
A Recovered Case of Massive Pericardial Effusion with Impending Cardiac Tamponade: An Atypical Presentation of COVID-19
*Corresponding Author(s):
Noor-E-Elahi MozumderDepartment Of Cardiac Surgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
Tel:+880 1813750616,
Email:dr.nooreelahiraju@gmail.com
Abstract
COVID-19 became a global health emergency due to its highly contagious nature. A substantial number of patients have been presented in emergency with acute COVID-19 Cardiovascular Syndrome (ACovCS). Pericardial involvement has been reported rarely so far. We report a case of massive pericardial effusion with impending cardiac tamponade in a COVID-19 patient. Pericardial fluid drainage done urgently using CV catheter under echocardiographic guidance and 1000ml of sero-hemorrhagic fluid drained. Thorough investigation revealed cytokine storm and no other apparent cause of pericardial effusion. Critical clinical evaluation of cardiovascular system of patients with COVID-19 is essential to save lives.
Introduction
Since its emergence in Wuhan, China, a novel coronavirus, Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) has affected almost every country of the world. Coronavirus disease 2019 (COVID-19) has become a global health emergency due to its high infectivity along with significant morbidity and mortality [1,2]. According to the Johns Hopkins COVID-19 resource center, more than 14 million people have been infected with this virus worldwide with more than six hundred thousand mortality confirmed up to 20 July, 2020 [3]. Though fever, cough, myalgia and shortness of breath have been considered as common symptoms, patient may develop serious complications like Acute Respiratory Distress Syndrome (ARDS), cardiac injury and secondary super infection, which can lead to death [4]. Substantial number of COVID-19 patients have been presented with acute coronary syndrome (STEMI or NSTEMI), acute myocardial injury without obstructive coronary artery disease, arrhythmias, heart failure ± cardiogenic shock, pericardial effusion, thromboembolic complications, which have been termed as acute COVID-19 Cardiovascular Syndrome (ACovCS) [5]. In this context, we are reporting a case of COVID-19 complicated with massive pericardial effusion with impending cardiac tamponade and we have found that no such massive effusion case has been reported yet.
Case Report
A 54 year old hypertensive, type-2 diabetic woman presented to the emergency department with orthopnea, dyspnea, fever, cough, myalgia, nausea, anorexia for 6 days. Three members of her family was suffering from fever and 1 day back her son tested positive for SARS-CoV-2. On physical examination, she was found anxious, febrile (100°C), dyspneic (aggravates on lying down). Her oxygen saturation was 98%, respiratory rate 32 breaths/min, heart rate 122bpm, pulse was feeble, pulsus paradoxus present and heart sound was muffled. She also had raised JVP, diminished breath sound in left lower lung field, bilateral leg edema. Admission ECG showed sinus tachycardia with low voltage ECG wave. After initial management, her nasopharyngeal swab was sent for RT-PCR of SARS-CoV-2 and CT scan of chest was done which revealed pericardial effusion and collapse of left lower lung (Figure 1).
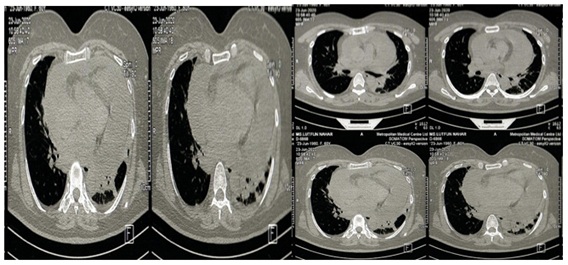 Figure1: CT scan of chest.
Figure1: CT scan of chest.
She was found RT-PCR positive for SARS-CoV-2 and emergency echocardiography revealed severe circumferential pericardial effusion (30mm) with partial collapse of right atrium. Patient was immediately taken to operating room for pericardial fluid drainage. On operating table her blood pressure was 80/40mm Hg, pulse- 130 beats/min, SpO2- 92% without oxygen and there was arrhythmia on ECG. Immediate pericardial fluid drainage done in minimal invasive way using CV catheter in seldinger technique under echocardiographic guidance from subcostal approach and 1000ml of sero-hemorrhagic fluid was drained. Pericardial fluid was sent for physical, biochemical, cytological and microbiological study. Patient’s clinical condition improved significantly after drainage of pericardial fluid. Continuous pericardial drainage was maintained by CV catheter in situ for 72 hours and a total of 1250ml of fluid was drained. Pericardial fluid study revealed no malignant cell, negative for Gram stain and acid-fast bacilli smear, no growth on bacterial and fungal culture, WBC- 700/mm3 (polymorph- 95%, lymphocyte- 5%), glucose- 3.41mmol/L, protein- 29.76g/L. RT-PCR of pericardial fluid couldn’t be done due to lack of facility. Thyroid function test and serum albumin was normal. After 72 hours chest x-ray revealed no effusion and ECG revealed anterior ischemia (T wave inversion in lead V1-V6). Abnormal laboratory test findings were ESR- 69mm in 1st hour, CRP- 48mg/l, D-Dimer- 9.8mg/l, NT-pro BNP- 1423pg/ml and Ferritin- 880.2ng/ml which reflects about cytokine storm in body.
