
Advanced Maternal Age with Severely Diminished Ovarian Reserve with Multiple Successful Live Births after Chinese Herbal Medicine Treatment: A Case Report
*Corresponding Author(s):
Xiaoxiong ShenShen Clinic 1328 W Artesia Blvd, Gardena, CA 90248, United States
Email:xiaoxiongshen@yahoo.com
Abstract
The fecundity of women decreases significantly beginning approximately at age 35 and decreases more rapidly after age 40. Age affects not only the size of the oocyte pool but also the quality of germ cells. Despite the continuous progress of assisted reproductive technology, infertility is still a problem for advanced maternal age. Here, we present case report of a woman who had two successful live births after treatment with Traditional Chinese Medicine. During her initial visit (at age 43), she had a severely diminished ovarian reserve (FSH: 26.2mIU/mL; AMH: 0.23ng/mL) and shorted menstrual cycle. Three years after her first child birth (at age 47), her ovarian reserve was worse (FSH: 27.1 mIU/mL;AMH: 0.07 ng/mL), yet after four months of Chinese herbal medicine treatment, she achieved a second successful pregnancy and live birth. This case demonstrates that Chinese herbal medicine, with thousands of years in the infertility natural remedy, has a positive clinical effect in the improvement of hormones balance and fecundity, which is worth further verification and summary by modern medical scientific methods.
Keywords
Advanced maternal age; Basal body temperature; Case report; Chinese herbal medicine; Infertility; Ovulation; Traditional chinese medicine; Yin and yang
Introduction
It is well established that Advanced Maternal Age (AMA) is associated with a rapid decline in the production of healthy and high-quality oocytes resulting in reduced fertility in women older than 35 years of age [1]. Despite the continuous progress of Assisted Reproductive Technology (ART), infertility is still a problem for women of AMA. Live birth rates, even with In Vitro Fertilization (IVF), in women over 40 years remains low [2,3]. At present, age-related infertility is an intricate clinical dilemma, apart from egg donation, no optimal remedies are available to counteract the aging-related fertility decay [4,5]. Traditional Chinese Medicine (TCM), meanwhile, has been used to treat gynecological diseases for more than 2,500 years. Ancient practitioner Zhang Zhongjing (c. 150-219 ce) wrote special chapters on gynecological pregnancy diseases in the book Essential Prescriptions of the Golden Coffer (Jingui Yaolue) [6]. In recent years, more patients with infertility problems are seeking to utilize TCM to improve their fecundity. Often, infertility patients wish to use Chinese Herbal Medicine (CHM) or/and acupuncture therapy first, and then consider Assisted Reproductive Technology (ART), or turn to CHM or/and acupuncture therapy after the failure of ART. TCM may represent a useful option for female infertility [7], which is worth exploring and summarizing. Therefore, we outline and discuss a case report of a patient of advanced maternal age with severely diminished ovarian reserve infertility who we treated successfully using Traditional Chinese Medicine.
Case Presentation
A 43 year-old female initially visited our clinic was on August 20, 2015, her chief complaint was that she had been trying to conceive for 2 years with a shortened menstrual cycle. Her menarche was at 12 years-old, after then her menstrual cycle was regular without dysmenorrhea. Since 2014, her menstrual cycle to be shorten 25-27 days, the menstrual amount was medium. She had once abortion in 2004. Her Last Menstrual Period (LMP) was on July 24, 2015. Her laboratory test results are as follows: her blood was collected at menstrual cycle day two (on September 11, 2015), Follicle Stimulating Hormone (FSH): 26.2mIU/mL (Postmenopausal: 23-116.3mIU/mL); Luteinizing Hormone (LH): 8.2mIU/mL (follicular phase: 1.9-12.5mIU/mL); Anti-Müllerian Hormone (AMH): 0.23ng/mL (>49yrs 3. Hysterosalpingography (HSG) on September 25, 2015 was normal. Her husband’s semen analysis was determined to be within normal range.
