
A Standardised Benefit-Risk Matrix Score for Virtual Health Care: A Systematic Review and Proposal for a Numerical Scoring System for Acute and Rehabilitation Services
*Corresponding Author(s):
Vaidya BalaPublic And Population Health, Senior Staff Specialist In Brain Injury Rehabilitation, The Wollongong Hospital, Australia
Email:vaidya.balasubramaniam@health.nsw.gov.au / v_balasubram0418@email.campbell.edu
Abstract
Background: Virtual Health Care (VHC)-including telehealth, remote monitoring, and virtual hospital models-has expanded rapidly, yet a unified Benefit-Risk Matrix (BRM) score to guide implementation across acute and rehabilitation settings is lacking.
Objective: To conduct a systematic literature review on benefit–risk assessment approaches relevant to VHC in Australia and internationally, and to propose a numerical BRM scoring system capturing clinical, operational, equity, safety, and data/privacy domains for both acute and rehabilitation services.
Methods: We searched peer-reviewed and grey literature (2015-Nov 2025) across PubMed/MEDLINE, Embase, PsycInfo, Cochrane Library, Web of Science, and targeted organisational websites (ATA, HHS Telehealth, CADTH, ACP/ORCHA) for studies describing benefit-risk frameworks, matrices, or telehealth evaluation metrics. We followed PRISMA guidance for screening and synthesis and mapped measures to the Quintuple Aim and digital health risk frameworks.
Results: We identified consistent benefit domains (clinical outcomes, access, cost, provider experience, equity) and convergent risk domains (data privacy/security, diagnostic safety, workflow disruption, infrastructure readiness, digital literacy). Evidence supports the use of standardised telehealth evaluation via balanced scorecards and readiness tools. Australian reports highlight the successful scale of virtual hospital/home models and urgent needs for governance, workforce support, and equity safeguards.
Proposed Key Metrics: We present a 10-dimensional BRM with weighted 0-10 sub-scores and a composite Benefit-Risk Ratio (BRR) and Net Benefit-Risk Index (NBRI).
Conclusion: A transparent, reproducible BRM score can enable consistent decisions on VHC adoption across acute and rehabilitation pathways while supporting safety, equity, and sustainability.
Keywords
Acute care; Australia; Benefit-risk assessment; Hospital at home; Rehabilitation; Scoring system; Telehealth; Virtual care
Introduction
Virtual Health Care (VHC) has transitioned from pandemic necessity to a strategic pillar across health systems, including virtual nursing, virtual rounding, remote monitoring, and hospital-at-home models [1,2]. Despite growth, leaders and clinicians often lack a standardised, transparent BRM score to judge when, where, and how VHC should be implemented [3,4].
The need is acute in Australia, where virtual hospitals (e.g., Royal Prince Alfred Virtual Hospital) and virtual urgent care services have demonstrated scale and patient satisfaction, while facing workforce shortages and increased acuity [5]. Internationally, quality frameworks and benefit-risk guidance exist for drugs and devices [6,7], and for digital apps (ACP/ORCHA DHAF), but VHC-specific BRM tools remain fragmented [8,9].
We therefore conducted a systematic review of benefit-risk approaches applicable to VHC and propose a numerical BRM scoring system tailored to acute and rehabilitation services.
Methods
Design
Systematic literature review (SLR) and framework synthesis, followed by proposal of a VHC-specific BRM score.
Search Strategy
With librarian-style methods, we searched MEDLINE/PubMed, Embase, PsycInfo, Cochrane Library, and Web of Science (2015-Nov 2025). Grey literature sources included ATA, HHS Telehealth, ACP/ORCHA DHAF, CADTH, industry reports, and health system white papers [1,8,10,11]. Search terms combined concepts of virtual care/telehealth/virtual hospital with benefit–risk, risk matrix, evaluation, score, quality measures, readiness, and Australia.
Inclusion Criteria
- Empirical studies, reviews, frameworks, or toolkits that assess the benefit and/or risk of VHC (acute or rehabilitation).
- Articles proposing matrices, scorecards, or readiness/risk assessments applicable to VHC.
- Australian and international contexts.
- English language.
Exclusion Criteria
- Purely technical specs without clinical/operational outcomes.
- Non-healthcare benefit-risk tools without clear transferability to VHC.
Screening & Extraction
Two-stage screening (title/abstract → full-text). We extracted domains, measures, scoring approaches, and implementation considerations. We mapped measures to Quintuple Aim (patient experience, provider experience, population health, cost, equity) and digital health risk “toxicities” [12], and classified adoption enablers/barriers using UTAUT themes [13,14].
