
A Retrospective Study to Determine the Impact of having a Dual Diagnosis for Patients who are on the Opioid Treatment
*Corresponding Author(s):
Hesitha AbeysunderaDepartment Of Alcohol And Other Drug Service, Gold Coast University Hospital, Gold Coast, Queensland, Australia
Email:hesitha.abeysundera@health.qld.gov.au
Abstract
Introduction: Dual Diagnosis (DD) is the condition of suffering from a mental illness and a co-morbid substance use disorder. This presents a challenge in daily clinical practice. DD patients have been found to have more complications and poorer outcomes compared to patients with a single disorder. The aim of the study was to determine the prevalence of co-morbid mental disorders among patients on an Opioid Treatment Program (OTP) and the impact of having DD on employment and incarceration. Comparison was also made between patients with and without DD on their duration of stay on OTP.
Settings: Data was collected from two outpatient OTP clinics at the Alcohol and Other Drug Services (AODS) at the Gold Coast Health and Hospital Service (GCHHS).
Methods: This study was a retrospective chart review of 122 new referrals to AODS at the GCHHS between 01/01/15 to 31/12/2015.
Findings: The prevalence of co-morbid Axis 1 or Axis 11 disorders (DSM-1V TR) was 67.2% among patients on the OTP. 81.1% of OTP patients were unemployed. There was a significant difference between the duration of stay on the OTP for patients with DD and without DD (p<0.025). 89% of patients who disengaged from OTP had DD.
Conclusion: DD is an evolving field as shown by the high prevalence of co-morbid mental disorder among the patients on OTP. DD is associated with poorer outcomes and further research is required in understanding casual relationships and developing effective prevention, treatment and recovery strategies.
Keywords
INTRODUCTION
Dual Diagnosis (DD) is the co-occurrence of mental illness and a substance use disorder. DD is often associated with high rates of continued substance use, greater psychological impairment and increased utilization of services [1,2]. This is now recognised as a major problem of patients receiving care from both mental health and AODS [3]. DD is associated with more severe symptoms, higher relapse rates, higher service use, poorer treatment outcomes and a strong association with violence and suicide [4-8]. Historically, people have found many barriers to accessing both mental health and substance abuse services and may not receive help from either service [9]. In comparison to non-DD patients, DD patients are more prone to complications and are at greater risk of adverse outcomes from poor personal hygiene, medication non-adherence, in addition to their psychiatric symptoms and their limited protective factors. DD patients often need more intense case management due to the complexity of their cases which is impacted on by the severity of their illness and drug use as well as the psychosocial impact of both diagnoses.
Studies of psychiatric co-morbidity in opioid abusers suggest that up to 80% of patients meet the criteria for at least one non-substance use disorder during their lifetime while current figures for psychiatric co-morbidity have been reported in 30%-70% of the patients [10-12]. Depression and antisocial personality disorder are the most common psychiatric diagnoses reported in patients dependent on opioids followed by dysthymia and anxiety disorders [10].
Substance use is common in the general population. The National Drug Strategy Household Survey of 2007 found that, in an Australian sample of 23,356 (of over 14 years old), 44.6% had smoked tobacco, (19.4% in the past 12 months); 89.9% had tried alcohol, (82.9% in the past 12 months); 38.2% had used an illicit drug (13.4% in the past 12 months), 9.1% Cannabis (THC), 3.9% prescription medication, 3.5% ecstasy and 2.3% amphetamines [13]. The prevalence of substance use is higher in people with severe mental health problems, with approximately 50% having had problems relating to their substance use and a quarter to a third having a current problem [14].
There have been many studies showing a much higher incidence of substance misuse in people with psychosis [14]. The Epidemiological Catchment Area (ECA) study found that in patients with schizophrenia, the odds of having an alcohol use disorder were three times higher and another drug use disorder six times higher, than for the general population [15]. The odds were five times higher and eight times higher in patients with bipolar disorder. An Australian study of community patients with schizophrenia showed a lifetime use of any substance of 59.8%, with a 26.8% use in the past 6 months (mainly alcohol and cannabis) [16]. The same ECA study reported that 47% of people with schizophrenia misused substances: (including alcohol -37%, cannabis -23% and stimulants or hallucinogens -13%) [15]. Of those with an affective disorder, 32% had a co-morbid substance use disorder. The lifetime prevalence of alcohol dependence or misuse in those with social anxiety disorder was, 22%, while among the opioid dependent population, lifetime prevalence of anxiety disorders were 6.1% in men and 10.7% in women.
