
Acute High Lateral Myocardial Infarction in a Patient with Covid-19 Pneumonia with Normal Coronary Arteries
*Corresponding Author(s):
Oguz KilicDepartment Of Cardiology, Karaman Research And Training Hospital, Turkey
Tel:+90 5300493033,
Email:dr.kilicoguz@gmail.com
Abstract
ST-Segment Elevation Myocardial Infarction (STEMI) may rarely be a clinical presentation of COVID-19.We present a 70-year-old male patient with no known cardiovascular disease and no conventional risk factors, who applied with STEMI and was diagnosed with COVID-19 infection during follow-up.
Introduction
The coronavirus disease-2019 (COVID-19) was first identified in China. The World Health Organization has described it as a pandemic [1]. It was found to cause diffuse thrombus in both arterial and venous circulation. Together with the evidence showing widespread intracoronary thrombus burden in COVID-19 patients presenting with ST-Segment Elevation Myocardial Infarction (STEMI), it suggests possible pathophysiological links between COVID-19 and acute coronary syndromes [2]. We aimed to present a COVID-19 patient with high lateral STEMI and had normal coronary arteries.
Case Report
A 70-year-old male patient presented to the emergency department with chest pain and shortness of breath lasting for 2 hours. At his admission, he was consciously oriented and cooperative. Arterial blood pressure was 120-80 mmHg, heart rate was 80 bpm and oxygen saturation was 97% on room air. He had no fever. He had no history of cardiovascular disease and conventional risk factors (smoking, hypercholesterolemia, diabetes mellitus, hypertension, or familial history of premature coronary artery disease).
A 12- Lead Electrocardiogram (ECG) showed persistent ST segment elevation in the lateral leads and reciprocal ST depression in D3, and a VF (Figure 1). Echocardiogram revealed hypokinesia of the lateral and posterior walls. Left ventricular ejection fraction measured by the modified Simpson method was 45%. In addition, mild mitral and tricuspid regurgitation were detected. A diagnosis of acute high lateral STEMI was made according to the universal definition of STEMI guidelines. The patient was immediately taken to the catheterization laboratory and coronary angiography was performed immediately. His right and left coronary arteries were completely open and there was no thrombus formation (Figures 2A&B). Laboratory tests, peak high-sensitivity troponin T levels 262 pg/mL, total cholesterol 195 mg/dL, low-density lipoprotein-cholesterol 78 mg/dL, high-density lipoprotein-cholesterol 33 mg/dL, triglycerides 176 mg/dL, d-dimers 1290 ng/mL, C-reactive protein was 20.12 mg/L. Our patient was started on clopidogrel and acetylsalicylic acid. In addition, subcutaneous Low Molecular Weight Heparin (LMWH) in therapeutic dose for 5 days, i.e. enoxaparin 80 mg twice daily, atorvastatin 40 mg and metoprolol 50 mg once a day were given.
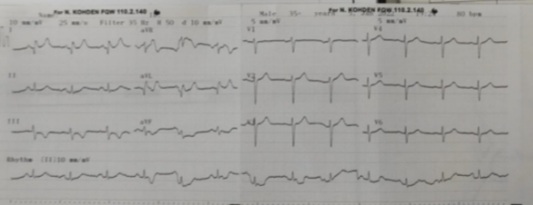 Figure 1: ECG shows obvious ST segment elevation in lateral leads and reciprocal ST segment depression in D3 and aVF.
Figure 1: ECG shows obvious ST segment elevation in lateral leads and reciprocal ST segment depression in D3 and aVF.
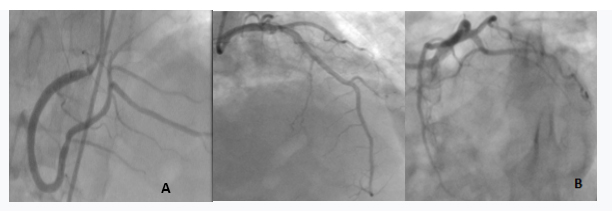
Figure 2: A) Completely patent right coronary artery; B) Left system coronary angiography shows patent left anterior descending and circumflex arteries.