This patient’s diagnosis was secondary infertility, severe diminished ovarian reserve, and frequent menstrual cycle. She had previously consulted with two reproductive clinics, and both had advised her to do IVF. One of them suggested her to do IVF with donated eggs. However, she wanted to first use natural remedies then consider ART. Her Basal Body Temperature (BBT) had shown shorter menstrual cycles of 25 days with slower slope of luteal phase temperature up and down shift during first month of treatment (Figure 1).
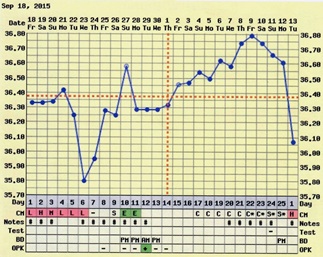 Figure 1: At the beginning of Chinese Herbal Medicine (CHM) treatment, the patient’s Basal Body Temperature (BBT) showed a short menstrual cycle, slower slope of luteal phase temperature with inconsistent shifts in luteal phase deficiency.
Figure 1: At the beginning of Chinese Herbal Medicine (CHM) treatment, the patient’s Basal Body Temperature (BBT) showed a short menstrual cycle, slower slope of luteal phase temperature with inconsistent shifts in luteal phase deficiency.
The treatment we designed was a Chinese herbal formula to help patients improve ovulation function and luteal function, called Fu Kun Tang (Decoction). The ingredients are as follows: Rehmanniae Radix preparate (Shu Di Huang) 15g, Ligustrilucidi Fructus (Nv Zhen Zi) 12g, Corni Fructus (Shan Zhu Yu) 20g, Cuscutae Semen (Tu Su Zi) 15g, Cistanches Herba (Rou Cong Rong) 15g, Angelicae sinensis Radix (Dang Gui) 12g, Salvia miltiorrhiza Radix (Dan Shen) 12g, Cyperi Rhizoma (Xiang Fu) 12g. During the luteal phase, we modified the formula and added Lycii Cortex (Di Gu Pi) 15g, Anemarrhenae Rhizoma (Zhi Mu) 12g, Phellodendri Cortex (Huang Bai) 12g. During later follicular and ovulation phase, we added Epimedii Herba (Xian Ling Pi) 12g, Curculiginis Rhizoma (Xian Mao) 12g, Leonuri Fructus (Chong Wei Zi) 12g. Instructions to prepare these raw herbs were to add 600 ml of water, gently boil for 25 minutes and drink the decoction, twice daily. We treated her with the basic formula “Fu Kun Tang” along with modification, as specified above, and after three months of Chinese herbal medicine treatment alone, she had two chemical pregnancies in December 2015 and January 2016 (Figure 2). Due to frustration and stress, she temporarily stopped taking the herbs for four months, from April to June 2016. After she stopped taking the herbs, she discovered that her menstrual cycle shorted again, she decided to continue to take the herbs. After treatment for two more months, her LMP was August 2, 2016, and her urine pregnancy test was positive on August 24 (Figure 3), and a health boy was born on May 4, 2017.
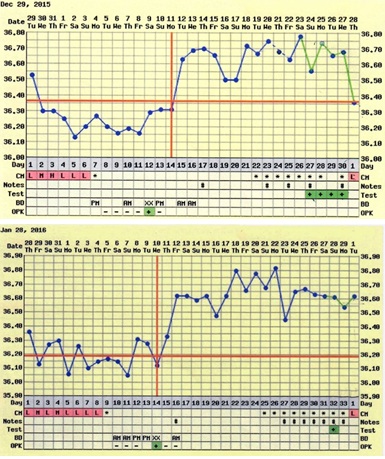 Figure 2: After CHM treatment, the patient had two positive pregnancies, with basal body temperature showing chemical pregnancies.
Figure 2: After CHM treatment, the patient had two positive pregnancies, with basal body temperature showing chemical pregnancies.
