
Aerobic Exercise in the Fasted State for Type 2 Diabetic Patient with Coronary Artery Disease - Protocol and Case Report
*Corresponding Author(s):
M ArdériusServico De Medicina Iii, Hospital Pulido Valente, Alameda Das Linhas De Torres 117, 1769-001 Lisboa, Portugal
Email:miguel_arderius@hotmail.com
Abstract
Introduction: Exercise is beneficial for health and, when practiced while fasting, can have additional gains (increased consumption of lipids, aerobic capacity and glucose tolerance), being safe in healthy subjects. In diabetics not on insulin, it seems to have an inferior glucose lowering effect and to attenuate the postprandial glycaemic increase, but there are concerns about its safety.
Objective: To present our exercise protocol and to evaluate the effect of fasting in the glycemic profile, cardiovascular safetyand ketonemia during exercise in patient with Type 2 Diabetes (T2DM) and Coronary Artery Disease (CAD).
Methods: Patients with T2DM and CAD were invited to perform 6 trials of continuous moderate intensity aerobic exercise, 3 of which in the Fasted State (FS). We monitored glucose and ketone levels, signs and symptoms and electrocardiographic changes.
Results: A 63-year-old man being treated with metformin completed the protocol. No relevant clinical or electrocardiographic changes were found. Postprandial exercise showed a greater glucose lowering effect than FS. No hypoglycaemia was detected. The difference between interstitial glucose and capillary glycaemia increased when glycaemia was changing fast. All ketonemia tests were negative.
Conclusions: FS exercise was safe in this high-risk patient, with an inferior glucose lowering effect. This protocol could be applied in further studies to better understand the effect of FS exercise in patients with T2DM and CAD.
Keywords
Aerobic exercise; Coronary artery disease; Fasted state; Flash glucose monitoring; Freestyle Libre; Glycemia; Glycemic profile; Ischemic cardiomyopathy; Type 2 diabetes mellitus
ABBREVIATIONS
DM: Diabetes Mellitus
CAD: Coronary Artery Disease
FS: Fasted State
PP: Postprandial
T2DM: Type 2 Diabetes Mellitus
BP: Blood Pressure
EKG: Electrocardiographic Monitoring
IG: Interstitial Glucose
CG: Capillary Glycaemia
INTRODUCTION
Diabetes Mellitus (DM) has become a worldwide epidemy with rising prevalence [1]. It is associated with a fourfold increase in mortality risk from heart disease, and Coronary Artery Disease (CAD) is the main cause of death in both type 1 and type 2 diabetics [2].
Exercise is known to have major beneficial effects on health, including decreased cardiovascular disease and all-cause mortality [3], being recommended 3 to 5 times a week (150 minutes a week) for type 2 diabetics [4,5].
Fasted State (FS) aerobic exercise appears to improve consumption of lipids as a substrate [6,7], aerobic capacity [8], oral glucose tolerance, insulin sensitivity and muscle capacity for transporting and oxidizing fat [9,10], making it attractive for both recreational and elite athletes. Its practice seems to be safe in healthy subjects and to have inferior glucose lowering effect when compared with Postprandial (PP) exercise [11], even in type 2 diabetics not on insulin [12-14]. Beyond these announced benefits, which are appealing to both the general population and particularly for diabetics, there is also some evidence of attenuation of the postprandial glycaemic increase [15]. However, there are still concerns about its safety, namely because the risk of myocardial ischemia seems to be lower in the fed state [16,17].
The relationship between exercise, nutrition and metabolism is highly complex and far from being fully understood [18], and thus there is still no universal consensus regarding the effects of feeding patterns and its results [19], making this a very interesting area of investigation.
We intend to present our exercise protocol and to evaluate the effects of fasting in the glycaemic profile, cardiovascular safety and ketonemia in a high risk patient with Type 2 DM (T2DM) during aerobic exercise.