Results
Evidence Landscape
Across the 2015-2025 literature, the benefits most frequently reported were improvements in access, patient satisfaction, throughput, and readmission reductions, staff experience/retention, and cost savings [4,9,15]. Risks concentrated on data privacy/security, diagnostic safety/clinical quality, technology/infrastructure limitations, workflow disruption, and digital literacy/equity gaps [12,13,16].
Frameworks Informing Structured Assessment Included
- Balanced scorecards adapted for telehealth [3].
- Telehealth readiness assessments [17].
- Quality indicators for VHC in ambulatory settings mapped to Quintuple Aim [9].
- Digital Health Assessment Framework (DHAF) for apps [8].
- Australian virtual hospital/home hospital blueprints and protocols [18,19].
Australian reports and case studies underscore successful scale-up and highlight governance, standardised workflows, and equity safeguards as pivotal for sustainability [5,8].
Synthesis of Core Benefit Domains
- Clinical Effectiveness & Safety (e.g., LOS, readmissions, escalation, adverse events) [5,9].
- Access & Timeliness (e.g., time-to-consult, weekend coverage, rural reach) [2,8].
- Patient Experience (satisfaction, usability, trust) [9,20].
- Provider Experience (burnout, retention, usability) [3,4].
- Cost & Efficiency (per-episode cost, avoided transfers/ED visits) [2,15].
- Equity & Inclusion (digital inclusion, language/cultural appropriateness) [9,13].
Synthesis of Core Risk Domains
- Data Privacy & Cybersecurity (breach risk, compliance gaps) [8,12].
- Diagnostic Safety/Clinical Quality (misdiagnosis risk, remote exam limitations) [10,16].
- Technology & Infrastructure (latency, device integration, reliability) [3,14].
- Workflow & Governance (role clarity, standardised protocols, documentation) [5,8].
- Digital Literacy & Accessibility (patient and staff readiness, language/culture) [13,16].
Proposed Numerical Benefit-Risk Matrix (BRM) Scoring System
Overview
The BRM system provides a transparent, reproducible way to score virtual care deployments across acute and rehabilitation pathways, aligning with Quintuple Aim benefits and the digital risk landscape.
Structure
- 10 Dimensions: 6 Benefits + 5 Risks (note: Equity counted under benefits; see formula weighting).
- Sub-score Scale: 0-10 per dimension (0 = minimal/none; 10 = exceptional/severe).
- Weighting: Clinical safety, diagnostic quality, and data privacy/security receive higher weights to reflect patient safety primacy [6,12].
Dimensions & Suggested Indicators
Benefits
- Clinical Effectiveness & Safety (e.g., reduction in readmissions, adverse events) [4,9].
- Access & Timeliness (coverage hours, rural reach, time-to-consult) [2,8].
- Patient Experience (standardised satisfaction surveys, usability) [9,20].
- Provider Experience (burnout/retention, usability) [3,4].
- Cost & Efficiency (episode cost, avoided transfers/ED) [2,15].
- Equity & Inclusion (language/culture, digital inclusion programs) [9,13].
Risks
- Data Privacy & Cybersecurity (controls, incident history) [8,12].
- Diagnostic Safety/Clinical Quality (risk of misdiagnosis, escalation pathways) [10,16].
- Technology & Infrastructure (uptime, interoperability, latency) [3,14].
- Workflow & Governance (protocols, credentialing, documentation quality) [5,8].
- Digital Literacy & Accessibility (patient/staff training, assistive supports) [13,16].
Acute Services vs Sub-acute Rehabilitation Services
For acute care, emphasise clinical effectiveness, diagnostic safety, and escalation. For rehabilitation, emphasise functional outcomes, continuity, patient engagement, and accessibility [9,18].
Weightings (Example)
- Clinical Effectiveness & Safety (Benefit): w = 1.5
- Data Privacy & Cybersecurity (Risk): w = 1.5
- Diagnostic Safety/Clinical Quality (Risk): w = 1.5
- All other dimensions: w = 1.0
(Local calibration via stakeholder input and sensitivity analyses recommended.)
You may calibrate weights locally using stakeholder input and sensitivity analyses [3,11].
Scoring Formulas
- Composite Benefit Score (CBS):
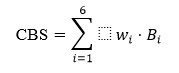
- Composite Risk Score (CRS):
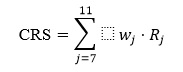
- Benefit–Risk Ratio (BRR): BRR = (CBS/CRS)
- (BRR > 1 = favourable balance; < 1 = unfavourable)
Net Benefit–Risk Index (NBRI): (Positive = supports adoption; negative = defer/mitigate)
Decision Bands (Example)
- Adopt/Scale: BRR ≥ 1.25 and NBRI ≥ +10.