Patient was treated with broad spectrum antibiotics, methyl prednisolone, diuretics, ACEI, beta blocker, LMWH and other supportive management for COVID-19. She became afebrile after 7 days and found RT-PCR negative for COVID-19 after 12 days. She was discharged as her clinical condition improved overall. She came to follow-up after 2 weeks and routine investigations including ECG, Echocardiography were done. T inversion was no longer present on chest leads of ECG and Echocardiography showed good left ventricular function (EF-67%), no regional wall motion abnormality and minimal (2mm) posterior effusion (Figure 2). Other routine tests revealed normal finding.
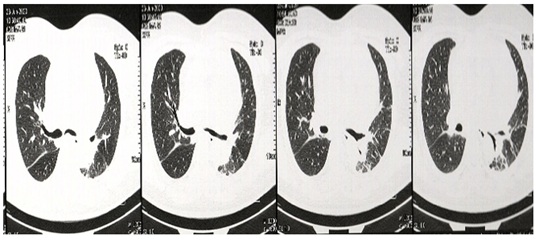
Figure 2: Echocardiography.
Discussion
The virus crosses the cell membrane and invades the cell by binding with a protein, Angiotensin Converting Enzyme 2 (ACE-2), which is found abundantly in pneumocytes and myocytes, which explains the affinity of COVID-19 towards respiratory and cardiovascular system [6]. Cardiovascular complications have been found in most of the critically ill patients along with systemic and respiratory complications and it is a leading cause of death in COVID-19 [7-10]. Among acute COVID-19 cardiovascular syndromes, acute coronary syndrome and myocardial injury are reported commonly and pericardial involvement has been reported rarely. A meta-analysis of chest CT findings of 2738 COVID-19 patients reported pericardial effusion in 4.55% of patients [11]. We have found 4 reported cases of cardiac tamponade with COVID-19. Among them 3 patients had preexisting cardiac disease (cardiomyopathy and myopericarditis) and 1 patient developed mechanical ventilation associated tamponade [12-15]. We are reporting the case of impending cardiac tamponade due to massive sero-hemorrhagic pericardial effusion with COVID-19, which we urgently drained in minimal invasive way using CV catheter in seldinger technique under echocardiographic guidance. Patient also had cytokine release syndrome as reflected by raised ESR, CRP, D-Dimer, Ferritin, LDH and lymphopenia. The patient had no previous history of angina, myocarditis or cardiac injury which was demonstrated by normal troponin-I level, no regional wall motion abnormality and good ejection fraction on echocardiography. Pericardial effusion is a common manifestation of viral pericarditis which can lead to cardiac tamponade, but such massive effusion is rare. Exact mechanism of cardiac involvement of COVID-19 hasn’t been understood yet, but it has been hypothesized that direct viral invasion or autoimmune type reaction leading to cytokine storm and exaggerated systemic inflammatory response may be responsible [13-16]. However, direct mechanism of pericarditis and pericardial effusion due to COVID-19 is still unclear. So far, only one case has been reported RT-PCR positive of pericardial fluid with several false negative results [14,17]. Thus, RT-PCR of pericardial fluid in case of pericardial effusion is conclusory for COVID-19, clinical correlation needed rather and CV catheter can be used for emergency pericardiocentesis in impending cardiac tamponade, especially in this pandemic situation.
Conclusion
Critical clinical evaluation of cardiovascular system of every COVID-19 patient in emergency department is necessary. Quick anticipation and timely intervention can save lives during this pandemic.
References
- Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: Summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA 323: 1239-1242.
- Chen N, Zhou M, Dong X, Qu J, Gong F, et al. (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. The Lancet 395: 507-513.
