Acupuncture Treatment Improves the Swallowing Function and Nutritional Status of the Elderly with Dysphagia : A Randomized Controlled Trial
*Corresponding Author(s):
Zhe ZhaoDepartment Of Geriatrics, Shanghai Sixth People’s Hospital Affiliated To Shanghai Jiaotong University School Of Medicine, Shanghai, China
Tel:+86 2124058456,
Email:sevofurane@163.com
Abstract
Objective: To explore the therapeutic effect of acupuncture on elderly patients with dysphagia.
Methods: A total of 112 elderly patients with dysphagia who were hospitalized in the geriatrics department of our hospital were randomly divided into control group and experiment group, with 56 cases in each group, the control group was given sham acupuncture combined with swallowing rehabilitation training, and the experiment group was treated with acupuncture combined with swallowing rehabilitation training. The changes in the Kubota Drinking Water Test, scores of Standardized Swallowing Assessment (SSA), clinical efficacy, nutritional status, incidence of pulmonary infection, indwelling gastric tube and mortality were compared between the two groups before and after treatment.
Results: There were no significant differences in baseline data such as age, gender, chronic disease, and Kubota Drinking Water Test between the two groups (all P > 0.05). After 3 months of treatment, Kubota Drinking Water Test classifications were improved compared with before treatment, and SSA scores of patients of the two groups were decreased, and Kubota Drinking Water Test classification and the improvements of the above scores in the combination group were significantly better, the differences were all statistically significant (all P < 0. 05). The total effective rate of the experiment group was higher than that of the control group [71.4% (40/56) vs 19.6% (11/56)] (P < 0.05). And the serum albumin, serum prealbumin and hemoglobin levels in the experiment group were higher than those in the control group, and the difference was statistically significant(P < 0.05), the incidence of pulmonary infection was lower than that of the control group [26.8% (15/56) vs 46.4% (26/56), P=0.031], and the rate of indwelling gastric tube was lower than that of the control group [12.5% (7/56) vs 28.6% (16/56), P=0.035]. The mortality rate was lower than in the control group.
Conclusion: The combination of acupuncture and swallowing rehabilitation training can effectively improve the swallowing function of elderly patients with dysphagia, improve their nutritional status, reduce the incidence of lung infections, indwelling gastric tubes, and mortality.
Keywords
Acupuncture; Dysphagia; Nutritional Status; Older People; Randomized Controlled Trial; Swallowing Training
Introduction
Dysphagia is a prevalent and increasingly common problem in the elderly population [1]. Dysphagia affects an individual's ability to safely and effectively eat and drink [2]. Over 13% of the total population 65 years of age and 51% of institutionalized elderly individuals are affected by dysphagia. Additionally, dysphagia affects 16% of independently living individuals aged 70–79 and 33% of the older-than-80 age group with an even higher prevalence among older hospitalized patients [3]. Dysphagia caused by functional impairment of structures such as the mandible, lips, soft palate, pharynx, and esophagus, or due to psychological reasons, which prevents individuals from safely transporting food from the mouth to the stomach. Its clinical features mainly include difficulties in eating and drinking, coughing while drinking water, and speech disorders [4]. Consequences of dysphagia include malnutrition, dehydration, an increased risk of aspiration pneumonia and death from choking [5]. As elderly individuals age, the muscles in their oral and pharyngeal areas gradually degenerate. Moreover, esophageal - related diseases like esophageal cancer and gastroesophageal reflux disease, as well as neurodegenerative diseases or injuries, can lead to the onset of dysphagia [6]. Dysphagia has become one of the common diseases in the elderly. However, due to the non-specific symptoms and communication difficulties of elderly patients, dysphagia is often overlooked, leading to insufficient diagnosis and intervention. Therefore, early diagnosis and treatment of dysphagia are of paramount importance.
Acupuncture is a traditional Chinese medicine therapy that treats swallowing disorders by modulating the nervous system. When specific points such as Hegu and Jiaji are stimulated, neural input to swallowing - related muscles can be adjusted. The technique also promotes local blood circulation, enhancing muscle nutrition and function. Moreover, acupuncture is guided by the meridian theory of traditional Chinese medicine. By stimulating specific acupoints, it aims to regulate the flow of Qi and blood in the meridians connected to the throat and zang - fu organs. This helps to restore the normal function of these areas and improve swallowing ability. Studies have shown that acupuncture can enhance the contraction and relaxation of swallowing - related muscles. It also promotes the release of neurochemical substances in the brain, regulates neural reflexes, and enhances the body's self - repair and regulatory capabilities. This makes acupuncture a safe and effective treatment option for patients with swallowing disorders [7-9].
In elderly individuals, disuse atrophy of swallowing - related muscles is common. Swallowing rehabilitation training is one of the most commonly used methods for treating dysphagia [10]. It can strengthen the movement of the lips, tongue, and chewing muscles, enhance the flexibility of the swallowing reflex, and improve eating and swallowing ability, reducing complications like aspiration pneumonia [11].
Therefore, the purpose of this study is to observe whether acupuncture treatment can improve swallowing function in elderly patients with dysphagia who have been swallowing rehabilitation training, and to observe whether it can improve the nutritional status, occurrence and mortality of aspiration pneumonia in elderly patients.