- Pilot with Mitigations: BRR 1.00–1.24 or NBRI +1 to +9
- Defer/Redesign: BRR < 1.00 or NBRI ≤ 0.
These thresholds should be co-designed with clinical, governance, and consumer stakeholders and validated prospectively [8,18].
Implementation Guidance
- Data Sources: EHR analytics, patient/provider surveys, operational logs, incident reports, equity audits [3,9].
- Governance: Establish a BRM committee (clinical safety, digital health, privacy, consumer reps) [5,8].
- Calibration: Conduct sensitivity analyses and benchmark against comparable services [4,11].
- Equity Safeguards: Include language support, digital inclusion, and accessibility features as explicit scoring elements [9,13].
User-Friendly Approach
- Step 1: Add up the good indicators (benefits × weights).
- Step 2: Add up the bad indicators (risks × weights).
- Step 3: Compare them using a ratio and a difference.
- Step 4: Use traffic-light rules (green = adopt, amber = pilot, red = defer).
Hypothetical Example: Virtual Rehabilitation Pilot
Step 1: Score the Benefits
Suppose each dimension is scored out of 20 (higher = better).
- Clinical Effectiveness & Safety = 15 × 1.5 = 22.5
- Access & Timeliness = 12 × 1.0 = 12
- Patient Experience = 14 × 1.0 = 14
- Provider Experience = 10 × 1.0 = 10
- Cost & Efficiency = 13 × 1.0 = 13
- Equity & Inclusion = 12 × 1.0 = 12
Total Benefit Score (CBS) = 83.5
Step 2: Score the Risks
Suppose each risk dimension is also scored out of 20 (higher = more risk).
- Data Privacy & Cybersecurity = 8 × 1.5 = 12
- Diagnostic Safety/Clinical Quality = 9 × 1.5 = 5
- Technology & Infrastructure = 7 × 1.0 = 7
- Workflow & Governance = 6 × 1.0 = 6
- Digital Literacy & Accessibility = 8 × 1.0 = 8
Total Risk Score (CRS) = 46.5
Step 3: Compare Benefits vs Risks
- Benefit–Risk Ratio (BRR):
- Net Benefit–Risk Index (NBRI):
Step 4: Decision Band
- BRR ≥ 1.25
- NBRI ≥ +10
Decision: Adopt/Scale (compelling case for expansion).
User-friendly Recommendations
- The good outweighs the bad by nearly 2 to 1.
- Net benefit is +37 points, well above the adoption threshold.
- This pilot would be recommended for scaling up, with ongoing monitoring of privacy and diagnostic safety risks.
Hypothetical Example: Acute Telehealth Escalation Service
Step 1: Score the Benefits
- Clinical Effectiveness & Safety = 14 × 1.5 = 21
- Access & Timeliness = 15 × 1.0 = 15
- Patient Experience = 10 × 1.0 = 10
- Provider Experience = 9 × 1.0 = 9
- Cost & Efficiency = 11 × 1.0 = 11
- Equity & Inclusion = 8 × 1.0 = 8
Total Benefit Score (CBS) = 74
Step 2: Score the Risks
- Data Privacy & Cybersecurity = 10 × 1.5 = 15
- Diagnostic Safety/Clinical Quality = 13 × 1.5 = 19.5
- Technology & Infrastructure = 9 × 1.0 = 9
- Workflow & Governance = 8 × 1.0 = 8
- Digital Literacy & Accessibility = 7 × 1.0 =7
Total Risk Score (CRS) = 58.5
Step 3: Compare Benefits vs Risks.
- Benefit–Risk Ratio (BRR):
- Net Benefit–Risk Index (NBRI):
Step 4: Decision Band
- BRR ≥ 1.25 (just above threshold)
- NBRI ≥ +10
Decision: Pilot with Mitigations. Although the ratio is favourable, the diagnostic safety risk is high, and patient experience is lower. This suggests the service should proceed cautiously, with strong escalation protocols and governance oversight.
User-Friendly Recommendations
- Acute telehealth shows benefits outweigh risks, but only slightly.
- Net benefit is +15.5, which is positive but not robust.
- Governance should pilot with safeguards (e.g., diagnostic escalation, cybersecurity monitoring, workflow training).