Conversely, mental health problems are common in people involved in substance use. The ECA study found that of people abusing alcohol, 37% had a mental illness [15]. Of these, 12% had a mood disorder and 29% had an anxiety disorder (the most common was post traumatic stress disorder-PTSD at 5.6%). Antisocial personality disorder co-occurred in 14%. Of people with drug disorders, 53% had another mental health problem; 28% anxiety disorder, 26% mood disorder and 18% had antisocial personality disorder.
OBJECTIVES OF THE STUDY
The aim of the study was to determine the prevalence of a co-morbid mental disorder among patients on OTP, and the impact of DD on employment and incarceration. We also looked at the duration of stay and hence the engagement of patients with/without DD on the OTP.
We hypothesized that patients diagnosed with a DD would have a lower employment rate and shorter stay/poor engagement on the OTP.
METHOD
Study population
Study setting/location
Study design
Data analysis
Ethics approval
RESULTS
The main opioid medication that patients were commenced on after registration with the OTP was the compound medication Suboxone TM (buprenorphine and naloxone). GCHHS uses Suboxone TM as first line treatment policy due to its relatively lower rate of diversion. Methadone was commenced on patients who were allergic to Suboxone TM. Buprenorphine alone (Subutex) was commenced on seven patients who were allergic to Suboxone TM and one patient who was pregnant (Table 1).
|
Demographic variables |
N=122 |
|
Age |
8 (6%) |
|
Gender |
74 (60.6%) |
|
Employment |
23 (18.9%) |
|
OTP Medications |
85 (69.6%) |
|
No of Patients |
% Patients |
OTP Stay in Months (Mean) |
P Value |
||
|
DD |
Yes |
88 |
72.1 |
5.3 |
0.007 |
|
No |
40 |
27.9 |
6.5 |
|
Variable |
Number Patients |
% Patients |
OTP Average Month Stay |
DD (n) |
DD (%) |
Chi Square |
P Value p<0.01 |
|
|
Age |
<25 |
9 |
7.4 |
4.1 |
7 |
77.8 |
9.53 |
0.008523 |
|
26-50 |
94 |
77 |
5.6 |
68 |
72.3 |
|||
|
>50 |
19 |
15.6 |
6.7 |
7 |
36.8 |
|||
|
Gender |
Male |
74 |
60.6 |
5.4 |
42 |
56.8 |
4.3859 |
0.3627 |
|
Female |
48 |
39.4 |
6 |
40 |
83.3 |
|||
|
Employment |
Yes |
23 |
18.9 |
5.6 |
8 |
34.8 |
13.5271 |
0.0002 |
|
No |
99 |
81.1 |
5.7 |
74 |
74.7 |
|
Generalised Anxiety Disorder (GAD) |
11 (9%) |
|
Schizophrenia |
10 (8.2%) |
|
Drug Induced Psychosis |
2 (1.8%) |
|
Bipolar Affective disorder |
7 (5.7%) |
|
Major Depressive Disorder (MDD) |
5 (4.1%) |
|
Post Traumatic Stress Disorder |
2 (1.6%) |
|
Post Natal Depression |
1 (0.8%) |
|
Anti-Social Personality Disorder |
11 (9.0%) |
|
Borderline Personality Disorder |
9 (7.4%) |
|
GAD + MDD |
23 (18.9%) |
Stem-and-Leaf Plots
The reasons for patients leaving the OTP provided some understanding of the impact of having a DD (Table 5).
• Twelve patients left the OTP prior to completion due to mental health reasons, either due to relapse, admission or aggression
• Of the patients who did not attend at all the OTP (17/19); 89.4% had a dual diagnosis
|
Reasons Given |
N=122 |
|
Mental health reasons |
12 (9.8%) |
|
Transfer to another service |
14 (11.5%) |
|
Did not attend |
19 (15.6%) |
|
Incarceration |
4 (3.3%) |
|
Completed detox |
7 (5.7%) |
|
Remained registered in OTP |
66 (54.1%) |
|
Total |
122 (100%) |
Table 5: Reasons for patients leaving OTP.