- John Hopkins Coronavirus Resource Center (2020) COVID-19 Map. John Hopkins Coronavirus Resource Center, USA.
- Irabien-Ortiz Á, Carreras-Mora J, Sionis A, Pàmies J, Montiel J, et al. (2020) Fulminant myocarditis due to COVID-19. Rev Esp Cardiol 73: 503-515.
- Hendren NS, Dranzer MH, Bozkurt B, Cooper LT (2020) Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation 141: 1903-1914.
- Coyle J, Igbinomwanhia E, Sanchez-Nadales A, Danciu S, Shah N (2020) A recovered case of COVID-19 myocarditis and ARDS treated with corticosteroids, tocilizumab and experimental AT-001. JACC: Case Reports 2: 1331-1336.
- Guo T, Fan Y, Chen M, Wu X, Zhang L, et al. (2020) Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol 5: 811-818.
- Babapoor-Farrokhran S, Gill D, Walker J, Rasekhi RT, Bozorgnia B, et al. (2020) Myocardial injury and COVID-19: Possible mechanisms. Life Sciences 253: 117723.
- Shi S, Qin M, Shen B, Cai Y, Liu T, et al. (2020) Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol 5: 802-810.
- Ruan Q, Yang K, Wang W, Jiang L, Song J (2020) Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med 46: 846-848.
- Bao C, Liu X, Zhang H, Li Y, Liu J (2020) Coronavirus disease 2019 (COVID-19) CT findings: A systematic review and Meta-analysis. J Am Coll Radiol 17: 701-709.
- Hua A, O’Gallagher K, Sado D, Byrne J (2020) Life-threatening cardiac tamponade complicating myo-pericarditis in COVID-19. Eur Heart J 41: 2130.
- Dabbagh MF, Aurora L, D’Souza P, Weinman AJ, Bhargava P, et al. (2020) Cardiac tamponade secondary to COVID-19. J Am Coll cardio Case Rep 2: 1326-1330.
- Farina A, Uccello G, Spreafico M, Bassanelli G, Savonitto S (2020) SARS-CoV-2 detection in the pericardial fluid of a patient with cardiac tamponade. European Journal of Internal Medicine 76: 100-101.
- Derveni V, Kaniaris E, Toumpanakis D, Potamianou E, Ioannidou I, et al. (2020) Acute life-threatening cardiac tamponade in a mechanically ventilated patient with COVID-19 pneumonia. ID Cases 21: 00898.
- Adler Y, Charron P, Imazio M, Badano L, Barón-Esquivias G, et al. (2015) 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The task force for the diagnosis and management of pericardial diseases of the European Society of Cardiology (ESC) Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 36: 2921-2964.