Thorax Computed Tomography (CT) and brain CT were requested to the patient. Ground-glass opacities covering approximately 50% of the lung parenchyma were observed in thorax CT. Pulmonary angiography was negative for pulmonary embolism (Figure 3). Brain CT was normal. The nasopharyngeal swab was positive for SARS-CoV-2 by real-time reverse- transcriptase-polymerase-chain-reaction assay. He was transferred to the pandemic service. 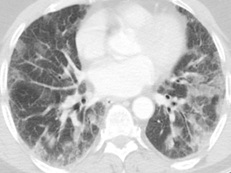
Figure 3: Ground-glass opacities covering approximately 50% of the lung parenchyma.
Discussion
Although COVID-19 often occurs with respiratory distress, studies have shown a significant increase in the risk of thrombosis. These thrombotic conditions are pulmonary embolism, deep vein thrombosis, cerebral infarction [3]. They can also apply with the STEMI clinic. This may be the only symptom of COVID-19. Especially, patients with comorbidities (diabetes mellitus, hypertension, hyperlipidemia and smoking history) are at risk. Our case is unique in the literature with the absence of conventional risk factors, the detection of normal coronary arteries, and the negative results of tests for other thrombotic disorders.
The mechanism that causes thrombus in COVID-19 patients has not been clarified yet. However, it is thought to be endothelial dysfunction caused by the cytokine storm caused by the increased production of pro-inflammatory cytokines (TNF-alpha,IL-1,IL-6) [4]. Thrombin together with endothelial dysfunction leads to coagulation activation. Therefore, we think that endothelial dysfunction and thrombin activation in the background of fibrous plaque erosion are the most likely mechanisms of STEMI [5]. Myocardial infarction with Non-Obstructive Coronary Artery (MINOCA) is clinically defined by the presence of the universal Acute Myocardial Infarction (AMI) criteria, absence of obstructive coronary artery disease (≥50% stenosis) and no overt cause for clinical presentation at angiography (eg, classic features for takotsubo cardiomyopathy) [6]. In our patient, the coronary arteries were also completely open. No major thrombus was observed. We are considering MINOCA due to COVID-19.
Conclusion
COVID-19 may present with STEMI with increased thrombosis. Although anticoagulant therapy may be beneficial in these patients, more studies are needed to elucidate the mechanism and make the treatment more comprehensive.
Acknowledgement
Thank you to Ali Raif Pharmaceutical Company for its support
References
- Levi M, Thachil J, Iba T, Levy JH (2020) Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol 7: 438-440.
- Choudry FA, Hamshere SM, Rathod KS, Akhtar MM, Archbold RA, et al. (2020) High thrombus burden in patients with COVID-19 presenting with ST-segment elevation myocardial infarction. J Am Coll Cardiol 76: 1168-1176.
- Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395: 507-513.
- Del Rio C, Malani PN (2020) 2019 Novel coronavirus-important information for clinicians. JAMA 323: 1039-1040.
- Masi P, Hékimian G, Lejeune M, Chommeloux J, Desnos C, et al. (2020) Systemic inflammatory response syndrome is a major contributor to COVID-19-associated coagulopathy: insights from a prospective, single-center cohort study. Circulation 142: 611-614.
- Agewall S, Beltrame JF, Reynolds HR, Niessner A, Rosano G, et al. (2017) ESC working group position paper on myocardial infarction with non-obstructive coronary arteries. Eur Heart J 38: 143-153.
Citation: Kilic O (2022) Acute High Lateral Myocardial Infarction in a Patient with Covid-19 Pneumonia with Normal Coronary Arteries. J Clin Stud Med Case Rep 9: 0132.
Copyright: © 2022 Oguz Kilic, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

