
A Retrospective Study on the Application of Guided Rehabilitation Training In the Rehabilitation of Children with Peripheral Facial Paralysis
*Corresponding Author(s):
Lin YangKey Laboratory Of Rehabilitation Medicine, West China Hospital, Sichuan University, Sichuan University, China
Email:green.yanglin@scu.edu.cn
Abstract
Objective
To observe the clinical efficacy of guided rehabilitation training in the treatment of peripheral facial paralysis in children.
Methods
Thirty-eight children with peripheral facial paralysis who met the inclusion and exclusion criteria were enrolled, and the patients were treated with conventional training and guided rehabilitation training respectively. The Portmann facial function score sheet and compliance score sheet were used for evaluation before and after treatment.
Results
Both groups of patients obtained good treatment effects. The compliance of patients in the treatment group was significantly higher than that of the control group, and the treatment effect was significantly better than the control group. Conclusion: guided rehabilitation training has a good clinical effect in the treatment of peripheral facial paralysis in children.
Keywords
Guided rehabilitation training; Peripheral facial paralysis in children; Physiotherapy
Introduction
Peripheral facial paralysis in children is a common neurological dysfunction, which idiopathic peripheral facial paralysis (Bell facial paralysis) is the most common accounting for 79.9% [1]. Although idiopathic facial paralysis is self-limiting and self-healing, the function of a considerable part of patients with facial paralysis cannot be fully recovered [2]. Due to face has the function of communication and expression, long-term facial dysfunction will not only affect the health of the eyes, oral cavity, and other organs, but will also harm children's communication, psychology, social participation, and quality of life [3].
The difficulty in the rehabilitation of children with facial paralysis, in addition to the disease itself, mainly depends on the cooperation of the children. Due to the young age, cooperation is often insufficient. Therefore, it is very important to seek a treatment method with good adaptability, short duration, and satisfactory curative effect. Guided education is a rehabilitation treatment model and concept that actively promotes children's participation and gradually improves physical and communication functions. Guided education is mainly used in children with cerebral palsy and has achieved good intervention effects [4,5], but there is no research report on whether it can be applied in children with peripheral facial paralysis.
The overall incidence of facial paralysis in children is lacking, for this study will conduct a retrospective study on the efficacy of guided education in the rehabilitation of children with facial paralysis. Through the analysis of the curative effect of the outpatient treatment of children with facial paralysis from July 2013 to November 2020, the curative effect of the guided education training mode on children with facial paralysis was explored. We summarize the treatment experience and formulate a more effective overall treatment strategy for young children with facial paralysis.
Material And Methods
Normal material
A total of 53 children with facial paralysis who were treated at the Rehabilitation Medicine Center of West China Hospital of Sichuan University from July 2013 to July 2021 were selected. During the treatment, the therapists performed conventional physical therapy and guided therapy on the patients based on their technical direction. The study was authorized by the Ethics Committee of West China Hospital, Sichuan University.
Inclusion criteria
(1) Idiopathic peripheral facial paralysis diagnosed according to the clinical diagnostic criteria [6]; (2) Age < 6 years old; (3)vDuration of disease < 3 months; (4) Complete data, treatment, and follow-up time ≥1 month. Exclusion criteria: (1)Facial paralysis caused by or complicated by tumor and infection; (2) Combined with severe liver and kidney disease, cardiovascular and mental diseases; (3) Cannot cooperate to complete the whole treatment and follow-up.
According to the above criteria, the patients were selected according to age, gender, course of the disease, functional score, and compliance score. SPSS23.0 was used for 1:1 propensity matching, and 38 patients were finally included in the statistics. The sample size of the study was calculated, and the functional disability score was used as the main evaluation index. The test level was α=0.05, and the test power was 1-β=0.90.
According to the previous research standards and the sample size calculation formula N=[(2(μa+μb)σ)/Δ]2, the total sample size N=24, that is, the total sample size should not be less than 24. Thirty-eight patients were included in this study, which met statistical needs.
