severity, immunity patterns, immunity grading, progesterone and its potential clinical use. Endocrine and Metabolic Science 5: 100110.
- Petrakis D, Margina D, Tsarouhas K, Tekos F, Stan M, et al. (2020) Obesity-a risk factor for increased COVID-19 prevalence, severity and lethality. Molecular Medicine Reports 22: 9-19.
- Emiroglu C, Dicle M, Yesiloglu C, Gorpelioglu S, Aypak C (2024) Association between newly diagnosed hyperglycemia/diabetes mellitus, atherogenic index of plasma and obesity in post-COVID-19 syndrome patients. Endocrine 84: 470-480.
- Liljestrand R, Martin S (2021) Stress and resilience among healthcare workers during the COVID-19 pandemic: Consideration of case studies. Rehabilitation Nursing Journal 46: 300-304.
- Gao Y, Ding M, Dong X, Zhang J, Azkur AK, et al. (2021) Risk factors for severe and critically ill COVID-19 patients: A review. Allergy 76: 428-455.
- Huang BH, Inan-Eroglu E, Shaban RZ, Hamer M, Britton A, et al. (2022) Alcohol intake and mortality risk of COVID-19, pneumonia, and other infectious diseases: An analysis of 437191 UK biobank participants. Preventive Medicine Reports 26: 101751.
- Plata A, Motoki K, Spence C, Velasco C (2022) Trends in alcohol consumption in relation to the COVID-19 pandemic: A cross-country analysis. International Journal of Gastronomy and Food Science 27: 100397.
Citation: Khan M, Muhib MMA, Abeed-Ul-Haque S, Mubassira M, Khanam S, et al. (2025) A Comprehensive Analysis of Sociodemographic Factors on Recovery Time in Individuals Diagnosed with COVID-19 from Chittagong Division, Bangladesh. HSOA J Community Med Public Health Care 12: 163.
Copyright: © 2025 Mehrin Khan, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