Discussion
Our review consolidates benefit and risk domains relevant to VHC and proposes a numerical BRM score that bridges clinical, technical, and equity considerations. Evidence from Australia demonstrates that virtual hospitals can reduce ED presentations and support high patient satisfaction when workflows are standardised, multidisciplinary teams are engaged, and governance addresses privacy and clinical safety [5,8]. International frameworks reinforce the need for structured benefit–risk assessment, balanced scorecards, and readiness tools to drive adoption [3,17].
Strengths of the proposed BRM include transparency, adaptability to acute/rehab care, and alignment with Quintuple Aim and digital risk frameworks [9,12]. Limitations include heterogeneity of measures across systems, potential subjectivity in scoring, and evolving reimbursement/regulatory contexts. Future work should validate the BRM prospectively across Australian LHDs and international sites, assess inter-rater reliability, and explore patient preference-based weighting, in line with FDA and MDIC approaches [6,7].
Conclusion
A standardised BRM score can support consistent, evidence-informed decisions about virtual care across acute and rehabilitation pathways. By quantifying benefits and risks-especially in clinical safety, privacy, and equity-health systems can scale virtual care responsibly, improving outcomes while mitigating harm.
Acknowledgement
We acknowledge clinicians and consumers across Illawarra Shoalhaven LHD for their ongoing contributions to improving virtual care.
Conflicts of Interest
None declared.
References
- American Telemedicine Association (2025) Scaling virtual care to improve patient safety, reduce burnout, and elevate care delivery.
- Deloitte (2021) Virtual health accelerated: How can health care organizations take advantage of the current momentum?
- Phinney D, Cho A, Ferlotti C, Allen K, Harger J, et al. (2023) Measuring telehealth value and impact using a balanced scorecard approach (Poster). Mid-Atlantic Telehealth Resource Center.
- Caregility (2025) Virtual care KPIs: What should you be measuring?
- McKinsey & Company (2023) Virtual hospitals could offer respite to overwhelmed health systems.
- S. Food & Drug Administration (2023) Benefit-Risk Assessment for New Drug and Biological Products: Guidance for Industry. U.S. Food & Drug Administration, Maryland, USA.
- MDIC (Medical Device Innovation Consortium) (2024) Patient-Centered Benefit-Risk (PCBR) Framework.
- ACP/ATA/ORCHA (2025) About the Digital Health Assessment Framework (DHAF). American College of Physicians.
- Petrie S, Laur C, Rios P, Suarez A, Makanjuola O, et al. (2024) Quality measures of virtual care in ambulatory healthcare environments: A scoping review. BMJ Open 14:
- HHS Telehealth (2025) Best Practice Guides. Telehealth.HHS.gov.
- CADTH (Canadian Agency for Drugs and Technologies in Health) (2022) Approaches to evaluations of virtual care in primary care. Environmental Scan.
- Perakslis ED, Stanley M (2021) Digital health: Understanding the benefit-risk patient-provider framework. Oxford University Press, Oxford, UK.
- Alotaibi N, Wilson CB, Traynor M (2025) Enhancing digital readiness and capability in healthcare: A systematic review of interventions, barriers, and facilitators. BMC Health Services Research 25:
- Oudbier SJ, Souget-Ruff SP, Chen BSJ, Ziesemer KA, Meij HJ, et al. (2024) Implementation barriers and facilitators of remote monitoring, remote consultation, and digital care platforms through the eyes of healthcare professionals: A review of reviews. BMJ Open 14:
- Recuro Health (2025) 30 key metrics when evaluating virtual care savings for 2026.
- Kemp M, Rising KL, Laynor G, Miao J, Worster B, et al. (2025) Barriers to telehealth uptake and use: A scoping review. JAMIA Open 8:
- Pollak AN (2019) Telehealth Readiness Assessment Tool©. Maryland Health Care Commission, Maryland, USA.
- Mathura P, Pascheto I, Dytoc-Fong H, Hrynchyshyn G, McMurtry N, et al. (2024) Advancing a virtual home hospital: A blueprint for development and expansion. BMJ Open Quality 13:
- Harrison R, Mitchell R, Walsan R, Sina M, Clay-Williams R, et al. (2025) Unlocking the promise of virtual care in hospitals: The Smarter Hospitals Project protocol. BMC Health Services Research 25:
- Spectrum Enterprise/HIMSS (2021) Measures of success: Five key metrics for evaluating telehealth services.
Citation: Bala V (2025) A Standardised Benefit-Risk Matrix Score for Virtual Health Care: A Systematic Review and Proposal for a Numerical Scoring System for Acute and Rehabilitation Services. HSOA J Community Med Public Health Care 12: 172.
Copyright: © 2025 Vaidya Bala, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