METHODS
Participants: Volunteer with previous diagnosis of T2DM and CAD, aged between 40 and 75 years old and participating in a cardiovascular rehabilitation program.The exclusion criteria were: Corticosteroid therapy, history of hypoglycaemia (grade 2 [<54mg/dL] or grade 3 [associated with severe cognitive changes requiring assistance in the recovery]) in the previous three months, therapy with insulin or glibenclamide and physical inability to perform moderate effort [20]. The protocol was approved by the local Ethics Committee and all participants signed written informed consent forms.
Experimental design: Interventional study, prospective cohort. Each participant was proposed to complete six trials of continuous moderate intensity aerobic exercise (defined as 70-80% of the heart rate reserve), in a LifeFitness® cycle ergometer, with 45 minutes duration, three of which in a FS and the other three PP (1.5 hours after a meal of approximately 480cal/2009kJ), in a randomized order.The trials were carried out with an interval of 2-3 days. During the trials, only water consumption was allowed, restriction that was extended to the 10 hours before every FS trial. In the 30 minutes that followed each trial, a similar meal took place (480cal/2009kJ). All trials were performed under similar conditions - same place, equipment, room temperature and at the same time of the day - with medical supervision and within 2 weeks. The postprandial meal was a glass of milk and bread with ham or cheese.
Clinical monitoring: Participants were asked about symptoms, namely hunger and fatigue at 0, 25 and 45 minutes of each trial, but were free to report any symptom at any time. Blood Pressure (BP) was measured at 0, 25 and 45 minutes.
Electrocardiographic monitoring: Continuous 6-lead Electrocardiographic monitoring (EKG) took place with a Norav Medical ECG NM700.
Glucose and ketones monitoring: Participants used a last generation flash glucose monitoring system (Abbott Freestyle Libre™), consisting of a small disposable sensor inserted into the skin that measures glucose in the interstitial fluid, estimating its blood concentration every 5 minutes during the exercise trials. Capillary measurement with Abbott Freestyle Precision™ and Freestyle β-ketone™ strips was done at 0, 25 and 45 minutes.
Statistical analysis: Data was analysed using the SPSS statistical software (SPSS Inc., Version 22, NY, USA). A descriptive analysis was done.
CASE REPORT
One 63-year-old man, obese (body mass index 30.4kg/m2, abdominal perimeter 112cm), with previous history of T2DM, CAD, essential hypertension and dyslipidaemia. The T2DM was diagnosed 5 years before and was well controlled (HbA1c 6.4%) with metformin 850mg twice daily. The CAD was diagnosed 1 year before and submitted to a triple coronary artery bypass graft. The essential hypertension and dyslipidaemia were diagnosed 6 years before, with pre-test evaluation showing a blood pressure of 133/75mmHg, total cholesterol of 188mg/dL, triglycerides of 186mg/dL, high-density lipoprotein cholesterol of 42mg/dL and low-density lipoprotein cholesterol of 109mg/L. The patient performed six exercise trials, three of which in the fasted state. All exercise trials were analysed, comparing fasted state with postprandial.
Clinical monitoring: In the minutes that preceded the beginning of two FS trials, the patient mentioned hunger, and in one of those he also mentioned mild dizziness. These symptoms were not accompanied by any changes in the BP, EKG, glycaemia or ketonemia and all quickly disappeared after the start of the trials. There were no symptoms mentioned in the other FS trial nor in any PP trial. Blood pressure was similar in all trials, with a slight increase in the first 25min and stabilization after that (Table 1).
|
|
|
0min |
25min |
45min |
|
Fasted State |
Systolic blood pressure |
130 |
161 |
158 |
|
Diastolic blood pressure |
81 |
67 |
77 |
|
|
Postprandial State |
Systolic blood pressure |
136 |
163 |
155 |
|
Diastolic blood pressure |
69 |
77 |
74 |
Table 1: Average blood pressure on each stage of the exercise trials.
Data presented as mean, in mmHg
Electrocardiographic monitoring: There were no relevant findings in the 6-lead EKG, namely no changes in the intraventricular conduction, no changes in repolarization and no malignant arrythmias.