Methods
- Clinical Data
A total of 112 elderly patients who have dysphagia and were admitted to Shanghai Sixth People’s Hospital Affiliated with Shanghai Jiaotong University School of Medicine between January 2021 and January 2024 were enrolled in this randomized controlled trial. The screening, diagnosis and treatment of dysphagia were accomplished through multidisciplinary collaboration. Each patient was assigned a number based on the order of their arrival. They were then provided information about the study and asked to sign an informed consent form. Non-participants generated random numbers using SPSS 23.0 software. These random numbers and the grouping information were placed in sealed, opaque envelopes. The envelopes were extracted in sequence according to the treatment order. The patients were then divided into an experimental group and a control group at a 1:1 ratio, with 56 patients in each group. To reduce potential bias, the assessors were blinded to the treatment allocation of the participants. There was no difference in age and gender data between the two groups. Each participant was adequately informed of the whole study and gave writing informed consent. Participants will be blinded to their group allocation. To test the patient-blinding effects, all patients will be asked to guess whether they received acupuncture or sham acupuncture. This study was approved by the Medical Ethics Committee of the Shanghai Sixth People's Hospital (No. 2022-KY-157(K)).
The formula for sample size calculation is: N = Z²*σ²/d², where Z represents the confidence interval, n is the sample size, d is the margin of error, and σ represents the standard deviation.
All patients were collected demographic information such as gender, age, and the prevalence of hypertension, diabetes, coronary heart disease, stroke, chronic obstructive pulmonary disease, and neoplasm, etc. Before enrollment, the patients were given venous blood collection, and were evaluated by Complete Blood Count (CBC), biochemistry, chest CT, and cranial nuclear magnetic examination. The patients were evaluated for their swallowing disorders and nutritional status within 48 hours of stabilization.
After 3 months of acupuncture treatment combined with swallowing rehabilitation training, the patients' swallowing disorders and nutritional status were evaluated again, and the occurrence of pneumonia, indwelling gastric tube, and death of the patients during the treatment period were recorded. The flowchart of the trial design is shown in figure 1.
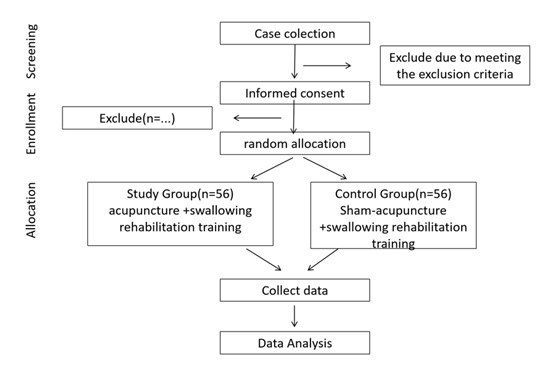 Figure 1: Trial flowchart.
Figure 1: Trial flowchart.
- Inclusion and Exclusion Criteria
Inclusion Criteria: (1) Elderly patients aged 80 years or older. (2) Have difficulty drinking water or eating and are screened as grade III or above using the Pudding Drinking Test. (3) Have normal cognitive function and be able to understand and cooperate with medical staff instructions for completing the assessment and treatment. (4) Voluntarily sign an informed consent form.
Exclusion criteria: (1) Those with serious cognitive impairment or communication disorders. (2) Those with serious, unstable diseases. (3) Patients with swallowing disorders caused by stroke. (4) Those with serious oral, pharyngeal, or cervical spine disorders, or skin breaks or infections at the treatment site.
Dropout criteria: (1) Subjects who have poor compliance during the clinical trial, or are unwilling to continue participating in the study and withdraw voluntarily. (2) Those who experience serious adverse reactions, serious complications, or deterioration during the study are unfit to continue. (3) Subjects who did not follow the treatment protocol or had incomplete observation data that affected the assessment.
- Treatment methods
Swallowing Training: Patients in both groups were treated with standard swallowing training according to the results of the VFSS tests. Functional training was applied to the feeding and swallowing organs (lip, cheek, tongue, soft palate, pharynx, throat, and esophageal sphincter). Standard swallowing training was performed by qualified and experienced nurses.
This oral rehabilitation method focuses on functional recovery of sensory and muscle strength in patients with swallowing dysfunction. Sensory function uses the modified oral care method. First, room temperature saline cotton balls clean the oral cavity. Then, ice saline, warm saline, and acetic acid cotton balls scrub the tongue surface, upper jaw, lower jaw, palatine arches, soft palate, and posterior wall of the pharynx in that order. Each site receives 10 seconds of dwell time, and each site is repeated five times. This process is performed twice daily, in the morning and evening. (b) Recovery of muscle strength refers to performing the following exercises:
Tongue exercises: Tongue extension, tongue topping, and tongue rolling. The purpose of these exercises is to strengthen the tongue muscles.
Oral cavity exercises: The purpose of these exercises is to improve muscle coordination in the various parts of the oral cavity. This includes cheek, open mouth, teeth, knocking, and swallowing movements. Each action is repeated 20 times, and two groups are performed every morning and evening, 60 minutes after meals.