- Hanson K, Caliendo C, Arias CA, Hayden MK, Englund JA, et al. (2020) Infectious Disease Society of America guidelines on the diagnosis of COVID-19. IDSA.
Appendix A: Supplementary Data
A) Serial evaluation of ECG
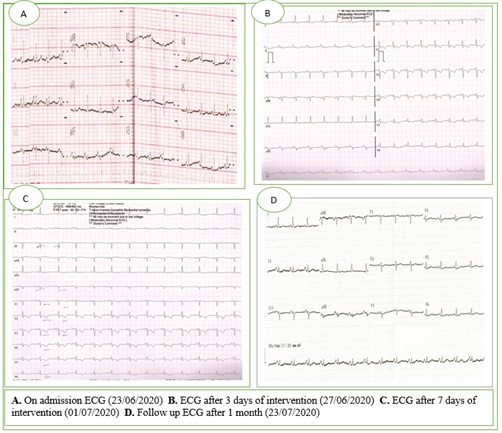
B) CT scan of chest
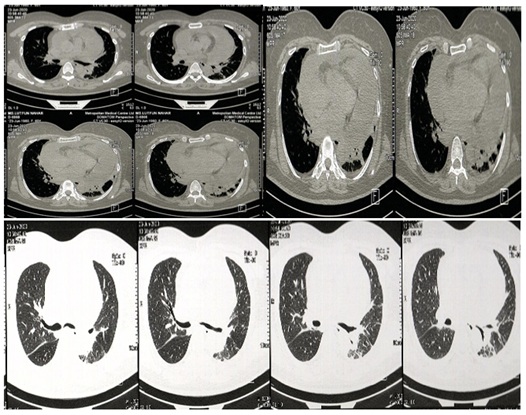
C) Echocardiography before intervention
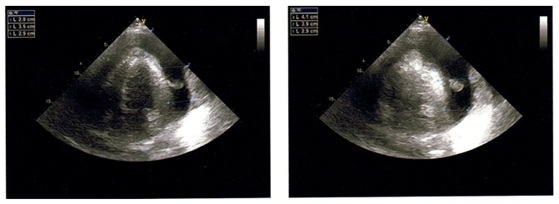
D) Follow-up Echocardiography after 1 month
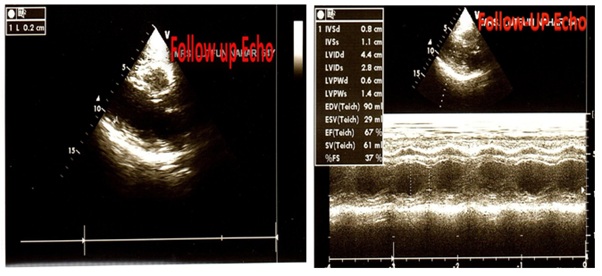
E) Chest X-ray P/A View
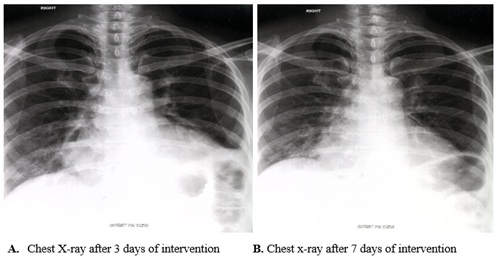
F) Laboratory results
|
Variable |
Reference Range |
23rd June |
25th June |
27th June |
1st July |
5th July |
10th July |
|
Hemoglobin (g/dl) |
11.5-16.5 |
11.2 |
12.6 |
12.1 |
12.9 |
10.8 |
|
|
Hematocrit (%) |
35-45 |
37.6 |
39.1 |
38.1 |
43.1 |
37.1 |
|
|
ESR (mm in 1st hour) |
0-20 |
69 |
20 |
26 |
25 |
25 |
|
|
RBC (per µl) |
4.3±0.5×106 |
5.10×106 |
5.75×106 |
5.75×106 |
6.21×106 |
5.25×106 |
|
|
WBC (per µl) |
7.0±3.0×109 |
11.5×109 |
11.5×109 |
6.76×103 |
9×103 |
9×103 |
|
|
Neutrophil (%) |
40-75 |
78 |
76 |
67 |
71 |
39 |
|
|
Lymphocyte (%) |
20-45 |
19 |
19 |
30 |
25 |
55 |
|
|
Platelet (per µl) |
150-450×103 |
170×103 |
273×103 |
505×103 |
585×103 |
410×103 |
|
|
CRP (mg/l) |
<5 |
48 |
2.14 |
||||
|
D-Dimer (µg/ml) |
<0.50 |
9.8 |
1.51 |
3.87 |
3.87 |
0.49 |
|
|
Troponin-I (ng/ml) |
<0.04 |
Negative |
|||||
|
NT-pro BNP (pg/ml) |
<300 |
1423 |
|||||
|
Ferritin (ng/ml) |
10-120 |
880.2 |
447.3 |
||||
|
LDH (U/l) |
200-400 |
398.1 |
|||||
|
Prothrombin time (sec) |
12-16. |
14.5 |
13.1 |
12.5 |
|||
|
APTT (sec) |
20-40 |
44.2 |
30 |
26.9 |
26.9 |
45 |
36.3 |
|
Sodium (mmol/l) |
135-145 |
130.4 |
130.4 |
137 |
137 |
134 |
|
|
Potassium (mmol/l) |
3.5-5.0 |
4.3 |
4.3 |
4 |
4.7 |
4.4 |
|
|
Albumin (g/l) |
35-50 |
32 |
|||||
|
TSH (µIU/ml) |
0.35-5.5 |
1.02 |
|||||
|
Creatinine (mg/dl) |
0.5-1.2 |
1.1 |
0.73 |
||||
|
SGPT (U/l) |
<40 |
43 |
24 |
||||
|
RT-PCR for SARS-Cov-2 |
Positive |
Negative |
Citation: Mozumder NEE, Imtiaz MN, Khan OS, Hoque R, Rahman KA, et al. (2021) A Recovered Case of Massive Pericardial Effusion with Impending Cardiac Tamponade: An Atypical Presentation of COVID-19. Archiv Surg S Educ 3: 013.
Copyright: © 2021 Noor-E-Elahi Mozumder, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

