Acute Early Graft Dysfunction Following Off Pump Coronary Surgery: A Case of Air Embolism
*Corresponding Author(s):
Giorgio ViganoDepartment Of Cardiothoracic Surgery, University-Medical-Centre-Groningen, Groningen, Netherlands
Tel:+31 50 3611327,
Email:g.vigano@umcg.nl
Abstract
Graft patency represents the most relevant issue in coronary surgery, whether on (ONCAB) or off pump (OPCAB). During the last decade major efforts have been made in managing all the multiple factors involved in graft dysfunction, such as more accurate techniques of harvesting and anastomosis, careful graft manipulation, coronary territory distribution and graft quality evaluation. Besides intraoperative graft evaluation have been proposed in order to achieve optimal results. Nevertheless graft dysfunction may occur with inherent complications and sequelae. In these cases, coronary angiography remains the gold standard, since it represents a prompt diagnostic as well as therapeutic solution. In the present case we describe and discuss a temporary acute graft dysfunction, due to air embolism detected by coronary angiography. Since Transit Time Flow Measurement (TTFM) was intra-operatively performed, we investigated additional potentials of TTFM in detecting air embolism.
INTRODUCTION
Carbon dioxide (CO2) blower improves visualization of the anastomotic site in off pump coronary surgery (OPCAB). Despite of a higher solubility in blood, the use of CO2 has been associated with potential embolic events in the circulatory system. We herein report a case of gaseous embolism, detected by coronary angiography. Since Transit Time Flow Measurement (TTFM) was intra-operatively performed, we investigated additional potentials of TTFM in detecting air embolism.
CASE REPORT
A 71 year-old woman was hospital admitted owing to exertional angina, in presence of a two-vessel coronary artery disease (Figure 1).
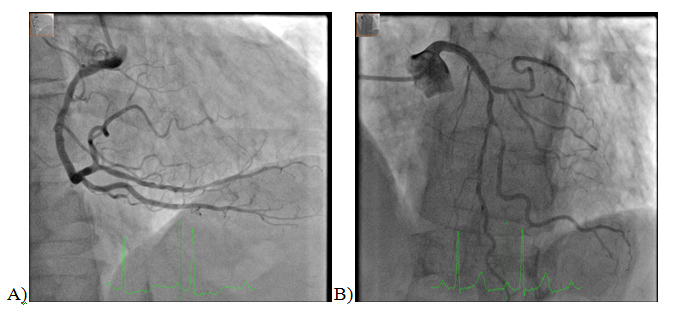 Figure 1: Preoperative coronary angiography. Right dominant coronary system. A) Right Anterior Oblique (RAO 20.3°), cranial 2.3°projection of the right coronary artery (RCA). Wall irregularities, in absence of severe stenosis. B) Left Anterior Oblique (LAO 28.3°), cranial 26.8°projectionof the left coronary artery (LCA). Severe distal left main bifurcation lesion, in presence of significant stenosis of the first diagonal branch (D1) and a small circumflex artery (LCx).
Figure 1: Preoperative coronary angiography. Right dominant coronary system. A) Right Anterior Oblique (RAO 20.3°), cranial 2.3°projection of the right coronary artery (RCA). Wall irregularities, in absence of severe stenosis. B) Left Anterior Oblique (LAO 28.3°), cranial 26.8°projectionof the left coronary artery (LCA). Severe distal left main bifurcation lesion, in presence of significant stenosis of the first diagonal branch (D1) and a small circumflex artery (LCx).
The patient underwent an incomplete revascularization (OPCAB), owing to a too small for grafting obtuse marginal branch (OM). Because of an unfavorable anatomy for a jump graft, in situ Left Internal Mammary Artery (LIMA) was grafted to Left Anterior Descending Artery (LAD), while Saphenous Vein Graft (SVG) was grafted to first diagonal branch (D1) from the ascending aorta. Aortic proximal anastomosis was performed under aortic side-clamping. The two distal anastomoses were performed with an intra-coronary shunt (ClearView® Intracoronary Shunt, Medtronic Inc. 1.75mm and 2.0mm respectively). Before tying the suture, the intra-coronary shunt was retrieved and the graft flushed by removing the proximal bulldog. Carbon dioxide (CO2) blower (Axius MAQUET Holding B.V. & Co. KG) provided controlled delivery of CO2 (flow of 4 l/min; pressure of 50mmHg) and saline to improve visibility during anastomosis. Transit Time Flow Measurement; (VeriQTM Medistim-ASA, Oslo-Norway) was performed twice; after each anastomosis and once Protamine was given. At the last TTFM the following values were detected: LIMA-LAD flow (Q) 15cc/min; Pulsatility Index (PI) 2.9; Diastolic Filling (DF) 73%; AcousticCoupling Index 93%; SVG-D1 Q 10cc/min; PI 5.3; DF 57%; ACI 100% (Figure 2).