- Acupuncture Treatment
Patients in the experiment group were treated with additional acupuncture after standard swallowing training. The acupuncture needles used in the above procedures were all 0.25 × 40 mm disposable sterile stainless steels needles (Suzhou Medical Appliance Factory Co., Ltd.). The acupuncture operation was performed in accordance with the Reporting Practice for Interventions in Acupuncture Clinical Trial (Standards for Reporting Interventions in Clinical Trials of Acupuncture, STRICTA). Acupoints include bilateral GV26 (Shuigou), and bilateral GB20 (Fengchi), GB12 (Wangu), TE17 (Yifeng), ST9 (Renying), and CV23 (Lianquan) (Table 1). Each acupuncture treatment lasted 20 min, twice a week, and the course of treatment lasted 3 months.
|
Acupoints |
Location |
Sham acupoints |
Location |
|
GV26 (Shuigou) |
On the face, the intersection of the upper 1/3 and the lower 2/3 of the philtrum. |
Sham GV26 |
On the face, under the right nostril, and 0.5 cun (about 15 mm) near the level of the intersection of the upper 1/3 and the lower 2/3 of the philtrum. Avoid ST (stomach meridian of foot-yangming) and CV (conception vessel). |
|
GB20 (Fengchi) |
In the posterior region of the neck, under the occiput, in the depression between the upper part of the sternocleidomastoid muscle and the upper part of the trapezius muscle. |
Sham GB20 |
In the posterior region of the neck, on the outside edge of the trapezius muscle, level with the upper edge of the second cervical spine and the BL10(Tianzhu)point, and 1.5 cun (about 40 mm) beside the posterior midline. Avoid GB (gallbladder meridian of footshaoyang), BL (bladder meridian of foot-taiyang), and the greater occipital nerve. |
|
GB12 (Wangu) |
On the neck, at the posterior and inferior depression of the mastoid process behind the ear. |
Sham GB12 |
On the neck, at the level of the GB12(Wangu)point and 2.25 cun (about 57.5 mm) away from the back midline. Avoid the TE (triple energizer meridian of hand-shaoyang), GB (gallbladder meridian of foot-shaoyang), EX-HN14(Yiming)point, Anmian point, and the lesser occipital nerve. |
|
TE17 (Yifeng) |
On the neck, behind the earlobe, at the anterior and inferior depression of the mastoid process. |
Sham TE17 |
On the sternocleidomastoid muscle of the neck, level with the mandibular angle and the midpoint of the line between TE16 (Tianyou) and SI17(Tianrong). Avoid GB (gallbladder meridian of foot-shaoyang), SI (small intestine meridian of hand-taiyang), and the great auricular nerve. |
|
ST9 (Renying) |
On the neck, level with the laryngeal prominence, at the anterior edge of the sternocleidomastoid muscle and the pulsation of the common carotid artery |
Sham ST9 |
On the neck, at the anterior edge of the sternocleidomastoid muscle and 1cun above the laryngeal prominence. Avoid ST (stomach meridian of foot-yangming) and the transverse nerve of the neck. |
|
CV23 (Lianquan) |
In the anterior region of the neck, on the anterior median line, above the laryngeal prominence, and in the depression of the upper edge of the hyoid bone. |
Sham CV23 |
In the anterior region of the neck, above the laryngeal prominence, and in the depression on the right side of the lower edge of the hyoid bone, 1.0 cun (about 25 mm) is beside the anterior midline. Avoid conception vessel and the transverse nerve of the neck. |
- Sham Acupuncture Treatment
Acupuncture will be performed at 6 non-acupoints. The selection of non-acupoints in control group are the points locating on non-meridians, but near the acupoints we select in experiment group, which is a common method in the design of sham acupuncture [12]. Shallow needling method will be used on these nonacupoints, without making sensation of Deqi. The protocol for choosing the non-acupoints are listed and shown in table 1. The requirements for acupuncturists are the same as for experiment group.
Outcome Measures
Primary outcomes: swallowing function
Swallowing function was assessed before and after treatment in both groups. All post-treatment examinations were completed on the same day after treatment.
- The Standardized Swallowing Assessment (SSA) score was divided into 3 parts, the first part was clinical examination, including pharyngeal reflex, voluntary cough, soft palate movement, laryngeal function, lip closure, consciousness, head and trunk control and respiration, with a value of 8~23 points; the second part was to instruct the patients to swallow 5 mL of water three times, and then to observe the laryngeal function, wheezing, laryngeal movement and repetitive swallowing, with a value of 5~11 points; if there was no abnormality in the above two parts, the patients were instructed to continue to swallow 60 mL of warm water, and then to observe whether there was choking during swallowing and record the time of swallowing, with a value of 5~12 points. If there is no abnormality in the above two parts, instruct the patient to continue to swallow 60 mL of warm water, observe whether there is any choking during swallowing, and record the swallowing time, with a score of 5 to 12. The total score of the scale was 18-46 points, and the stronger the swallowing function, the lower the score [13]. The scale was evaluated by a physician before and after treatment.
- The Kubota drinking test was used to assess swallowing function. Specific method: the patient is asked to take a sitting position or semi-recumbent position, drink 30 mL of warm water, according to the drinking water choking situation and the time used from low to high scoring for 1-5 grades. 1 grade is excellent, can be smooth one time to drink the water down; 2 grades is good, more than two times, cannot choke swallow; 3 grades medium, can be swallowed once, but there are symptoms of choking; 4 grades can be divided into two times more than swallowing, but there are symptoms of choking; 5 grades is poor, frequent choking, and can not be swallowed in full. and unable to swallow all the way down. The rating is normal for grade 1, can be grade 1 within five seconds, grade 2 for more than five seconds, and abnormal for grades 3-5 [14].
- Videofluoroscopic Swallowing Study (VFSS) is the most commonly used method for examining swallowing function and is considered the “gold standard” for detecting and diagnosing swallowing dysfunction. Liquid (30 mL) containing 60% barium sulfate was prepared. The patient was asked to sit down and swallow the liquid, during which the swallowing process was observed using an ICONOS R200 X-ray machine (SIEMENS AG, Germany). The severity of symptoms in the oral phase (0–3 points), throat phase (0–3 points), and aspiration (0–4 points) were evaluated, respectively. VFSS scores ranged from 0 to 10, with a higher score indicating a better swallowing ability. The score of 10 indicated normal swallowing, a score of 7 to 9 indicated a mild abnormality, 4 to 6 points indicated a moderate abnormality, and a score of 0 to 3 points indicated a severe abnormality [15]. Methods of evaluating effectiveness [16]: after treatment, a VFSS score of 10 points indicated a cured condition, an increase in the VFSS score ≥ 2 points and not reaching the normal level was considered to have been excellently effective, and an increase ≥ 1 point and not reaching the normal level was considered effective; no increase or a decrease was considered an effective outcome.