DISCUSSION
Our study showed a higher rate of (67.2%) DD patients on OTP compared to previous studies. Two studies by Brooner et al., reported psychiatric co-morbidity of 37% and 47% respectively among patients on OTP [18,19]. Similarly, Rouser et al., reported that 39% of OTP patients had a co-morbid psychiatric diagnosis [20]. Other studies including Kessler et al., Dake et al., Limbeek et al., reported 50%, 60% and 85% additional psychiatric co-morbidity in their opioid dependent population respectively [11,12,21]. In contrast to other studies Merikan et al., and Musharaf and Rehman et al., reported less than 10% psychiatric co-morbidity in their samples [22,23]. There can be several reasons for these wide variations, including widely different populations studied by different authors, use of different diagnostic criteria and the heterogeneous settings in which the studies were conducted.
Prior studies have shown higher rates of depression among opioid users. Findings of Limbeek et al., [16], Regier et al., and Rounsaville et al., reported a high figure of around 48% with major depression in their samples [24,25]. In our study, the rate of MDD was 4.1% among OTP patients. Although Musharaf and Rehman et al., reported a much lower figure of less than 2% in their study, it has to be noted that the Musharaf and Rehman et al., study was a retrospective study based on case notes which could have inherent problems. These studies indicate that about one third of patients suffering from opioid dependence have additional depressive illness. These findings support the hypothesis of a relatively high prevalence of psychiatric co-morbidity among people dependent upon opioids seeking treatment [11].
The studies done by Brooner et al., Khan M and Rehman A et al., and Regier DA et al., have shown anxiety and psychotic disorders to be less associated with opioid dependence than depressive illness [9,18,23]. However the co-morbidity of schizophrenia and substance abuse has attracted considerable attention in recent years [27] with evidence that the rate is rapidly increasing [24,26]. Fowler et al., reported a higher prevalence of about 26% for overall substance abuse in schizophrenia; however, opioid use has been reported in only 2-9% in this population. Similarly Caniwell et al., showed that 7% of the study population with first episode psychosis met the diagnosis of substance abuse including 8.4% with substance related psychotic disorder [10,27]. Our study showed 9.1% with generalised anxiety disorder, Schizophrenia in 8.2% and drug induced psychosis in 1.8% respectively among the opioid users. Most authors agree that substance abuse and schizophrenia are associated not only with violence but also with a number of other problems including poor treatment adherence , an increased suicide risk, increased rates of hospital admission and Human Immunodeficiency Virus (HIV) infections [24].
Similarly, personality disorder has been a co-morbid diagnosis in excess of 30% in many studies [9,11,19-21]. Dake et al., even reported a figure of 60% in their study [21]. In our study the percentage of ASPD ad BPD were 11.0% and 8% respectively (Table 2).
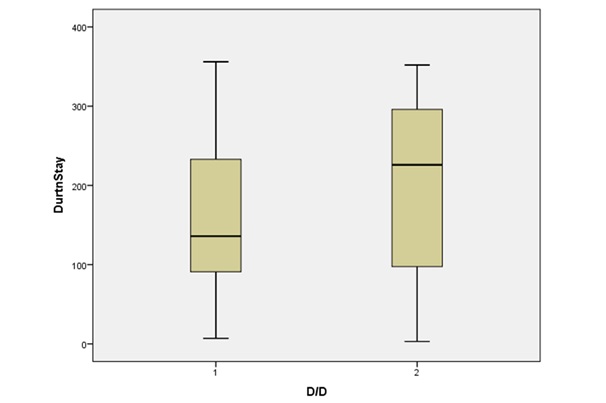
This study highlights the high prevalence of psychiatric co-morbidity in patients with opioid dependence with GAD and ASPD being the highest. As hypothesized our study showed a high unemployment rate 81.1% among the OTP patients but with a low incarceration rate. These results are in keeping with prior similar studies by Griffin et al., which showed an unemployment rate of 62.8% and Bennningfield et al., showed an unemployment rate of 77%. The incarceration rate in Benningfield et al., showed a lower rate of 19.5%. This is possibly due to a different population (American pregnant women). As hypothesized our study showed a shorter duration of stay on the OTP for patients with DD, we were unable to find similar studies comparing duration of stay on OTP with or without DD.