Interstitial glucose (IG) levels: In the beginning of the exercise trials, glucose levels were higher in the postprandial state (190 vs 131mg/dL). During the exercise trials, it was noticed that while glucose levels remained relatively stable throughout the trials performed in the FS, these levels dropped during the PP trials (Figure 1). By the end of the trials, IG was still slightly higher in the PP state (127 vs 115mg/dL). No hypoglycaemia (≤70mg/dL) was detected throughout the exercise trials [20].
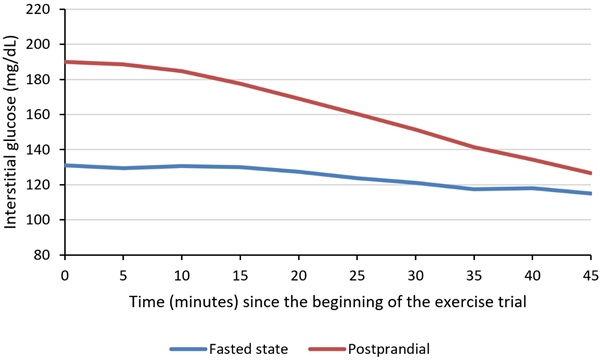 Figure 1: Average interstitial glucose level during exercise trials.
Figure 1: Average interstitial glucose level during exercise trials.
Capillary Glycaemia (CG): In the beginning of the trials, IG and CG were very similar, differing only 5.4%. After 25 minutes of exercise, that difference increased to 19.4%, with a much bigger difference in the PP trials (28.3% vs 10.6%). A similar difference (20.0%) was found after 45 minutes, also with a much greater difference in the PP trials (27.9% vs 12.1%) (Table 2). Also, comparing CG at 25 minutes with IG measured 5, 10 and 15 minutes later, we noticed that, during PP trials, that difference decreased over time (Table 3). Analysing the CG levels during the exercise (Figure 2), we noticed a stepper decrease in the CG when compared to the IG (Figure 1). These findings are suggestive of a lag in the IG evaluation when the CG is changing fast.
|
|
0min |
25min |
45min |
|||
|
|
mg/dL |
% |
mg/dL |
% |
mg/dL |
% |
|
Fasted state |
8.0±7.8 |
5.6±5.0 |
10.7±12.4 |
10.6±13.4 |
12.0±7.0 |
12.1±8.0 |
|
Postprandial state |
10.7±5.7 |
5.2±2.1 |
35.7±13.5 |
28.3±9.3 |
27.0±10.4 |
27.9±12.9 |
Table 2: Difference between interstitial glucose and capillary glycaemia on each stage of the exercise trials.
Data presented as mean ± standard deviation.
|
|
0min |
5min |
10min |
15min |
|
Fasted state |
10.6±13.4 |
10.4±12.8 |
11.6±10.4 |
8.6±8.8 |
|
Postprandial state |
28.3±9.3 |
21.1±7.8 |
13.2±4.1 |
7.6±2.7 |
Table 3: Difference between capillary glycaemia at 25 minutes of exercise and interstitial glucose 0, 5, 10 and 15 minutes later.
Data presented as mean ± standard deviation, in percentage.
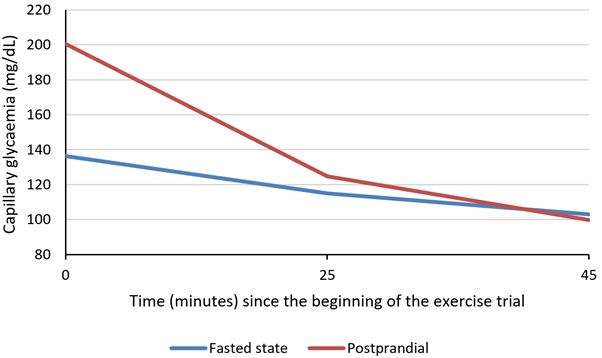 Figure 2: Average capillary glycaemia during exercise trials.
Figure 2: Average capillary glycaemia during exercise trials.
Ketones during exercise: All the capillary ketonemia tests showed levels of β-hydroxybutyrate under 0.2mmol/L.