Secondary outcomes
Nutritional status assessment: Venous blood was drawn from both groups before treatment and after 3 months of treatment, and serum albumin (ALB), serum prealbumin (PA), and hemoglobin (Hb) levels were measured using an automatic biochemical analyzer.
Incidence of pneumonia, indwelling gastric tube, and death. Diagnostic criteria for aspiration pneumonia include clinical signs/symptoms of pneumonia in patients with a history or risk factors for aspiration. a complete blood count (CBC) often shows Total number of leukocyte greater than 10,000 or more, with or without leftward shifting of the nucleus of the cells. A chest X-ray typically shows new infiltrates, often in gravity-dependent lung areas. Other indicators are risk factors like impaired consciousness or swallowing dysfunction, and possible foul-smelling breath or frothy sputum. A definitive diagnosis may require tests like videofluoroscopy to confirm aspiration.
Statistical Analysis
SPSS 23.0 software was used for statistical analysis. P value less than 0.05 was considered statistically significant. The Chi-square tests were used to analyze categorical data. Count data were expressed as a percentage (%) and compared among groups using the chi-square (Χ2) test. Normally distributed data were expressed as mean ± standard deviation (x? ± SD). An intergroup comparison was conducted using an independent sample t-test, and an intra-group comparison was conducted among different time points using a paired t-test. Ridit analysis was used to compare the grade information of the two groups.
Results
A comparison of the basic data between the 2 groups
A total of 112 elderly patients with swallowing dysphagia were included in the study. The control group comprised 56 cases, including 45 males and 11 females, aged 80 to 95 years, with an average age of (87.32±4.78) years. The experimental group included 56 cases, 42 males and 14 females, aged 81 to 95 years, with an average age of (88.46±3.72) years. There were no significant differences between the 2 groups in the basic data, such as age, gender, tumor, Coronary Heart Disease (CHD), hypertension, stroke (cerebral apoplexy), Diabetes Mellitus (DM), chronic obstructive pulmonary disease (COPD) (all P > 0.05; Table 2).
|
|
Control group (56 cases) |
Experimental group (56 cases) |
t/χ2 |
P-Value |
|
Age (years, x?±s) |
87.32±4.78 |
88.46±3.72 |
1.413 |
0.160 |
|
Gender [n (%)] |
|
|
0.496 |
0.651 |
|
Male |
45 (80.4) |
42(75.0) |
|
|
|
Female |
11(19.6) |
14(25) |
|
|
|
Tumor [n (%)] |
|
|
0.303 |
0.441 |
|
Y |
11(19.6) |
7(12.5) |
|
|
|
N |
45(80.4) |
49(87.5) |
|
|
|
Coronary Heart Disease [n (%)] |
|
|
0.345 |
0.450 |
|
Y |
25(44.6) |
30(53.6) |
|
|
|
N |
31(55.4) |
26(46.4) |
|
|
|
Hypertension [n (%)] |
|
|
0.280 |
0.419 |
|
Y |
46(82.1) |
50(89.3) |
|
|
|
N |
10(17.9) |
6(10.7) |
|
|
|
Stroke [n (%)] |
|
|
0.508 |
0.742 |
|
Y |
4(7.1) |
6(10.7) |
|
|
|
N |
52(92.9) |
50(89.3) |
|
|
|
Chronic Obstructive Pulmonary Disease (COPD) [n (%)] |
|
|
0.541 |
0.684 |
|
Y |
19(33.9) |
16(28.6) |
|
|
|
N |
37(66.1) |
40(71.4) |
|
|
|
Diabetes Mellitus [n (%)] |
|
|
0.681 |
0.837 |
|
Y |
16(28.6) |
18(32.1) |
|
|
|
N |
40(71.4) |
38(67.9) |
|
|
Table 2: Comparison of basic data between the 2 groups.
Compared with the same group before treatment, *P < .05, **P < .01.
A comparison of the therapeutic effects between the 2 groups
Comparison of Kubota Swallowing Test Grades between 2 groups: After three months of acupuncture treatment combined with swallowing rehabilitation training, the Kubota Swallowing Test grades of patients in the experimental group demonstrated significant improvement compared to those in the control group (P < 0.05; Table 3).
|
|
Grade1 |
Grade2 |
Grade3 |
Grade4 |
Grade5 |
Grade1 |
Grade2 |
Grade3 |
Grade4 |
Grade5 |
|
Before treatment |
After treatment |
|||||||||
|
Control group(56cases) [n (%)] |
0(0) |
0(0) |
22(39.3) |
28(50.0) |
6(11.7) |
0(0) |
0(0) |
21(37.5) |
16(28.6) |
19(33.9) |
|
Experimental group (56 cases)[n (%)] |
0(0) |
0(0) |
27(48.2) |
19(33.9) |
10(17.9) |
0(0) |
14(25) |
16(28.6) |
16(28.6) |
10(17.8) |
|
Z |
-0.362 |
-2.855 |
||||||||
|
P |
0.717 |
0.04* |
||||||||
Table 3: Comparison of Kubota Swallowing Test Grades between 2 groups.