The most common co-morbid mental disorders are major depression and anxiety. Detection and treatment of these conditions has a significant preventative role in the management of opioid dependence. It appears that in clinical practice most of these cases go undetected even in the tertiary care units as was the case in these centres. Appropriate treatment of mood disorders can potentially help to decrease the severity, duration and complications of drug dependence. This suggests the need for psychiatric screening of all patients with opioid dependence who come for detoxification. While the presence a co-morbid mental disorder makes the treatment of drug dependence more difficult, there is also evidence that successful treatment of co-morbid mental disorder improves outcomes in co-morbid substance use disorders, and vice versa [19].
Our study showed that patients aged less than 25 years had a shorter mean duration of stay compared to the patients who were 26 years and older. In less than 25 years age group, larger proportion of patients disengaged from the OTP. This could possibly be due to the fact that younger age group are more likely to disengage due to recurrent illicit substance use. This age group possibly will require several attempts at stabilising on OTP. We could not find other similar studies comparing duration of stay on OTP with DD patients.
LIMITATIONS
There were a number of limitations in this study. This was a retrospective study, with information gathered from chart reviews. Results may be influenced by recall bias, although previous work suggests that informants of illicit substance users underestimate psychiatric and substance use problems [25]. Some patients may not have disclosed having a co-morbid mental disorder at the time of the registration due to stigma or for other reasons. It was assumed that patients with DD who disengaged prior to completion of the OTP were due to a relapse of co-morbid mental disorder or admission to mental health units, as the reason for disengagement was not recorded on the charts.
CONCLUSION
These results show that the presence of a co-morbid mental disorder was associated with poor outcomes in patients enrolled in an OTP, including lower employment, more likely not to attend any sessions and a shorter time to discharge from the OTP. These findings suggest that screening for co-morbid mental disorder at the time of enrolment in the OTP may lead to better outcomes both for mental health and for substance use disorders by targeted treatment of co-morbid conditions.
Detection and treatment of a co-morbid mental disorder has significant preventive role in the management of substance dependence. Therefore, it is necessary for screening all opioid dependent patients for co-morbid mental disorders who come for detoxification is recommended. Timely detection of DD could lead services to link OTP patients to appropriate services (mental health services, dual diagnosis services). It is recommended that training of AODS staff working in the AODS be implemented and screening instruments be used to detect psychiatric co-morbidity.
CONFLICT OF INTEREST
The authors have no conflict of interest to report in conducting this study.
ACKNOWLEDGEMENTS
We wish to thank Greta Ridley and other staff members of the statistical department Griffith University who helped us with this project.
REFERENCES
- Queensland Health (2010) Dual Diagnosis Clinician Tool Kit. Queensland Health, Queensland, Australia.
- Kovasznay B, Fleischer J, Tanenberg-Karant M, Jandorf L, Miller AD, et al. (1997) Substance use disorder and the early course of illness in schizophrenia and affective psychosis. Schizophr Bull 23: 195-201.
- Wade D, Harrigan S, Edwards J, Burgess PM, Whelan G, et al. (2006) Substance misuse in first-episode psychosis: 15-month prospective follow-up study. Br J Psychiatry 189: 229-234.
- Bartels SJ, Teague GB, Drake RE, Clark RE, Bush PW, et al (1993) Substance use in schizophrenia: Service utilization and costs. J Nerv Ment Dis 181: 227-232.
- Department of Health (2002) Mental health policy implementation guide: Dual diagnosis good practice guide. Department of Health, London, UK.
- Graham HL, Copello A, Birchwood MJ, Mueser KT (2007) Substance misuse in psychosis: Approaches to treatment and service delivery. Wiley, Hoboken, New Jersey, USA.
- Todd FC, Sellman JD, Robertson PJ (2002) Barriers to optimal care for patients with coexisting substance use and mental health disorders. Aust N Z J Psychiatry 36: 792-799.