 Figure 2: Intraoperative Transit Time Flow Measurement (TTFM) of saphenous vein graft to first diagonal (SVG to D1).
Figure 2: Intraoperative Transit Time Flow Measurement (TTFM) of saphenous vein graft to first diagonal (SVG to D1).
Once transferred to Intensive Care Unit (ICU), owing to several episodes of dynamic overall ST-segment elevation, bradycardia and hypotension the patient was brought to the cardiac catheterization laboratory. Coronary angiography revealed air bubbles trapped at anastomotic site between SVG-D1(Figure 3 and Video 1).
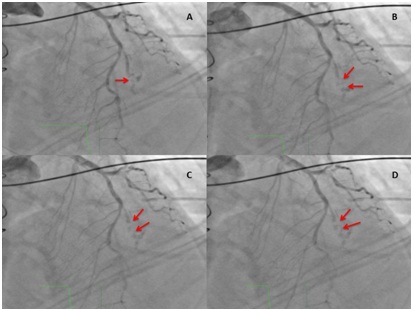 Figure 3: Temporary sequence of postoperative coronary angiography. Left Anterior Oblique (LAO 0.1°) cranial 36.2°projection of the native Left Coronary Artery (LCA). Red arrows show air bubbles migrating towards proximal coronary system (first diagonal - D1). Concomitant distal occlusion of D1.
Figure 3: Temporary sequence of postoperative coronary angiography. Left Anterior Oblique (LAO 0.1°) cranial 36.2°projection of the native Left Coronary Artery (LCA). Red arrows show air bubbles migrating towards proximal coronary system (first diagonal - D1). Concomitant distal occlusion of D1.
Video 1: Postoperative coronary angiography: Left Anterior Oblique (LAO 0.1°), cranial 36.2° projection of the native left coronary artery (LCA). Air is clearly visible at the distal anastomotic site between saphenous vein graft- first diagonal (SVG-D1), with partial dislocation of air bubbles towards proximal coronary system. Distal occlusion of D1.
Selective contrast injection in SVG resulted in dislocation of air bubbles and subsequent ventricular fibrillation. The patient was shortly resuscitated with complete recovery and TIMI 3 flow (Thrombolysis in Myocardial Infarction) in native Left Coronary Artery (LCA). At the end of coronary angiography a right anterior oblique (RAO) caudal projection showed a normal functioning SVG (Video 2).
Click here for Video 2
Video 2: Postoperative coronary angiography: Right Anterior Oblique (RAO 33.9°) Caudal (4.1°) projection of saphenous vein graft (SVG) selectively injected. Air is no longer visible with a good run off and function of venous bypass graft.
DISCUSSION
Air embolism in OPCAB represents a rare, but dreaded complication. Fluid-dynamics and solubilityof gases in blood is complex. Gases dissolve in blood according to a number of variables (concentration, saturation, pressure, temperature and solubility) and to specific laws (Henry’s law). Every gas in contact with blood exists in an equilibrium between dissolved fraction and gaseous fraction. As far as the latter is concerned, the surface tension between gas and blood determines the diameter of the bubble / emboli. The greater the dimensions of the emboli are, the greater the chances to lodge in the body with a variety of consequences, most of which place the patient at some level of risk [1]. Gases rise in blood against the gravity vector, owing to their lower density. The highest points that gas (air) can reach in the circulatory system vary depending on several factors, like patient’s position, centrifugal direction of blood flow and pressure gradients. Since carbon dioxide (CO2) dissolves in blood ≥25 times faster than air, CO2 has been introduced in OPCAB for optimal visualization of the anastomosis with even lower risk of embolism. Although several non-standardized techniques have been developed to assist the CO2 trapped within the heart to escape, de-airing maneuvers cannot totally prevent emboli, therefore early recognition is of great relevance in order to prevent considerable morbidity and mortality [2,3]. CO2 insufflation in the circulatory system may be responsible for massive embolism, that may result in severe consequences such as neurological disorders, myocardial dysfunction and even death [3]. In our reported case two mechanisms occurred: trapped air (CO2) and CO2 embolism. The temporary sequence of the reported events does not allow any definitive conclusion on the pathophysiology of what happened, but allows us to do few considerations. First. Iatrogenic coronary air embolism during coronary angiography has an incidence of 0.1% to 0.3% [4]. Air emboli might be introduced to the coronary arteries along with the contrast injection [5]. In our case air embolism did not occur during catheterization, as no trace of air was visible in the diagnostic catheters and as signs of ischemia were already found on ICU. Second. Several