 Figure 3: After CHM treatment, the patient’s urine pregnancy test positive on August 23, 2016, and a health boy was born on May 4, 2017.
Figure 3: After CHM treatment, the patient’s urine pregnancy test positive on August 23, 2016, and a health boy was born on May 4, 2017.
On Jun 20, 2020, she returned to our clinic again at 47 years-old, her chief complaint was that she had been trying to conceive a second child for about 2 years. Menstrual cycle was a shortened 22-27 days, amount of medium, without menstrual cramp. On her return visit her LMP was on June 11, 2020, her BBT showed the shortening of the length of her menstrual cycle with luteal phase deficiency (Figure 4). Laboratory blood test result were collected at menstrual cycle day two (November 19, 2020): FSH: 27.1 mIU/mL (Postmenopausal: 23-116.3mIU/mL); LH: 5.2 mIU/mL (follicular phase: 1.9-12.5); FSH/LH> 5; AMH: 0.07 ng/mL (>49yrs <0.45). After treatment of Fu Kun Tang decoction with modifications for five months, her LMP was on November 18, 2020, and her urine pregnancy test positive on December 10, 2020 (Figure 5). Additionally, her blood test for Human Chorionic Gonadotropin (hCG) was 431mIU/mL (>5 mIU/mL pregnancy) on December 15, 2020. Her Noninvasive Prenatal Testing (NIPT) result showed low risk for microdeletions aneuploidies, and the fetal sex was determined to be male on January 27, 2021. A health boy was born on August 20, 2021.
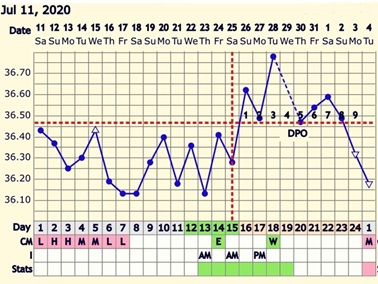 Figure 4: Patient returned on Jun 20, 2020 at 47 year-old, she was attempting to conceive a second child for about 2 years. Before CHM treatment, the patient’s BBT showed short menstrual cycle with luteal phase deficiency.
Figure 4: Patient returned on Jun 20, 2020 at 47 year-old, she was attempting to conceive a second child for about 2 years. Before CHM treatment, the patient’s BBT showed short menstrual cycle with luteal phase deficiency.
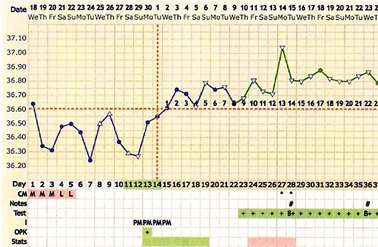 Figure 5: After CHM treatment, the patient’s urine pregnancy test was positive on December 10, 2020, and Noninvasive Prenatal Testing (NIPT) result shown microdeletions aneuploidies low risk, fetal sex was male. The health boy was born on August 20, 2021.
Figure 5: After CHM treatment, the patient’s urine pregnancy test was positive on December 10, 2020, and Noninvasive Prenatal Testing (NIPT) result shown microdeletions aneuploidies low risk, fetal sex was male. The health boy was born on August 20, 2021.
Discussion
Age-related infertility is often considered a problem that can be easily solved by the application of ART. However, it is well established that maternal age is associated with a rapid decline in the production of healthy and high-quality oocytes resulting in reduced fertility in women older than 35 years of age, even with ART treatment. Despite the profound changes in numbers and quality of follicles, the process of ovarian aging remains largely unnoticed. The events that can be quite easily recognized are cycle irregularity, with the first subtle clinical sign of advancement in the reproductive aging process is a shortening of the length of the menstrual cycle by 2-3 days [8], shortened follicular phase with elevated FSH [9], and FSH rise occurring earlier during the luteal phase [10]. This suggests that dominant follicle growth starts earlier, even before the onset of menses, with higher levels of estradiol present in the subsequent early follicular phase. The main reasons for age-related infertility include reduced ovarian reserve and decreased oocyte/embryo competence due to aging insults, especially concerning an increased incidence of aneuploidies, and possibly decreased mitochondrial activity [11].
