
Acute Coronary Syndrome (ACS), a Special Case Report
*Corresponding Author(s):
Shi-Bo ZhaoCollege Of Clinical Medicine, Youjiang Medical University For Nationalities, Baise, China
Email:760547867@QQ.com
Summary
The main point of investigation in this case was the painful suffocating sensation at an atypical site, which has not been reported in the literature and can be considered as a special case of ACS and a direction for further research. ACS is very common in clinical practice and this case is reported as a special case with the aim of providing ideas and references for clinical management.‘
Acute Coronary Syndrome (ACS) is a group of clinical syndromes caused by acute ischemia of the myocardium, including Unstable Angina (UA), non-ST-segment elevation myocardial infarction (NSTEMI) and ST-segment Elevation Myocardial Infarction (STEMI). The disease is based on the presence of lesions in the coronary arteries. The basis of the disease is the rupture or erosion of atherosclerotic plaques located in the coronary arteries, which leads to the aggregation of platelets in the coronary arteries as acute thrombi, exacerbating the reduction of oxygen flow and severe ischaemia in the myocardium that depends on the coronary arteries for oxygen supply, leading to acute and severe illnesses such as arrhythmia, heart failure and myocardial infarction, which can be life-threatening in severe cases. It can be classified into three categories according to the clinical manifestations, that is, resting angina (variant angina), primary angina and worsening angina.
Case Information
The patient was a 65-year-old male who was admitted to hospital with "episodes of right posterior lumbar back pain for more than 8 hours". On March 10, 2022, after having lunch at 12 noon, the patient felt a sudden pain in the right posterior lumbar back with a suffocating sensation lasting about 10 minutes, which was relieved by rest, without radiating pain, sweating, palpitations, shortness of breath, dizziness and headache, nausea and vomiting. 2 hours later, the above symptoms reappeared without any obvious cause, and the pain was significantly worse than before, lasting for about 20 minutes with excessive sweating. After 2 to 3 minutes, the pain was significantly reduced, but the symptoms were not completely relieved. He was admitted to our department with "acute coronary syndrome". He had a history of hypertension for 15 years, type 2 diabetes mellitus for 10 months, appendectomy in 2021, smoked for 40 years, 1 pack per day, and occasionally drank alcohol. On examination: body temperature: 36.5°C; heart rate: 92 beats/min; respiratory rate: 20 breaths/min; blood pressure: 132/87 mmHg. There was no enlargement of the heart borders, the heart rate was 92 beats/min, the heart rate was in rhythm, no pathological murmur was heard in the valves, no edema in both lower limbs, physiological reflexes were present, and pathological reflexes were not elicited. On admission, he was given aspirin enteric solution 100mg Qd Po, poliovir 75mg Qd Po, low molecular heparin sodium 6400IU Bid Ih triple antithrombotic, atorvastatin calcium tablets 20mg Qd Po for lipid lowering and plaque stabilization, bisoprolol 2.5mg Qd Po to reduce myocardial oxygen consumption, nicorandil 5mg Tid Po, isosorbide nitrate for coronary expansion to improve circulation. Blood, urine and stool, liver and kidney function, coagulation and fibrinolytic indexes, and lipids were generally normal. Cardiac ultrasound suggested a small amount of tricuspid regurgitation; left ventricular hypo-diastolic function (EF: 63%), chest CT suggested thyroid lesion; atherosclerosis; bilateral pulmonary emphysema; multiple small nodules and foci of calcification in both lungs; and multiple cysts in the liver. After ruling out contraindications, a coronary angiogram was performed on March 14, 2022. It was found intraoperatively that: the right dominant coronary artery was distributed; the left main coronary artery (LM) was normal; the proximal middle segment of the left anterior descending (LAD) artery had an unsmooth intima with a 20 mm myocardial bridge and 30% systolic stenosis; the proximal segment of the left circumflex artery (LCX) had plaque; and the right coronary artery (RCA) was normal. Diagnostic imaging: 1. coronary atherosclerosis; 2. left anterior descending artery myocardial bridging (LAD); 3. right dominant type of coronary distribution, returned to the ward after the procedure.
Discussion
Basic information of acute coronary syndrome
Clinical manifestation: Episodic chest pain is the main clinical manifestation. The pain has the following characteristics: 1. It is often induced by physical exertion or emotional excitement. 2. The pain is mainly located behind the body of the sternum and may spread to the precordial region, is about the size of the palm of the hand, which may run through the anterior chest with unclear boundaries, and may be reflected to the left shoulder, left arm, or the neck, pharynx or jaw. 3. The nature of the pain is often pressure, tightness or constriction, with or without chest pain. 4. The pain is more severe, longer lasting, more frequent and can occur at rest than instable angina. 5. General rest or sublingual nitroglycerin can only temporarily or even completely relieve the symptoms. 6. The attack may be accompanied by new symptoms such as sweating, nausea, vomiting, palpitations or dyspnoea.