Compared with the same group before treatment, *P < .05, **P
A comparison of the SSA scores between the 2 groups before and after treatment
Before treatment, no significant difference was observed in Swallowing Screening Assessment (SSA) scores between the 2 groups (P > 0.05). Conversely, following treatment, the scores of SSA decreased in both groups, but the scores in the experimental group were lower than those in the control group, and the differences were statistically significant (P < 0.05; Table 4).
|
|
Control group (56 cases) |
Experimental group (56 cases) |
t/χ2 |
P |
|
Before treatment (points) |
34.72 ±5. 28 |
35.41±4. 67 |
0.263 |
0. 837 |
|
After treatment (points) |
33.63 ±5. 32 |
29.34±5.71 |
0.872 |
0.017* |
Table 4: Comparison of SSA scores between the 2 groups before and after treatment.
SSA = Standardized Swallowing Assessment.
Compared with the same group before treatment, *P < .05, **P < .01.
- Comparison of the therapeutic effects between the 2 groups
After treatment, the total effective rate of the experimental group was higher than that of the control group; the effective rates of the 2 groups were 71.4% and 19.6%, respectively (P = 0.006). (P < 0.05; Table 5).
|
Group |
n |
Cure |
Marked Effect |
Effective |
Ineffective |
Total Effective |
|
Control Group |
56 |
0(0.0) |
1(1.8) |
10(17.9) |
45(80.4) |
11(19.6) |
|
Experimental Group |
56 |
6(10.7) |
20(35.7) |
14(25.0) |
16(28.6) |
40(71.4) |
|
Z |
|
-4.516 |
||||
|
P |
0.006** |
|||||
Table 5: Comparison of the therapeutic effects between the 2 groups before and after treatment.
Compared with the same group before treatment, *P < .05, **P <.01.
Comparison of nutritional status indicators between 2 groups
Before treatment, there were no statistically significant differences in serum albumin, serum pre-albumin, and hemoglobin levels between the two groups (P > 0.05). After 3 months of combined diagnosis/treatment and swallowing rehabilitation training, the experimental group had significantly higher levels of serum albumin, serum pre-albumin, and hemoglobin than the control group (P < 0.05; Table 6).
|
|
|
Control group (56 cases) |
Experimental group (56 cases) |
t/χ2 |
P |
|
ALB(g/L) |
Before treatment |
34.49±4.36 |
35.12±2.88 |
1.569 |
0.767 |
|
After treatment |
33.19±2.68 |
37.62±4.13 |
0.732 |
0.042* |
|
|
PA(g/L) |
Before treatment |
238.68±12.63 |
240.05±10.78 |
2.461 |
0.587 |
|
After treatment |
230.24±8.29 |
249.61±9.56 |
0.433 |
0.034* |
|
|
Hb(mg/L) |
Before treatment |
121.61±8.53 |
120.79±6.28 |
0.589 |
0.849 |
|
After treatment |
120.87±9.21 |
132.23±8.73 |
1.032 |
0.043* |
Table 6: Comparison of t nutritional status Indicators between the 2 groups.
Compared with the same group before treatment, *P < .05, **P < .01.
Comparison of pneumonia, indwelling gastric tube, and mortality rates between 2 groups
The experimental group had significantly lower incidence rates of pulmonary infection and indwelling gastric tube placement than the control group (P < 0.05). Although the mortality rate in the experimental group was lower than that in the control group, this difference was not statistically significant. (P > 0.05; Table 7).
|
|
Control group (56 cases) |
Experimental group (56 cases) |
t/χ2 |
P |
|
Incidence of Pneumonia [n (%)] |
|
|
0.018 |
0.029* |
|
Yes |
26(46.4) |
14(25.0) |
|
|
|
No |
30(53.6) |
42(75.0) |
|
|
|
Rate of Indwelling Gastric Tube [n (%)] |
|
|
0.017 |
0.031* |
|
Yes |
16(28.6) |
6 (10.7) |
|
|
|
No |
40(71.4) |
50(89.3) |
|
|
|
Mortality Rate [n (%)] |
|
|
0.496 |
0.325 |
|
Deceased |
14(25.0) |
11(19.6) |
|
|
|
Alive |
42(75.0) |
45(80.4) |
|
|
Table 7: Comparison of Pneumonia, Indwelling Gastric Tube, and Mortality Rates between the 2 groups.
Compared with the same group before treatment, *P < .05, **P < .01.
Discussion
Older adults often experience swallowing difficulties, or dysphagia, a condition that can significantly impact their quality of life. Dysphagia can occur in any of the swallowing phases, including oral, pharyngeal, and esophageal phases. It is estimated that around 20% to 25% of people aged 50 and above experience dysphagia [17]. This condition is more common in older adults and can be caused by various factors such as neurological disorders, muscle weakness, dry mouth, esophageal cancer, etc [18]. Symptoms of dysphagia may include coughing while eating or drinking, difficulty chewing, feeling like food is stuck in the throat, a wet or gurgly-sounding voice during meals, and unexplained weight loss [19]. It can lead to malnutrition in patients, and may also cause dehydration, electrolyte disturbances, and oral inflammation due to food residue [5]. Additionally, food entering the trachea can result in severe complications such as aspiration pneumonia, which can even be life-threatening [20]. The management of dysphagia varies depending on the individual and the underlying cause. Treatments may include behavioral changes, dietary modifications, oral care, swallowing therapy with a speech-language pathologist, medications to manage underlying conditions, and in severe cases, feeding tube placement [21].