The patient in this case had severely diminished ovarian reserve case, whose blood test results shown baseline FSH was over 26 when her initial visiting, and when she was expecting second child, the baseline FSH was 27.10, AMH was 0.07, and with a shorted menstrual cycle. For AMH, low ovarian reserve was defined at < 0.7 ng/mL [12]. AMH hormone seems to be the best endocrine marker for assessing the age-related decline of the ovarian pool in healthy women, the age effect on live birth was more strongly mediated by AMH and less by FSH [13]. Her examination results indicated that the patient's hormone level was close to menopause with the loss of ovarian follicular pool. Lower AMH is independently associated with lower live birth and higher IVF cycle cancellation rates [14], and it has been suggested that 45 years should be considered the highest age-threshold to undergo IVF with own egg [15].
With the loss of ovarian follicular pool and cycle shortening, it is an open question whether any remedy can make shortened menstrual cycles return to normal. Fu Qing-zhu, a TCM gynecologist in the Chinese Qing dynasty (1607-1684), who wrote a famous gynecological monograph, named “Fu Qing-zhu Gynecology”, which included a special chapter that discusses the disease of “shorted menstrual cycle”, in which he contributed two herbal formulas [16], both of which have been still used in TCM clinical practice now. The concept of Yin and Yang serves as the foundation for understanding health, as well as diagnosing and treating illness. TCM believes that Yin and Yang maintain a dynamic balance during the whole menstrual cycle, according to ancient literatures, we have been drawn the Taiji Yin-Yang diagram of menstrual cycle to illustrate the dynamic balance in the menstrual cycle (Figure 6). The primordial eight trigrams (Ba Gua) are originated from China, each consists of three lines, "broken" line (- -) and dark park are representing Yin, on the another hand, “unbroken” line (¾) and white (bright) part are representing Yang. Yin and Yang are opposite, as well as interdependent, they are mutually transformative and consuming, and derives everything, which forms the cycle of the movement and change of things and maintains the homeostasis of Yin and Yang in the whole monthly Taijicycle. A synchronous relationship between the menstrual cycle and lunar rhythm has been illustrated by investigative data [17-19], and Qing dynasty practitioner Tang Rongchuan (1846-1897) mentioned the full moon should be in the pure Yang, new moon should be in the pure Yin. During the follicular phase, Yin generate Yang, and the Yang will be maximum until ovulation, with the Yang meaning dominant, creativities, strengthen, warm, movement, activate, upgrade and positive feedback. During the luteal phase, Yang generate Yin, and the Yin will be maximum until menstruation. Yin means compliance, obedience, smooth, peaceful, sequence, downgrade, and negative feedback. This Yin-Yang theory of TCM accords with the theory of modern reproductive medical principle, Yang phase (preovulation to midluteal phase) indicate higher levels of sex hormones, where positive feedback is in the effect of LH on estrogen, and more LH leads to more upstream estrogen release. On the other hand, Yin phase (late luteal phase to early follicular phase) indicate lower of levels of sex hormones, and negative feedback, conversely, is in the effects of progesterone on GnRH and LH levels, where increased progesterone levels decrease the upstream release of GnRH and LH [20,21].
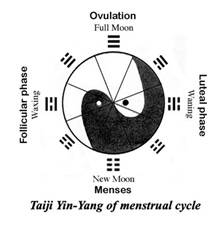 Figure 6: Illustration of Taiji Yin-Yang of menstrual cycle. “broken” line (- -) and dark park are representing Yin, “unbroken” line (¾) and white (bright) part are representing Yang. During the follicular phase, Yin generate Yang, the Yang will be gradually maximum until ovulation. During the luteal phase, Yang generate Yin, the Yin will be gradually maximum until menstruation.