On physical examination, a transient systolic murmur due to mitral regurgitation may be heard. The ECG may show transient ST-segment elevation or depression and T-wave hypoplasia and inversion.
Diagnostic criteria for ACS: There are three types of ACS as follows, STEMI, NSTEMI and UA, and the diagnostic criteria for each of these three types are described by the 2019 Acute Coronary Syndrome Emergency Rapid Care Guidelines [1] as follows.
STEMI Essential diagnostic criteria: cardiac troponin (cTn) or creatine kinase isozyme-MB (CK-MB) >99th upper Limit of Normal Reference value (ULN) and ECG manifesting as an upward elevation of the ST segment arch. One or more of the following: persistent ischaemic chest pain; abnormal segmental ventricular wall activity on echocardiography; abnormal coronary angiogram.
NSTEMI Essential diagnostic criteria: cardiac Troponin (cTn) or creatine kinase isozyme-MB (CK-MB) >99th upper limit of normal reference value (ULN). In combination with one or more of the following: persistent ischaemic chest pain; electrocardiogram showing new ST-segment depression or T-wave hypoplasia or inversion; echocardiogram showing segmental ventricular wall activity abnormalities; coronary angiography abnormalities.
UA cTn negative, ischaemic chest pain, ECG showing transient ST-segment depression or T-wave depression, inversion, rare ST-segment elevation (vasospastic angina)
Staging of UA [2]: (i) primary angina: new onset of angina within 2 months, manifesting as spontaneous episodes withexertional episodes; (ii) worsening exertional angina: previous history of angina, frequent and prolonged episodes within the last 2 months, with a decreased pain threshold; (iii) resting angina: episodes of angina at rest, usually lasting more than 20 minutes.
Analysis of the characteristics of this case
The patient is an elderly male who was admitted to hospital with "episodic right posterior lumbar back pain for more than 8 hours". In just one day, two episodes of angina-like symptoms occurred with suffocating pain. The second episode was worse than the first and lasted longer with sweating symptoms, and the pain was relieved by taking "quick-acting heart pills". No abnormalities were found in myocardial injury markers and myocardial triadsigns, and no ST-segment changes were seen in the ECG.
UA at atypical sites: In general, the pain site of UA is located in the upper or middle part of the sternal body, which may spread to the precordial region and radiate to the left shoulder, the medial side of the left upper limb and the end of the fingers.
Coronary artery spasm: Coronary angiography in this patient suggests coronary atherosclerosis. It is now believed that sustained spasm in the coronary arteries causes interruption of blood flow and damage to the coronary intima, increased thromboxane A2 and decreased prostacyclin I2, leading to platelet adhesion and aggregation, further increasing vasospasm and forming a vicious circle [3]. If the unstable plaque leads to coronary spasm, causing transient myocardial ischemia and hypoxia, the neural reflexes of the heart may radiate to the back, which may cause the first painful sensation of suffocation in the lower back in this case, mostly seen in myocardial ischemia of the inferior or posterior wall, but the ECG failed to suggest the above ischemia because the patient had no corresponding symptoms at the time of consultation.
Coronary microangiopathy: Under physiological conditions, adaptive processes during the movement of intracoronary blood flow are typically characterized by slight or even no changes in coronary arterial oxygen partial pressure, achieved by feed-forward regulation of coronary blood flow [4]. The mechanisms of coronary microangiopathy are classified as functional abnormalities, structural abnormalities, and due to extra vascular factors [5]. Among the pathogenesis of functional abnormalities, when the microvascular constriction occurs, vasoactive substances can selectively act on the microvasculature, causing diffuse stenosis and myocardial ischemia, which can lead to angina pectoris.
Myocardial bridge: In Japan, a case of acute coronary syndrome in a 28-year-old male patient without any risk factors for coronary atherosclerosis was reported and analyzed as possibly due to a myocardial bridge that accelerated proximal plaque formation [6]. Therefore, there is a relationship between the occurrence of x cardiovascular adverse events and myocardial bridges, which greatly increase the chances of their transformation into vulnerable plaques by causing progressive changes in the microstructure of atherosclerotic lesions in the coronary arteries. Once ruptured, it is highly susceptible to adverse cardiac events such as acute myocardial infarction.