Acupuncture is gaining prominence as a therapeutic modality for elderly dysphagia. At present, it has been used both independently and in conjunction with conventional therapies to address swallowing disorders in the elderly [22]. By inserting fine needles into specific acupuncture points that are intricately linked to swallowing function, acupuncture is believed to stimulate the nervous system, enhancing neural reflexes and promoting the release of neurochemical mediators. This can lead to improved muscle tone and coordination in the oral and pharyngeal regions, which are crucial for the swallowing process [23]. Studies have indicated that acupuncture can significantly reduce the severity of dysphagia symptoms, such as coughing and choking during eating, and can improve the efficiency of swallowing [24]. It offers a non-invasive and generally low-risk treatment option, making it particularly suitable for elderly patients who may have multiple comorbidities and be at higher risk for complications from more invasive procedures. Furthermore, acupuncture can be tailored to the individual patient's needs and symptoms, allowing for a more personalized treatment approach [25]. However, it's worth noting that while research into the use of acupuncture for dysphagia is growing, large-scale, randomized controlled trials are still somewhat limited. More rigorous studies are needed to fully elucidate the mechanisms of action and to establish standardized treatment protocols.
Additionally, the integration of acupuncture with other rehabilitation techniques, such as swallowing exercises and dietary modifications, is increasingly being explored to provide a more comprehensive and effective management strategy for elderly patients with dysphagia [26]. The significance of acupuncture in treating elderly dysphagia lies not only in its potential to alleviate symptoms and improve quality of life but also in its contribution to a more holistic and individualized approach to managing this complex condition [27]. Acupuncture stimulates specific points linked to swallowing, enhancing neural reflexes and muscle coordination. Functional training strengthens the oral and pharyngeal muscles through targeted exercises. Together, they improve swallowing function, reduce complications like aspiration pneumonia, and enhance quality of life [28]. This integrated method leverages the benefits of both therapies, offering a more comprehensive and effective solution for elderly patients with swallowing difficulties.
In this study, we treated patients with swallowing disorders in advanced age using acupuncture specific points combined with swallowing rehabilitation training and obtained good results. We used the Kubota drinking test, the SSA score and VFSS to evaluate patients' swallowing function. The Kubota drinking test is a commonly used method for clinically assessing patients with swallowing disorders. It is simple to operate, has clear and distinct grading, and higher grades indicate more severe disorders [29]. The results of this study showed no statistically significant difference in Kubota drinking test ratings between the experiment and control groups before treatment. After treatment, the grade 3 and grade 5 rates were lower in the experiment group than in the control group (28.6% and 17.8%, respectively, versus 37.5% and 33.9%, respectively). There was also an increase in the grade 2 rate in the experiment group after treatment (25%, P < 0.05).
The SSA score, first reported by Ellul et al. in 1996, provides a comprehensive assessment of swallowing function. It ranges from 18 to 46 points, with lower scores indicating better function [30]. Before treatment, the SSA scores of patients in the two groups were compared, and the difference was not statistically significant (P > 0.05). After treatment, however, the SSA scores of patients in the experiment group were lower than those in the control group, and the difference was statistically significant (29.34±5.71 versus 34.72 ±5. 28, P < 0.05).
The VFSS is a dynamic imaging method to evaluate swallowing function. VFSS offers a real-time, dynamic visualization of the entire swallowing process, enabling clinicians to identify abnormalities that might be missed with static imaging. It is relatively safe and non-invasive, requiring minimal patient preparation. The results are highly accurate and reliable, making it the gold standard for swallowing function evaluation. Overall, VFSS is an invaluable tool for healthcare professionals in managing patients with swallowing difficulties [31]. Comparison of efficacy before and after treatment was evaluated using the VFSS: after treatment, the total effective rate of the experiment group was higher than that of the control group (71.4% vs. 19.6%), with P=0.006 (P<0.05) by the nonparametric rank sum test.
The Kubota test, SSA scores and VFSS revealed that acupuncture treatment on the basis of standardized swallowing rehabilitation significantly reduced dysphagia in elderly patients. This is because the Lianquan and Yifeng acupoints selected in our study are specialized in treating dysphagia symptoms [32]. Together with the Fengchi acupoints, they improve cerebral blood flow and promote nerve repair [33]. Local blood circulation, alleviating edema and inflammation is improved in the pharyngeal area, stimulating local nerves (e.g., the hypoglossal nerves) to enhance nerve function, improving muscle flexibility and coordination, and promoting patient rehabilitation. This promotes the patient's recovery. Combined with rehabilitation therapy, acupuncture further promotes the regeneration and repair of damaged nerves and enhances muscle strength and coordination, thus improving swallowing function [34].
Dysphagia often leads to inadequate nutrient intake due to the difficulties in swallowing and eating. This stimulation can enhance the reflex function of nerves and improve the flexibility and coordination of the muscles involved in swallowing [35]. As a result, patients may experience a reduction in symptoms such as coughing and choking during meals, making eating a more comfortable and efficient process. Together, acupuncture and rehabilitation training can lead to a notable improvement in swallowing ability, enabling patients to consume a wider variety of foods and increase their overall food intake [36].