The general information of the patients is shown in (Table 1).
|
Group |
Sex (male/female)* |
Age (y)@ |
Onset (d)#
|
Functional score #
|
Assessment of compliance# |
||||
|
1(%) |
2(%) |
3(%)
|
4(%) |
5(%) |
|||||
|
Control group |
10:9 |
4.3±1.7 |
35.6±14.3 |
2.1±1.5 |
3(15.8) |
7(36.8) |
9(47.4) |
0(0) |
0(0) |
|
Treatment group |
12:7 |
4.6±1.8 |
33.1±14.0 |
1.5±1.1 |
5(26.3) |
3(15.8) |
11(59.7) |
0(0) |
0(0) |
Table 1: Basic information of patients before treatment.
*Chi-square test, P=0.743, no statistical difference
@Independent samples t-test, P=0.585, no statistical difference
#Rank sum test, P>0.05, no statistical difference
1.2 treatment method
The treatment group received physical factor therapy and guided rehabilitation training, the control group received similar physical factor therapy and conventional exercise therapy.
Physical factor therapy
(1) Ultrashort-wave electrotherapy (Shantou DL-C II facial features ultrashort-wave electrotherapy machine) The patient is seated, and the mid-round electrode is placed on the affected side mastoid and the healthy side ear, no heat to slight heat, energized for 10 minutes. (2) DC drug iontophoresis (Beijing K8832-T computer multifunctional electrotherapy apparatus) The patient was in a supine position. Add an injection containing 1100 mg of vitamin B1 to a filter cloth soaked in an appropriate amount of distilled water, place it on the affected side, then put a fleece mask electrode connected to the positive electrode, and the auxiliary electrode is placed on the waist connected to the negative electrode, using the 20-gauge DC iontophoresis prescription, the current intensity is 1 ~ 3mA , 20 min;(3) Intermediate frequency electrotherapy (Beijing K8832-T computer multi-functional electrotherapy apparatus) The patient was placed in the supine position, and the No. 3 neuritis prescription was used for 20 minutes. Various physical factors were treated once a day, 5 times a week for 4 weeks.
Conventional exercise therapy: According to the dysfunction of the facial expression muscles of the child, the patients were subjected to local stretching, relaxation, stimulation, and other techniques, and five basic movements of raising eyebrows, closing eyes, whistling, showing teeth, and puffing cheeks were selected, cooperating with partial relaxation, manipulation and other methods for expressive muscle training. Each training session is about 30 minutes, 5 times a week, for a total of 4 weeks. Instruct the parents to conduct relevant facial expression muscle training at home every day according to the therapist's method. Treatment is done by therapist A. Therapist A has 5 years of experience in the treatment of facial paralysis.
Guided rehabilitation training: According to the facial expression muscle dysfunction of children, based on conventional exercise therapy, combined with guided education. In training, through game interaction and other methods, it can achieve facial sensory stimulation, neuromuscular function promotion, muscle strength training, coordination training, etc. [7,8]. Each training session is about 30 minutes, 5 times a week, for a total of 4 weeks. The family members were instructed to complete the relevant facial exercise training in a guided learning mode after returning home. The treatment is completed by therapist B, who has 10+ years of experience in the treatment of facial paralysis.
Assessment methods
The facial function of the patients was evaluated by the facial paralysis Portmann scale [9,10], and the patients were evaluated before treatment and after 4 weeks of treatment. At the same time, the patients' compliance was assessed before treatment, 2 weeks after treatment, 4 weeks after treatment.
Statistical methods
The data obtained in this study were expressed as (X±SD), and SPSS 23.0 statistical software was used for data analysis, using t test; enumeration data using the chi-square test, P < 0.05 indicated that the difference was statistically significant.