Relevant differential diagnosis: This patient was admitted to the emergency room with "pain in the right posterior lumbar back for more than 8 hours". The pain was suffocating in nature and was relieved by oral administration of "quick-acting heart pills". In a study on the clinical value of the combination of cardiac enzyme profile, troponin, myoglobin and natriuretic peptide in the early diagnosis of acute myocardial infarction, Li Juntao [7] found that the combination of cardiac enzyme profile + BNP + MYO + cTn was more effective than the combination of cardiac enzyme profile, troponin, myoglobin and natriuretic peptide alone and in different combinations. The diagnosis of myocardial infarction can be basically ruled out. The patient has been examined for myocardial triad, markers of myocardial injury and ECG, and no abnormalities were found.
Risk factor inventory: The risk factors in this case included age, gender, hypertension, diabetes mellitus and smoking history. As Atherosclerosis (AS) is a major contributor to ACS, it has been found to be less common in women than in men due to the presence of oestrogen in the body that counteracts the effects of AS [8], AS is particularly common in middle-aged and older men over 40 years of age. In the Chinese expert consensus on the prevention and treatment of hypertension combined with atherosclerosis [9], it is stated that in a state of elevated blood pressure, the pressure of blood on the vessel wall increases, causing mechanical damage and abnormal function of the vascular endothelium. Patients with hypertension often suffer from disorders of lipid metabolism, and elevated levels of total plasma cholesterol and triacylglycerol, which are easily deposited in the damaged endothelium, ultimately leading to atherosclerosis. In addition, vascular endothelial injury is followed by increased expression of adhesion factors, which can also trigger a vascular inflammatory response. Meanwhile, an imbalance in the secretion of vasodilator factors (such as nitric oxide and prostaglandin E1) and vasoconstrictor factors (such as endothelin and angiotensin II) leads to vasodilator dysfunction, which further promotes the development of AS, forming a vicious circle. Yang Shuo [10] found that cigarette smoke leads to impaired vasodilatory function and vascular dysfunction through the release of free radicals and Reactive Oxygen Species (ROS), which cause a decrease in nitric oxide production by endothelial-type Nitric Oxide Synthase (eNOS). eNOS uncoupling leads to the proliferation of Vascular Smooth Muscle Cells (VSMC), matrix eNOS uncoupling leads to proliferation of VSMCs, the release of matrix Metalloproteinases (MMPs) and the initiation of the atherosclerotic process. Nicotine contained in cigarettes stimulates the release of catecholamines and causes both platelet aggregation and thrombosis. Nicotine increases VSMC proliferation by stimulating the release of Fibroblast Growth Factor (FGF), leading to neointimal formation and plaque angiogenesis, and cigarette smoke promotes thrombosis by causing an imbalance between coagulants and anticoagulants. Cigarette smoke promotes thrombosis by causing an imbalance between coagulants and anticoagulants. Smoking induces endothelial dysfunction and oxidative damage to cardiomyocytes, leading to increased risk of vascular injury and thrombosis. Wei Biyue [11] found that increased blood viscosity in diabetic patients leads to tissue ischaemia and hypoxia, generates more oxygen radicals, and further decreases endothelium-dependent vasodilatory effect by reducing NO synthesis and attenuating its bioactivity. It also inactivates two key anti-atherogenic enzymes and prostacyclin synthase, inducing VSMC proliferation and migration, further leading to plaque instability and rupture, while by reducing the synthesis of prostaglandins and others can weaken the vasodilatory effect and accelerate AS.
Detailed analysis of the efficacy of Quick-acting Heart Pill: The main active ingredients of this medicine are ice chips and Chuanxiong Ligustici, which are warm in nature and have the effects of dispelling wind and relieving pain, activating blood circulation and resolving blood stasis; ice chips are bitter in nature and can dispel blood stasis, resolve phlegm and open up the orifices. Modern pharmacological studies have shown [12] that Chuanxiong can inhibit the body's production of oxidized Low-Density Lipoprotein (ox-LDL), reduce the uptake of ox-LDL by macrophages and block the formation of foam cells, thus acting as an anti-inflammatory, antioxidant and free radical scavenger. This patient was admitted to the hospital mainly because of right-sided low back pain. The active ingredient in the quick-acting heart pill, ice chips, can effectively dilate the coronary arteries and improve the blood circulation of the myocardium, which can laterally suggest the presence of relevant stenosis in the coronary arteries.