With enhanced swallowing function, patients are better able to meet their nutritional needs, which can help prevent malnutrition, dehydration, and other complications associated with dysphagia. This integrated approach not only alleviates the symptoms of dysphagia but also has a positive impact on the overall nutritional status of elderly patients, thereby improving their quality of life and general well – being [37].This study showed that the nutritional status of patients in the experiment group improved further after treatment. Levels of serum albumin (ALB), serum prealbumin (PA), and hemoglobin (Hb) were higher than in the control group. The incidence of pneumonia and indwelling gastric tubes was lower in the experiment group than in the control group, and the difference was statistically significant (P < 0.05). Although not statistically significant, the incidence of death was lower in the experiment group (19.6%) than in the control group (25.0%). These results suggest that the treatment method combining acupuncture and swallowing rehabilitation training reduces the occurrence of complications, improves prognosis, increases self-care ability, minimizes dependence on others, and reduces mortality.
This study has some limitations. First, the patients were not studied over the medium or long term to determine the effects of this treatment method over time. Second, the sample size needs to be expanded to obtain more reliable results.
Conclusion
In conclusion, the acupuncture can effectively improve swallowing function in elderly patients with dysphagia, alleviate symptoms such as choking while eating or drinking, and reduce the risk of malnutrition, aspiration pneumonia, and other adverse events. This method can also improve quality of life, reduce the burden on families and society, and help maintain the dignity of elderly patients. This method compensates for the limitations of single swallowing function training and is worthy of reference, promotion, and learning.v
Conflict of Interest Statement
All authors of this article declare that they have no conflicts of interest.
Authorship Contribution Statement
Zhe Zhao & Yingying Ke: Conceptualization, Methodology, Software. Zhe Zhao & Yingying Ke: Data curation, Writing- Original draft preparation. Ping Yuan & Wei Chen: Visualization, Investigation. Ping Yuan & Wei Chen: Supervision. Zhe Zhao, Junfeng Zhang & Yingying Ke: Writing- Reviewing and Editing.
Ethical Approval
Ethics approval for this study was obtained from the Medical Ethics Committee of the Shanghai Sixth People's Hospital at Shanghai Sixth People’s Hospital Affiliated to Shanghai Jiaotong University School of Medicine (approval number: 2022-KY-157 (K) ). All participants were provided with information regarding the study and gave their written informed consent prior to participation. This study was conducted in compliance with the Declaration of Helsinki and all applicable ethical guidelines.
Funding Declaration
The authors have not declared a specific grant for this research from any funding agency.
Acknowledgement
We sincerely thank all the collaborating investigators, subjects and their families for their support of the project.
Data Availability
All co-investigators (CIs) will have equal access to the completed dataset, and will collectively decide upon who shall have access to the data and how the data shall be used.
References
- Smukalla SM, Dimitrova I, Feintuch JM, Khan A (2017) Dysphagia in the Elderly. Curr Treat Options Gastroenterol 15: 382-396.
- Adkins C, Takakura W, Spiegel BMR, Lu M, Vera-Llonch M, et al. (2020) Prevalence and Characteristics of Dysphagia Based on a Population-Based Survey. Clin Gastroenterol Hepatol 18: 1970-1979.
- Wirth R, Dziewas R, Beck AM, Clavé P, Hamdy S, et al. (2015) Oropharyngeal dysphagia in older persons - from pathophysiology to adequate intervention: a review and summary of an international expert meeting. Clin Interv Aging 11: 189-208.
- Leira J, Maseda A, Lorenzo-López L, Cibeira N, López-López R, et al. (2023) Dysphagia and its association with other health-related risk factors in institutionalized older people: A systematic review. Arch Gerontol Geriatr 110: 104991.
- Tagliaferri S, Lauretani F, Pelá G, Meschi T, Maggio M (2019) The risk of dysphagia is associated with malnutrition and poor functional outcomes in a large population of outpatient older individuals. Clin Nutr 38: 2684-2689.
- Abu-Ghanem S, Chen S, Amin MR (2020) Oropharyngeal Dysphagia in the Elderly: Evaluation and Prevalence. Current Otorhinolaryngology Reports 8: 34-42.
- Xue C, Jiang C, Zhu Y, Liu X, Zhong D, et al. (2022) Effectiveness and safety of acupuncture for post-stroke spasticity: A systematic review and meta-analysis. Front Neurol 13: 942597.
- Yao L, Ye Q, Liu Y, Yao S, Yuan S, et al. (2023) Electroacupuncture improves swallowing function in a post-stroke dysphagia mouse model by activating the motor cortex inputs to the nucleus tractus solitarii through the parabrachial nuclei. Nat Commun 14: 810.
- Bai L, Cheng H, Hu P, Wang Q, Shilin Z, et al. (2024) Effect of acupuncture on post-stroke dysphagia: a randomized controlled trial. Front Neurol 15: 1391226.
- Huckabee ML, Flynn R, Mills M (2023) Expanding Rehabilitation Options for Dysphagia: Skill-Based Swallowing Training. Dysphagia 2023 38: 756-767.
- Vishak MS, Ramasamy K (2024) Swallowing Rehabilitation: Tracing the Evolution of Assessment and Intervention Approaches for Dysphagia over 30 Years. Indian J Otolaryngol Head Neck Surg 76: 2171-2175.
- Du Y, Zhang L, Liu W, Rao C, Li B, et al. (2020) Effect of acupuncture treatment on post-stroke cognitive impairment: A randomized controlled trial. Medicine (Baltimore) 99: 23803.
- Güleç A, Albayrak I, Erdur Ö, Öztürk K, Levendoglu F (2021) Effect of swallowing rehabilitation using traditional therapy, kinesiology taping and neuromuscular electrical stimulation on dysphagia in post-stroke patients: A randomized clinical trial. Clin Neurol Neurosurg 211: 107020.