Figure 6: Illustration of Taiji Yin-Yang of menstrual cycle. “broken” line (- -) and dark park are representing Yin, “unbroken” line (¾) and white (bright) part are representing Yang. During the follicular phase, Yin generate Yang, the Yang will be gradually maximum until ovulation. During the luteal phase, Yang generate Yin, the Yin will be gradually maximum until menstruation.
Therefore, “the concepts of Yin and Yang provided the intellectual framework of much of Chinese scientific thinking, especially in the fields of biology and medicine” [22]. According to this Yin-Yang principle, we prescribed an herbal formula named “Fu Kun Tang” to promote ovulation and promote regular menstruation. “Fu Kun Tang” has been demonstrated by clinic trial and animal experiments that the decoction can significantly promote the ovarian development of pubertal mice aged 26-30 days (P<0.05) (Figure 7) [23]. To treat the shorted menstrual cycle, during the luteal phase, we add herbs to nourish Yin, such as Lycii Cortex, Anemarrhenae Rhizoma, Phellodendri Cortex, with the purpose of controlling FSH levels to prevent the antral follicular growth early in luteal phase. During later follicular and ovulation phase, we add herbs to tonify the Yang, such as Epimedii Herba, Curculiginis Rhizoma, Leonuri Fructus, with purpose of improving the follicular quality and elevate the LH peak during ovulation. With Epimedii Herba, modern pharmacological experiments have shown that the main active ingredients of epimedium include Total Flavonoids of Epimedium (TFE), and Icariin (ICA). Rat ovary granulosa cells were cultured in vitro and treated with different concentrations of icariin, the results showed that icariin can promote the secretion of estradiol and progesterone through up-regulation of CYP17 and CYP19, icariin could improve the ovarian endocrine function through these effects [24]. In vivo experiment of rats, icariin administration elevated the serum levels of female hormone Estradiol (E2), Testosterone (T), and Interleukin (IL)-2, decreased those of FSH and LH, promoted the expression levels of Estrogen Receptor (ER) and ERα in the hypothalamus [25]. Given these previous pharmacological studies, we hypothesize that some herbs for tonifying Yang have the effect of increasing hormone receptor sensitivity. However, the mechanism of Chinese herbal medicine remains to be confirmed, and further clinic trials and molecular experiments are necessary.
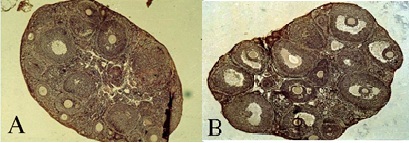 Figure 7: H&E staining was performed on the vertical sections of the mice ovaries (X100). Oral administration of CMH formula of Fu Kun Tang extract 0.3ml/10gram body weight for seven days, inpubertal mice aged 26-30 days body and weight 17-19 gram. Representative histologic images are shown (A) control group of mice were treated with sterilization of water; (B) The Fu Kun Tang group of mice were treated with herbal extract. Results have been shown that herbal group has significant mature follicular counts vs. control group. n=15/group, P
Figure 7: H&E staining was performed on the vertical sections of the mice ovaries (X100). Oral administration of CMH formula of Fu Kun Tang extract 0.3ml/10gram body weight for seven days, inpubertal mice aged 26-30 days body and weight 17-19 gram. Representative histologic images are shown (A) control group of mice were treated with sterilization of water; (B) The Fu Kun Tang group of mice were treated with herbal extract. Results have been shown that herbal group has significant mature follicular counts vs. control group. n=15/group, P
BBT measurements have been used for decades to help women optimize the timing of intercourse during a fertile window [26]. Although, studies have expressed the viewpoint that BBT is an unreliable technique to determine accurate ovulation timing, but would be of use if the clinical precision required for the diagnosis of ovulation were less [27]?and revealed under recognized age-dependent changes in menstrual cycle length and BBT, which will contribute to a better understanding of female reproductive health [28]. The amplitude of the temperature rise was independent of the progesterone concentration and the type of hormonal stimulation [29], whilst LH test kits have been used to determine the day of ovulation for decades, they have a significant margin of error when used in isolation, the addition of BBT and the use of a fertility app may help to narrow down testing days. Additional it is a valuable method to dynamic indicator for retrospective analysis of ovulatory, luteal function, chemic pregnancy, Luteinizing Unruptured Follicle syndrome (LUFs), and evaluation of treatment effectiveness. Therefore, BBT is as a valuable utilized method to indirectly detect changes in a woman's hormone cycle, to identify ovulation and in turn luteal phase length can give insights into individual fertility and potentially support early identification of subfertility, because of its inexpensiveness, ease, and painlessness.