Results
Differences in facial function score (Portmann score) between the two groups before and after treatment (Table 2)
|
Group |
Before |
After |
Improvement |
|
1 |
2.0±1.5? |
14.6±2.4* |
12.5±2.9? |
|
2 |
1.5±1.1? |
17.3±2.8# |
15.7±3.2? |
Table 2: Comparison of facial function after 1 month of treatment (X±SD)
*Paired sample t-test for the control group, p= 0.00, there was a statistical difference between before and after treatment
# Paired sample t-test for treatment group, p=0.00, there was a statistical difference between before and after treatment
?Comparison of the two groups before treatment, independent samples t-test: p=0.231, there was no statistical difference
?The degree of improvement, independent sample t test, p=0.002, there was a statistical difference
Differences in compliance between the two groups before and after treatment (Table 3)
|
Times |
Compliance score |
Control group |
Treatment group |
|
1(before)* |
1 |
3 (15.8) |
5(26.3) |
|
2 |
7(36.8) |
3(15.8) |
|
|
3 |
9(47.4) |
11(57.9) |
|
|
4 |
0(0) |
0(0) |
|
|
5 |
0(0) |
0(0) |
|
|
2(2week)# |
1 |
0(0) |
0(0) |
|
2 |
8(42.1) |
1(5.3) |
|
|
3 |
5(26.3) |
4(42.1) |
|
|
4 |
6(31.6) |
9(36.8) |
|
|
5 |
0(0) |
5(15.8) |
|
|
3(4week)# |
1 |
0(0) |
0(0) |
|
2 |
1(5.3) |
0(0) |
|
|
3 |
8(42.1) |
0(0) |
|
|
4 |
7(36.8) |
5(26.3) |
|
|
5 |
3(15.8) |
14(73.7) |
Table 3: Compliance between treatment group and control group (number of cases, %).
*Independent sample rank-sum test, P>0.05, no statistical difference
#Independent sample rank-sum test, p < 0.05, there is a statistical difference
The results showed that there was no significant difference in compliance between the two groups before treatment (P>0.05). After 2 weeks and 4 weeks of treatment, the compliance of children in the treatment group was significantly higher than that in the control group (P < 0.05).
The effect of adherence on treatment outcomes (Figure 1)
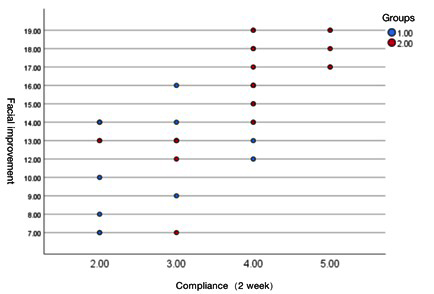 Figure 1: Correlation between facial improvement and compliance (2 weeks).
Figure 1: Correlation between facial improvement and compliance (2 weeks).
The correlation between compliance and treatment effect, using correlation analysis, compared the patient's facial function score at 4 weeks with the patient's compliance score at 2 weeks. The Spearman method was used for statistics, and the correlation coefficient was 0.734, p=0.00, indicating that compliance was positively correlated with the curative effect, and the correlation was statistically significant.
Discussion
The incidence of facial paralysis in children under 15 years old is about 21/100,000/year [11], which idiopathic facial paralysis is the most common, accounting for about 79.9% [1]. Although the overall prognosis of idiopathic facial paralysis is good after treatment [1,12,13], for children, especially young children, due to the low compliance in treatment, it often brings greater difficulties to treatment. This study was conducted on children under 6 years of age. By using the guided training mode in the rehabilitation training of children with facial paralysis, compared with the traditional functional training method, the results show that this method can effectively improve the patient's compliance and the effect of rehabilitation treatment.
The treatment of children with idiopathic facial paralysis is mainly drug and rehabilitation. Steroids combined with antiviral drugs are commonly used drug treatment options, but there are some controversies in the current study [11]. Physical therapy is considered to be an important and effective intervention for facial paralysis, including muscle strength training, biofeedback training, electrical stimulation, and local massage [14]. Among them, exercise training is the most important part of the rehabilitation program. Through proprioceptive stimulation, neuromuscular activation and promotion, and muscle strength training, it can promote facial muscle strength and motor coordination [8,15,16], and achieve natural expression and communication. Aysel's study confirmed the importance of exercise therapy for children with facial paralysis and achieved good results [12]. However, previous studies have mainly focused on older children. Particular attention is paid to the compliance problems of young children. However, this study mainly focuses on young children with insufficient compliance and integrates the guided education model into routine exercise training to demonstrate the positive treatment effect of this method on children with facial paralysis.