- Tucker P (2009) Substance misuse and early psychosis. Australas Psychiatry 17: 291-294.
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, et al. (1990) Comorbordity of mental disorders with alcohol and other drug abuse: Results from the Epidemiological Catchment Area (ECA) Study. JAMA 264: 2511-2518.
- Fowler IL, Carr VJ, Carter NT, Lewin TJ (1998) Patterns of current and lifetime substance use in schizophrenia. Schizophr Bull 24: 443-455.
- American Psychiatric Association (2000) Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition: DSM-IV-TR®. American Psychiatric Association, Virginia, USA.
- Australian Institute of Health and Welfare (2002) 2001 National drug strategy household survey. Australian Institute of Health and Welfare, Canberra, Australia.
- Rounsaville BJ, Weissman MM, Crits-Christoph K, Wilber C, Kleber H (1982) Diagnosis and symptoms of depression in opiate addicts: Course and relationship to treatment outcome. Arch Gen Psychiatry 39: 151-156.
- Wu LT, Kouzis AC, Leaf PJ (1999) Influence of comorbid alcohol and psychiatric disorders on utilization of mental health services in the National Comorbidity Survey. Am J Psychiatry 8: 1230-1236.
- Robins LN, Helzer JE, Weissman MM, Orvaschel H, Gruenberg E, et al. (1984) Life time prevalence of specific psychiatric disorders in three sites. Arch Gen Psychiatry 41: 949-958.
- von Limbeek J, Wouters L, Kaplan CD, Geerlings PJ, von Alem V (1992) Prevalence of Psychopathology in drug addicted Dutch. J Subst Abuse Treat 9: 43-52.
- Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank RG, et al. (1996) The epidemiology of co-occuring addictive and mental disorders: Implications for prevention and services utilisattion. Am J Orthopsvchiatry 66: 17-31.
- Brooner RK, King VL, Kidorf M, Schmidt CW Jr, Bigelow GE (1997) Psychiatric and substance use comorbidily among treatment seeking opioid abusers. Arch Gen Psychiatry 4: 71-80.
- Brooner RK, Herbst JH, Schmidt CW, Bigelow GE, Costa PT Jr (1993) Antisocial personality disorder among drug abusers. Relations to other personality diagnoses and the five-factor model of personality. J Nerv Ment Dis 181: 313-319.
- Rouser E, Brooner RK. Regier MW, Bigelow GE (1994) Psychiatric distress in antisocial drug abusers: relation to other personality disorders. Drug Alcohol Depend 34: 149-154.
- Dake S, Hall W, Swift W (1994) Prevalence, symptoms and correlates of antisocial personality disorders among methadone maintenance clients. Drug Alchol Depend 34: 253-257.
- Merikangas KR, Risclt N, Weisaman M (1994) Comorbidity and co-transmission of alcoholism, anxiety and depression. Psychol Mcd 24: 69-80.
- Khan M, Rehman AU (1990) Characteristics of heroin addiction in Peshawar. Pilot study. J Postgrad Med 4: 80-86.
- Soyka M (2000) Substance misuse, psychiatric disorders and violent and disturbed behaviour. Br J Psychiatry 176: 345-50.
- Rounsaville BJ, Weissman MM, Kleber H, Wilber C, et al. (1982) Heterogenicity of psychiatric diagnosis in treated opiate addicts. Arch Gen Psychiatry 39: 161-168.
- Boutrose MN, Bowers MR. Quinlan D (1998) Chronological association between increase in drug abuse and psychosis in Connecticut State I-lospilals. J Neuro psychiatr, Clin Neurosci 10: 48-54.
- Cantwell R, Brewin J, Glazebrook C, Dalkin T, Fox R, et al. (1999) Prevalence of substance misuse in first-episode psychosis. Br J Psychiatry 174: 150-153.
Citation: Abeysundera H, Ng B (2018) A Retrospective Study to Determine the Impact of having a Dual Diagnosis for Patients who are on the Opioid Treatment. J Clin Stud Med Case Rep 5: 056.
Copyright: © 2018 Hesitha Abeysundera, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