Conclusion
This clinical case suggests that TCM which has a history of more than 2000 years in the treatment of infertility, could have a certain clinical effect on improving reproductive endocrine function and helping natural conception. Even for IVF patients, TCM can be considered as a treatment to improve the conditions of conception before procedure or as an alternative treatment after failure. In addition, in most cases, personalized identification of the fertility window based on BBT and menstrual date can help reduce the time to conception. This clinical case suggests the viability of TCM as a treatment option of infertility and that we can use the methods of modern medicine including molecular biology to verify the curative effect of Traditional Chinese medicine and reveal the clinical mechanism of traditional Chinese medicine.
Funding
No external funding was received for this case report.
Conflict of Interest
The authors have declared that no conflict of interest exists.
Consent
Author informed consent was obtained from the patient for publication of this case report.
References
- Mikwar M, MacFarlane AJ, Marchetti F (2020) Mechanisms of oocyte aneuploidy associated with advanced maternal age. Mutat Res Rev Mutat Res 785: 108320.
- Fernandez AM, Drakopoulos P, Rosetti J, Uvin V, Mackens S, et al. (2021) IVF in women aged 43 years and older: A 20-year experience. Reprod Biomed Online 42: 768-773.
- Hipp H, Crawford S, Kawwass JF, Boulet SL, Grainger DA, et al. (2017) National trends and outcomes of autologous in vitro fertilization cycles among women ages 40 years and older. J Assist Reprod Genet 34: 885-894.
- Ubaldi FM, Cimadomo D, Vaiarelli A, Fabozzi G, Venturella R, et al. (2019) Advanced Maternal Age in IVF: Still a Challenge? The Present and the Future of Its Treatment. Front Endocrinol (Lausanne) 10: 94.
- Somigliana E, Paffoni A, Busnelli A, Filippi F, Pagliardini L, et al. (2016) Age-related infertility and unexplained infertility: An intricate clinical dilemma. Hum Reprod 31: 1390-1396.
- Shen X, Bagherigaleh S (2019) Acupuncture and Pregnancy: Classical Meets Modern. Med Acupunct 31: 248-250.
- Ried K, Stuart K (2011) Efficacy of Traditional Chinese Herbal Medicine in the management of female infertility: A systematic review. Complement Ther Med 19: 319-331.
- Broekmans FJ, Soules MR, Fauser BC (2009) Ovarian aging: Mechanisms and clinical consequences. Endocr Rev 30: 465-493.
- Miro F, Aspinall LJ (2005) The onset of the initial rise in follicle-stimulating hormone during the human menstrual cycle. Hum Reprod 20: 96-100.
- van Zonneveld P, Scheffer GJ, Broekmans FJ, Blankenstein MA, de Jong FH, et al. (2003) Do cycle disturbances explain the age-related decline of female fertility? Cycle characteristics of women aged over 40 years compared with a reference population of young women. Hum Reprod 18: 495-501.
- Cimadomo D, Fabozzi G, Vaiarelli A, Ubaldi N, Ubaldi FM, et al. (2018) Impact of Maternal Age on Oocyte and Embryo Competence. Front Endocrinol (Lausanne) 9: 327.