Three kinds of physical factors were used in this study. The ultrashort wave of facial features, direct current drug iontophoresis, and intermediate frequency pulse electrotherapy. Ultrashort waves have been confirmed to have the effect of promoting functional recovery after nerve injury [17,18], and there are research reports on promoting functional recovery in patients with facial paralysis [19].The direct current drug iontophoresis directly introduces the drug into the lesion site, maintains a high drug concentration in the affected site, and plays a good role in promoting the recovery of nerves [20].Intermediate frequency electrical therapy can promote muscle recovery, stimulate proprioception, and promote nerve function recovery [21,22]. Ultrashort wave, direct current, and medium frequency electrical stimulation were used as the basic physical therapy methods for treatment, which had a positive effect on patients and improved the effect of exercise therapy.
Guided education is a brand-new system founded by Professor Andras Peto of Hungary. Specifically, it induces target movements in a certain way, emphasizing patient-centeredness. Guided education is superior to other methods in stimulating patients' active participation and comprehensive rehabilitation [5,7]. In this study, the core principles and guiding methods of guided education were applied to the rehabilitation training of children with facial paralysis.
In this study, we innovatively applied the concept of guided education to the exercise treatment of young children with facial paralysis, with the main purpose of increasing children's exercise participation. From the evaluation results of training participation, children's participation has been significantly improved under the guided education model. In the training process, children's fear or resistance to the treatment staff is reduced through game interaction, and children's active participation is stimulated in an entertaining, rhythmic, and intentional manner. Through repeated practice, continuous consolidation, and gradual progress, the children's abilities in all aspects can be gradually improved. From this study, it can be found that the children in the control group were treated with conventional physical therapy, the resistance of the children to the treatment was obvious during the treatment process, and the situation did not improve significantly over time. This study shows that the degree of active participation is positively correlated with the curative effect, and the increase of active participation significantly improves the effect of facial paralysis treatment.
In previous studies on children with facial paralysis, few children under the age of 6 years. In this study, it can be seen that exercise training can significantly improve the recovery effect of children with facial paralysis. Participation is an important factor affecting the training effect. Although the current view is that children with idiopathic peripheral facial paralysis have strong self-healing ability [1,11], this study also indirectly suggests that therapeutic training has a significant effect on promoting children’s functional recovery. The cognition of facial function in patients under 6 years old is not yet comparable to that of older children. The recovery process may be affected by the lack of active participation.
Guided rehabilitation training combined with physical factor therapy can effectively promote the functional recovery of young children with facial paralysis. The guiding education concept and method are integrated into the therapeutic training, which significantly improves the participation of children and the effect of treatment.
There are still deficiencies in this study. The low incidence of facial paralysis in young children, only a retrospective study was used, which affected the strength of the demonstration; on the other hand, there may be differences at the treatment level due to large differences in the number of therapists' years of work, which may affect the results. Subsequent studies with better research designs are needed to further explore the effect of guided training in children with facial paralysis.
References
- Karalok ZS, Taskin BD, Ozturk Z, Gurkas E, Koc TB, et al. (2018) Childhood peripheral facial palsy. Childs Nerv Syst 34: 911-917.
- Kanerva M, Liikanen H, Pitkäranta A (2021) Facial palsy in children: Long-term outcome assessed face-to-face and follow-up revealing high recurrence rate. Eur Arch Oto-Rhino-Laryngol Off J Eur Fed Oto-Rhino-Laryngol Soc EUFOS Affil Ger Soc Oto-Rhino-Laryngol - Head Neck Surg 278: 2081-2091.
- Fu L, Bundy C, Sadiq SA (2011) Psychological distress in people with disfigurement from facial palsy. Eye Lond Engl 25: 1322-1326.
- Bourke-Taylor H, O’Shea R, Gaebler-Spira D (2007) Conductive education: A functional skills program for children with cerebral palsy. Phys Occup Ther Pediatr 27: 45-62.
- Balogh E, Kozma I (2009) Conductive education for children with neurological diseases. Ideggyogyaszati Szle 62: 12-22.
- Thielker J, Kuttenreich A-M, Volk GF, Guntinas-Lichius O (2021) Diagnostics and Therapy of Idiopathic Facial Palsy (Bell’s Palsy). Laryngorhinootologie 100: 1004-1018.