- Huang S, Liu Y, Li M, Liu Z, Zhao F, et al. (2022) Oral health knowledge, attitudes, and practices and oral health-related quality of life among stroke inpatients: a cross-sectional study. BMC Oral Health 22: 410.
- Martin-Harris B, Jones B (2008) The videofluorographic swallowing study. Phys Med Rehabil Clin N Am 19: 769-785.
- Tippett DC (2011) Clinical challenges in the evaluation and treatment of individuals with poststroke dysphagia. Top Stroke Rehabil 18: 120-133.
- Su B, Li D, Xie J, Wang Y, Wu X, et al. (2023) Chronic Disease in China: Geographic and Socioeconomic Determinants Among Persons Aged 60 and Older. J Am Med Dir Assoc 24: 206-212.
- Seene T, Kaasik P (2012) Muscle weakness in the elderly: Role of sarcopenia, dynapenia, and possibilities for rehabilitation. European Review of Aging and Physical Activity 9: 109-117.
- Smith Hammond C (2008) Cough and aspiration of food and liquids due to oral pharyngeal Dysphagia. Lung 186: 35-40.
- Liu X, Feng Y, Li R, Zhang H, Ren F, et al. (2025) Comprehensive review of dysphagia and technological advances in dysphagia food. Food Res Int 199: 115354.
- Speyer R, Baijens L, Heijnen M, Zwijnenberg I (2010) Effects of therapy in oropharyngeal dysphagia by speech and language therapists: a systematic review. Dysphagia 25: 40-65.
- Liu X, Chen F, Chu J, Bao Y (2018) Effects of nape acupuncture combined with swallowing rehabilitation on dysphagia in pseudobulbar palsy. J Tradit Chin Med 38: 117-124.
- Cui J, Song W, Jin Y, Xu H, Fan K, et al. (2021) Research Progress on the Mechanism of the Acupuncture Regulating Neuro-Endocrine-Immune Network System. Vet Sci 8: 149.
- Guo H, Pan X, Zheng Y, Yang X, Xu H, et al. (2024) Current state of research on acupuncture for the treatment of post-stroke dysphagia: a scoping review. Front Neurosci 18: 1391576.
- Birch S (2019) Treating the patient not the symptoms: Acupuncture to improve overall health - Evidence, acceptance and strategies. Integr Med Res 8: 33-41.
- Wang J, Wu B, Tong Y, Wang X, Lu Z (2024) Effect of acupuncture combined with rehabilitation training on sensory impairment of patients with stroke: a network meta-analysis. BMC Complement Med Ther 24: 102.
- Wang P, Ma X, Huang J, Li J, Ma L, et al. (2022) Effect of acupuncture treatment on dysphagia caused by pseudobulbar paralysis after stroke: a systematic review and meta-analysis. Ann Palliat Med 11: 2257-2264.
- Wie HS, Kim SN (2025) Therapeutic components of acupuncture stimulation based on characteristics of sensory nerve and nervous signaling pathway. J Integr Med 23: 106-112.
- Suiter DM, Leder SB (2008) Clinical utility of the 3-ounce water swallow test. Dysphagia 23: 244-250.
- Ye J, Pan Y, Zhou T, Liu F, Wei Y, et al. (2024) Evaluating dysphagia in Alzheimer's disease: the significance of age and medical comorbidities,a cross-sectional study from a tertiary psychiatric hospital in Guangzhou China. Front Psychiatry 15: 1482951.
- Boaden E, Nightingale J, Bradbury C, Hives L, Georgiou R (2020) Clinical practice guidelines for videofluoroscopic swallowing studies: A systematic review. Radiography (Lond) 26: 154-162.
- Qin L, Zhang XP, Yang XC, Cui CH, Shi J, et al. (2019) Deep acupuncture of Lianquan (CV23) and Yifeng (TE17) in combination with conventional acupuncture of other acupoints is superior to swallowing rehabilitation training in improving post-stroke dysphagia in apoplexy patients. Zhen Ci Yan Jiu 44: 144-147.
- Guo J, Wang G, Liu T, Zhang J, Li Q, et al. (2025) Acupuncture Improves Chronic Cerebral Ischemia by Inhibiting the CKLF1/HIF-1α/VEGF/Notch1 Signaling Pathway. CNS Neurosci Ther 31: 70246.
- Zhuo P, Huang L, Lin M, Chen J, Dai Y, et al. (2023) Efficacy and safety of acupuncture combined with rehabilitation training for poststroke cognitive impairment: A systematic review and meta-analysis. J Stroke Cerebrovasc Dis 32: 107231.
- Wang X, Wang J, Han R, Yu C, Shen F (2024) Neural circuit mechanisms of acupuncture effect: where are we now? Front Neurol 15: 1399925.
- Ito H, Yamada O, Kira Y, Tanaka T, Matsuoka R (2015) The effects of auricular acupuncture on weight reduction and feeding-related cytokines: a pilot study. BMJ Open Gastroenterol 2: 000013.
- Chen Y, A S, Liu C, Zhang T, Yang J, et al. (2024) A Randomized Controlled Trial Assessing the Impact of Transcutaneous Electrical Acupoint Stimulation on Gastrointestinal Motility, Nutritional Status, and Immune Function in Patients Following Cerebrovascular Accident Surgery. J Invest Surg 37: 2434093.
Citation: Ke Y, Zhang J, Yuan P, Chen W, Zhao Z (2025) Acupuncture Treatment Improves the Swallowing Function and Nutritional Status of the Elderly with Dysphagia: A Randomized Controlled Trial. HSOA J Altern Complement Integr Med 11: 616.
Copyright: © 2025 Yingying Ke, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.