- Steiner AZ, Herring AH, Kesner JS, Meadows JW, Stanczyk FZ, et al. (2011) Antimüllerian hormone as a predictor of natural fecundability in women aged 30-42 years. Obstet Gynecol 117: 798-804.
- Meczekalski B, Czyzyk A, Kunicki M, Podfigurna-Stopa A, Plociennik L, et al. (2016) Fertility in women of late reproductive age: The role of serum Anti-Müllerian Hormone (AMH) levels in its assessment. J Endocrinol Invest 39: 1259-1265.
- Ligon S, Lustik M, Levy G, Pier B (2019) Low Antimüllerian Hormone (AMH) is associated with decreased live birth after in vitro fertilization when follicle-stimulating hormone and AMH are discordant. Fertil Steril 112: 73-81.
- Ubaldi FM, Cimadomo D, Capalbo A, Vaiarelli A, Buffo L, et al. (2017) Preimplantation genetic diagnosis for aneuploidy testing in women older than 44 years: A multicenter experience. Fertil Steril 107: 1173-1180.
- Qing-Zhu F (2002) Fu Qing-Zhu’s Gynecology. Blue poppy press Inc.
- Law SP (1986) The regulation of menstrual cycle and its relationship to the moon. Acta Obstet Gynecol Scand 65: 45-48.
- Luo S, Luo Y (1984) Preliminary study on the relationship between menstrual rhythm and lunar phase. Shanghai J TCM (Chinese): 42-44.
- Helfrich-Förster C, Monecke S, Spiousas I, Hovestadt T, Mitesser O, et al. (2021) Women temporarily synchronize their menstrual cycles with the luminance and gravimetric cycles of the Moon. Sci Adv 27: eabe1358.
- Simic N, Ravlic A (2018) Changes in basal body temperature and simple reaction times during the menstrual cycle. Arh Hig Rada Toksikol 64: 99-106.
- Terasawa Ei (2018) Neuroestradiol in regulation of GnRH release. Horm Behav 104: 138-145.
- Dutt T, Toh CH (2008) The Yin-Yang of thrombin and activated protein C. Br J Haematol 140: 505-515.
- Shen X, Chen D, Sheng Y, Yang Z (1988) Clinical Observation and Experimental Study on Treatment of Anovulatory Menstruation with Fu Kun Tang (Chinese). J TCM 29: 40.
- Nie X, Sheng W, Hou D, Liu Q, Wang R, et al. (2019) Effect of Hyperin and Icariin on steroid hormone secretion in rat ovarian granulosa cells. Clin Chim Acta 495: 646-651.
- Cao LH, Qiao JY, Huang HY, Fang XY, Zhang R, et al. (2019) PI3K-AKT Signaling Activation and Icariin: The Potential Effects on the Perimenopausal Depression-Like Rat Model. Molecules 24: 3700.
- Steward K, Raja A. (2021) Physiology, Ovulation and Basal Body Temperature. Stat Pearls Publishing, Island.
- de Mouzon J, Testart J, Lefevre B, Pouly JL, Frydman R (1984) Time relationships between basal body temperature and ovulation or plasma progestins. Fertil Steril 41: 254-259.
- Tatsumi T, Sampei M, Saito K, Honda Y, Okazaki Y, et al. (2020) Age-Dependent and Seasonal Changes in Menstrual Cycle Length and Body Temperature Based on Big Data. Obstet Gynecol 136: 666-674.
- Forman RG, Chapman MC, Steptoe PC (1987) The effect of endogenous progesterone on basal body temperature in stimulated ovarian cycles. Hum Reprod 2: 631-634.
Citation: Shen X (2022) Advanced Maternal Age with Severely Diminished Ovarian Reserve with Multiple Successful Live Births after Chinese Herbal Medicine Treatment: A Case Report. J Reprod Med Gynecol Obstet 7: 094.
Copyright: © 2022 Xiaoxiong Shen, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