- Bek J, Brown MR, Jutley-Neilson J, Russell NCC, Huber PAJ, et al. (2016) Conductive Education as a Method of Stroke Rehabilitation: A Single Blinded Randomised Controlled Feasibility Study. Stroke Res Treat 2016: 5391598.
- Barbara M, Antonini G, Vestri A, Volpini L, Monini S (2010) Role of Kabat physical rehabilitation in Bell’s palsy: A randomized trial. Acta Otolaryngol (Stockh) 130: 167-172.
- Sun Z, Tian Y, Tan Y, Tao D, Li W, et al. (2020) Effectiveness of Kinesio taping on peripheral facial paralysis. Medicine (Baltimore) 99: e23090.
- VanSwearingen JM, Brach JS (1996) The Facial Disability Index: Reliability and Validity of a Disability Assessment Instrument for Disorders of the Facial Neuromuscular System. Phys Ther 76:1288-1298.
- Jenke AC, Stoek L-M, Zilbauer M, Wirth S, Borusiak P (2011) Facial palsy: Etiology, outcome and management in children. Eur J Paediatr Neurol 15: 209-213.
- Aysel A, Müderris T, Yilmaz F, Tokat T, Aliyeva A, et al. (2020) Pediatric Bell’s palsy: Prognostic factors and treatment outcomes. Turk J Pediatr 62:1021-1027.
- Karatoprak E, Yilmaz S (2019) Prognostic Factors Associated With Recovery in Children With Bell’s Palsy. J Child Neurol 34: 891-896.
- Vaughan A, Gardner D, Miles A, Copley A, Wenke R, et al. (2020) A Systematic Review of Physical Rehabilitation of Facial Palsy. Front Neurol 11: 222.
- Jacqueline Diels H, Ma DC (1997) Neuromuscular Retraining For Facial Paralysis. Otolaryngol Clin North Am 30: 727-743.
- Baba S, Kondo K, Yoshitomi A, Kanemaru A, Nakaya M, et al. (2021) Efficacy of Mirror Biofeedback Rehabilitation on Synkinesis in Acute Stage Facial Palsy in Children. Otol Neurotol Off Publ Am Otol Soc Am Neurotol Soc Eur Acad Otol Neurotol 42: e936-e941.
- Wang N, Feng Z, Zhao W, Zhang Z, Zhang L (2018) Ultrashortwave radiation promotes the recovery of spinal cord injury by inhibiting inflammation via suppression of the MK2/TNF-α pathway. Int J Mol Med 42: 1909-1916.
- Incebiyik S, Boyaci A, Tutoglu A (2015) Short-term effectiveness of short-wave diathermy treatment on pain, clinical symptoms, and hand function in patients with mild or moderate idiopathic carpal tunnel syndrome. J Back Musculoskelet Rehabil 28: 221-228.
- Marotta N, Demeco A, Inzitari M, Caruso M, Ammendolia A (2020) Neuromuscular electrical stimulation and shortwave diathermy in unrecovered Bell palsy: A randomized controlled study. Medicine (Baltimore) 99: e19152.
- Liang H, Li Z, Lin H, Chen J (2018) Effects of methycobal iontophoresis combined with balance acupuncture on peripheral facial paralysis. Zhongguo Zhen Jiu Chin Acupunct Moxibustion 38: 955-960.
- Wang X-J, He N-N, Ji W-B, Yu L, Zhang P (2021) Effect of Penetration Electroacupuncture Combined with Intermediate Frequency Electrotherapy, Facial Acupoint Massage, and Cervical Reduction on Facial Nerve Function and Curative Effect of Senile Refractory Facial Paralysis. J Healthc Eng 2021: 3776006.
- Tuncay F, Borman P, Taser B, Ünlü I, Samim E (2015) Role of Electrical Stimulation Added to Conventional Therapy in Patients with Idiopathic Facial (Bell) Palsy. Am J Phys Med Rehabil 94: 222-228.
Citation: Zhang L, Yang H, Xue J, Hou Y, Ma X, et al. (2023) A Retrospective Study on the Application of Guided Rehabilitation Training In the Rehabilitation of Children with Peripheral Facial Paralysis. J Phys Med Rehabil Disabil 9: 80.
Copyright: © 2023 Liming Zhang, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