Differential diagnosis and gold standard "coronary angiography": The patient was admitted with "episodic right posterior lumbar back pain for more than 8 hours", and if the diagnosis of unstable angina pectoris is considered, the differential diagnosis with other related possible diseases is required. The patient's medical history was followed up with a history of multiple polyps in the gallbladder at the age of 20. The patient was admitted to the hospital with a urine routine suggestive of glucose 4+, which could not be explained by the primary pain. At present, the differential diagnosis is ruled out and only the association with coronary atherosclerosis is still being considered. Angiographic diagnosis: 1. coronary atherosclerosis; 2. left anterior descending artery myocardial bridging (LAD); 3. right dominant coronary artery distribution. The angiographic findings confirmed the presence of coronary atherosclerosis, but did not meet the criteria for coronary artery disease (stenosis must be >50%) or for coronary artery bypass grafting, but still considered the presence of myocardial ischaemia. The first symptom of "right posterior lumbar back pain" is considered to be related to coronary atherosclerosis and its risk factors, hypertension and diabetes mellitus (Figures 1-3).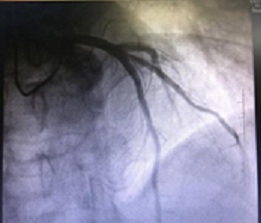
Figure 1: Coronary angiography.
 Figure 2: Episodic right posterior lumbar back pain for more than 8 hours.
Figure 2: Episodic right posterior lumbar back pain for more than 8 hours.
 Figure 3: Right posterior lumbar back pain.
Figure 3: Right posterior lumbar back pain.
Prognosis: Atherosclerotic plaque rupture leading to platelet aggregation and thereby thrombus formation is the main pathogenic basis for myocardial ischaemia in ACS patients, so aspirin combined with clopidogrel is commonly used clinically to inhibit platelet aggregation. Clopidogrel is a P2Y12 receptor antagonist that inhibits the binding of endogenous ADP to platelet receptors, preventing phase 1 coagulation, and the combination of the two greatly improves the survival prognosis of patients with ACS; in addition, clinical treatment of unstable angina is still mainly based on pharmacological control, with statins being the main treatment for this disease [13]. Atorvastatin acts by inhibiting the biosynthesis of endogenous cholesterol, which can reduce lipoprotein levels. Jacobs D [14] found that it has other multifaceted effects, inhibiting the inflammatory response within atheromatous plaques, acting as a plaque stabilizer, and also altering the endothelial function of blood vessels and reducing the occurrence of unstable angina. Yang Bin [15] found in a study on the effects of different doses of atorvastatin on the relevant indexes of patients with unstable angina that the use of higher doses of atorvastatin in the short term could effectively exert anti-inflammatory effects. There was no statistically difference between the adverse reaction rate of the high-dose response group and the low-dose group, confirming that the use of relatively high doses of atorvastatin in a short period of time is more advantageous for the treatment of the disease, which can improve patients' various indicators and improve the long-term prognosis of UA patients.
Treatment options: Primary prevention of coronary heart disease: Coronary angiography suggests coronary atherosclerosis, atorvastatin can be routinely given to lower lipid and stabilize plaque, while patients have a myocardial bridge. β-blockers are often considered the first-line treatment for symptomatic patients [16]. They can relieve myocardial oxygen consumption, increase diastolic coronary filling time, reduce myocardial contractility and coronary artery pressure, and bring coronary flow reserve in the myocardial bridge to normal levels. Calcium channel blockers may provide additional benefit by reducing the concomitant vasospasm in patients with severe myocardial bridges [3], as well as by controlling risk factors, smoking cessation, blood pressure and blood glucose control.
Traditional medicine: The patient's current symptoms are atypical, with no significant abnormalities in any of the indicators. Traditional medicine can be used in a variety of ways to reduce myocardial damage caused by acute coronary syndrome, significantly improve cardiac function, alleviate the patient's symptoms and improve the patient's quality of life. In addition, traditional medicine has significant preventive effects, and their application can greatly reduce the incidence of coronary syndromes, such as Tongxinluo capsule, Thromboxone capsule, Muscadine Heart Protective Pill, Ginkgo biloba drip pill and other Chinese patent medicines. Self-prepared formulas such as Yi Qi and Blood Invigorating Tang, Qishen Tong Yu Tang and Dan Shen Injection are used to activate blood circulation, remove blood stasis, regulate Qi and relieve pain, delay coronary artery sclerosis, improve patients' clinical symptoms and improve long-term prognosis.