mechanisms of embolism have been reported, frequently in association with major complications [2,6,7]. In our case, air remained long “silent”, most likely trapped by a prominent valve in the vein graft, preventing its detection. No sign of myocardial ischemia was found at the time of operation,Third. Although the surgical blower-mister device represents the most likely source of potential emboli, the origin of gaseous emboli remains speculative. Forth. Gaseous bubbles can temporary prevent graft flow. In case of air blockage Transit Time Flow Measurement (TTFM) can show a suboptimal or no flow in the graft, while it allows to detect air bubbles by epicardial ultrasonography, preventing unnecessary graft revision [8]. According to the European Guidelines, graft evaluation is suggested before leaving the operating theatre (class I; level of evidence C) with recommended TTFM target values [9,10]. In our case, in presence of a suboptimal graft flow, but in absence of clinical signs of ischemia, flowmetry values were merely considered affected by the poor quality of the native coronary system and to the small vessel territory distribution. Owing to the low sensitivity of TTFM in detecting graft failures, particularly in presence of partially failed anastomosis, the proportion of grafts needing revisions in case of inadequate flows remains extremely variable. Whether symptomatic or not, air embolism should be always ruled out, as a possible cause of graft dysfunction, before graft revision. Epicardial Ultrasound imaging adds a value to TTFM, since it allows to detect specific graft issues, such as air embolism. Therefore TTFM could ensure high quality of anastomosis in OPCAB surgery [11,12].
CONFLICT OF INTEREST
The Authors acknowledge no conflict of interest in the submission.
REFERENCES
- Pollard A, Secretain F, Milne B (2014) Air and blood fluid dynamics: at the interface between engineering and medicine. Journal of Physics (Conference Series) 530: 1-16.
- Shim JK, Choi YS, Yoo KJ, Kwak YL (2009) Carbon dioxide embolism induced right coronary artery ischaemia during off-pump obtuse marginalis artery grafting. Eur J Cardiothorac Surg 36: 598-599.
- Kuralay E (2009) Massive systemic air embolism during off-pump coronary artery surgery. Eur J Cardiothorac Surg 35: 183-184.
- Khan M, Schmidt DH, Bajwa T, Shalev Y (1995) Coronary air embolism: incidence, severity, and suggested approaches to treatment. Cathet Cardiovasc Diagn 36: 313-318.
- Suastika LOS, Oktaviono YH (2016) Multiple Air Embolism During Coronary Angiography: How Do We Deal With It? Clinical Medicine Insights: Cardiology 10: 67-70.
- Badreldin AM, Albert AA, Ismail MM, Heldwein M, Doerr F, et al. (2010) Gaseous emboli during off-pump surgery with T-graft technique, two different mechanisms. Interactive CardioVascular and Thoracic Surgery 10: 766-770.
- Hirata N, Kanaya N, Yamazaki Y, Sonoda H, Namiki A (2010) Pulmonary embolism caused by a carbon dioxide blower during off-pump coronary artery bypass grafting. J Anesth 24: 114-116.
- Iino K, Kato H, Yamamoto Y, Takemura H (2016) Air blockage at coronary anastomosis detected by intraoperative epicardial ultrasonography. European Journal of Cardio-Thoracic Surgery 50: 186-187.
- Kolh P, Wijns W, Danchin N, Di Mario C, Falk V, et al. (2010) Guidelines on myocardial revascularization. Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS); European Association for Percutaneous Cardiovascular Interventions (EAPCI). Eur J Cardio-thorac Surg 38: S1-S52.
- Niclauss L (2017) Techniques and standards in intraoperative graft verification by transit time flow measurement after coronary artery bypass graft surgery: a critical review. Eur J Cardiothorac Surg 51: 26-33.
- Desai ND, Miwa S, Kodama D, Koyama T, Cohen G, et al. (2006) A randomized comparison of intraoperative indocyanine green angiography and transit-time flow measurement to detect technical errors in coronary bypass grafts. J Thorac Cardiovasc Surg 132: 585-94.
- Kieser TM, Rose S, Kowalewski R, Belenkie I (2010) Transit-time flow predicts outcomes in coronary artery bypass graft patients: a series of 1000 consecutive arterial grafts. Eur J CardiothoracSurg 38: 155-162.
Citation: Vigano G, de Maat GE, van der Werf HW, Mariani MA (2019) Acute Early Graft Dysfunction Following Off Pump Coronary Surgery: A Case of Air Embolism. Int J Case Rep Ther Stud 1: 001.
Copyright: © 2019 Giorgio Vigano, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.