Acupuncture: Acupuncture has the effect of regulating qi and blood and unblocking meridians, and its advantages of simple operation, economy and convenience have been widely used in clinical practice, and its efficacy in the treatment of heart diseases has been verified by evidence-based medicine [17-19]. Patients with acute coronary syndrome have been found that acupuncture-assisted treatment could effectively regulate lipid metabolism and reduce depression in patients with ACS, all of which could improve the prognosis of patients with ACS.
References
- Chinese Journal of Emergency Medicine (2019) Guidelines for rapid diagnosis and treatment of acute coronary syndrome. Chinese Journal of Emergency Medicine 2019: 421-428.
- Miao YJ, Yin RH Tang XQ (2020) Diagnostic Study of Coronary Artery Lesions in Patients with Unstable Angina Pectoris By MDCT and Coronary Arteriography. Chinese Journal of CT and MRI 18: 70-72.
- Wu H, Yuan MY (2021) Research status of coronary myocardial bridge with myocardial infarction. Chinese Journal of Medicine 56: 257-260.
- Murray KJ (1990) Cyclic AMP and mechanisms of vasodilation. Pharmacol Ther 47: 329-345.
- Gong YD, Ma HY, Zhang M (2021) New progress in the mechanism, diagnosis and treatment of coronary microvascular disease[J].Chinese Journal of Evidence-Based Cardiovascular Medicine 13: 510-512.
- Kikuchi S, Okada K, Hibi K, Maejima N, Matsuzawa Y, et al. Myocardial infarction caused by accelerated plaque formation related to myocardial bridge in very young male. Can J Cardiol 34: 13-15.
- Li JT, Tian RY (2019) Clinical value of combined detection of CKMB, cTn, Myo and BNP in early diagnosis of acute myocardial infarction. Hebei Medical Journal 41: 1779-1783.
- Liu L M, Zhu S M, Liu X (2021) Maternal and Child Health Care of China. Maternal and Child Health Care of China 36: 194-197.
- Zhao LY, Sun YX, Li YM (2020) Chinese expert consensus on prevention and treatment of hypertension complicated with atherosclerosis. Chinese Journal of Hypertension 28: 116-123.
- Yang S, Yu B (2021) Interaction between smoking and statins in coronary atherosclerosis. Chinese Journal of Cardiovascular Rehabilitation Medicine 30: 366-370.
- Wei BY, Liang MH (2021) Research progress of mechanism of diabetes mellitus causes atherosclerosis. Chinese Journal of Cardiovascular Rehabilitation Medicine 30: 85-87.
- Guo SH, Fu XL, Zha LH (2015) Clinical efficacy of Suxiao Jiuxin pill combined with tirofiban hydrochloride sodium chloride injection in the treatment of patients with acute coronary syndrome and its effect on serum hsCRP, Cys-C and BNP. medical clinical research 32: 2191-2194.
- Zhang GQ, Ni ZY, Lv LL (2019) Efficacy and mechanism of atorvastatin combined with fasudil in the treatment of elderly unstable angina pectoris. International Journal of Geriatrics 40: 341-343.
- Jacobs D, Wassell K, Guidry TJ, Sullivan J (2020) Safety Outcomes of Atorvastatin 80 mg Versus Atorvastatin 40 mg in a Veteran Population. Annals of Pharmacotherapy 54: 151-156.
- Yang B (2021) Effects of different doses of atorvastatin on related indexes in patients with unstable angina pectoris. China Practical Medicine 16: 140-143.
- Cerrato E, Barbero U, D’ascenzo F, Taha S, Zoccai GB, et al. (2017) What is the optimal treatment for symptomatic patients with isolated coronary myocardial bridge? A systematic review and pooled analysis. J Cardiovasc Med 18: 758-770.
- Zhou JH, Huang W, Deng J (2021) Meta-analysis of the therapeutic effect of acupuncture on stable angina pectoris. Journal of Hubei University of Chinese Medicine 20: 38-41.
- Lin HF, Su H, Shi ZY (2020) Clinical Study on Acupuncture and Moxibustion in Treating Acute Coronary Syndrome. Inner Mongolia Journal of Traditional Chinese Medicine 39: 98-100.
- Su H, Lin HF, Yu WQ (2020) Effects of traditional Chinese medicine acupuncture and moxibustion on the quality of life of patients with acute coronary syndrome. Inner Mongolia Journal of Traditional Chinese Medicine 39: 95-97.
Citation: Sun M, Zheng H, Wu Z, Wei Y, Yan A, et al. (2022) Acute Coronary Syndrome (ACS), a Special Case Report. J Altern Complement Integr Med 8: 239.
Copyright: © 2022 Minghui Sun, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