DISCUSSION
To the best of our knowledge, this was the first time a protocol of this kind was applied to a patient with T2DM and CAD. In this very interesting field of investigation, there is still a lot to be understood regarding exercise and nutrition, still being unclear whether exercising in the fasted state is good for health or, especially in high risk populations, if there are special hazards to be considered.
Our recruited volunteer was a middle-aged man witha metabolic syndrome (T2DM, essential hypertension, dyslipidaemia and central obesity) and established CAD, representing not only a high percentage of the diabetic population, but also the kind of patient that would benefit the most from the additional advantages of fasted state exercise and, at the same time, would be at higher risk for cardiovascular complications. He was being treated with metformin, which doesn’t raise any high-risk alarms for hypoglycaemia, but that could lead to a faster glycaemic decline in both the PP and FS exercise trials.
The mild symptoms reported before the start of the FS trials were not accompanied by any abnormalities in the vital signs, glycaemia or ketonemia and disappeared after just a few minutes of exercise. Also, the changes in the BP throughout the exercise trials were as expected and there were no relevant findings in the EKG, suggesting probable safety of this practice.
Both IG and CG showed a stepper decrease in the PP state, which is probably related to the increased level of circulating insulin caused by the prior meal. The stability found in the FS trials is suggestive that, at least with this kind of therapy, there is no increased risk of hypoglycaemia while practicing moderate intensity aerobic exercise while fasting, at least during the first 45 minutes.
Despite the highly complex changes in the interstitial fluid during exercise and the known lag in the flash glucose monitoring system [21,22], the scarce existing evidence regarding the performance of these devices during exercise suggests a reasonable accuracy [23]. Our findings favour a 15-minute lag in the IG droppage when glycaemia is changing fast. The much lower differences between IG and CG found during FS trials suggests that lag is not related to the exercise itself, but rather to the fast glycaemia changes.
There was some concern that slowing the glucose usage by the muscle cells could result in increased ketone formation, but all the capillary ketonemia tests were negative, which means that either there was no considerable increase in such production or there was also increased consumption, not resulting in relevant accumulation.
These results favour the apparent safety and inferior glucose lowering effect of fasted state aerobic exercise, and also support the existence of a slight lag in the flash glucose monitoring when glycaemia levels are changing fast.
The major limitation of this study was the recruitment of only one patient so far. The major strengths of this study are: 1) the divulgation of an exercise protocol that could be used by other researchers; and 2) the inclusion of a high-risk patient with CAD and T2DM.
Further study is warranted in a longer-term trial with a greater number of participants.This protocol demonstrated the potential for success and could be applied in further studies to better understand the effect of FS exercise in patients with T2DM and CAD.
ACKNOWLEDGEMENTS
The authors gratefully thank the volunteer for his participation, Abbott for offering the FreeStyle Libre™ devices and Academia de Fitness do Estádio Universitário de Lisboa for providing the exercise room and cycle ergometer.
REFERENCES
- Zhou B, Lu Y, Hajifathalian K, J Bentham, M Di Riley, et al. (2008) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 387: 1513-1530.
- Aronson D, Edelman ER (2014) Coronary artery disease and diabetes mellitus. Cardiol Clin 32: 439-455.
- Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, et al. (2009) Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA 301: 2024-2035.
- Colberg SR, Albright AL, Blissmer BJ, Braun B, Chasan-Taber L, et al. (2010) Exercise and type 2 diabetes: American College of Sports Medicine and the American Diabetes Association: Joint Position Statement. Med Sci Sports Exerc 42: 2282-2303.
- Vanhees L, De Sutter J, GeladaS N, Doyle F, Prescott E, et al. (2012) Importance of characteristics and modalities of physical activity and exercise in defining the benefits to cardiovascular health within the general population: recommendations from the EACPR (Part I). Eur J Prev Cardiol 19: 670-686.
- Enevoldsen LH, Simonsen L, Macdonald I, Bülow J (2004) The combined effects of exercise and food intake on adipose tissue and splanchnic metabolism. J Physiol 561: 871-882.
- Gonzalez JT, Veasey RC, Rumbold PLS, Stevenson EJ (2013) Breakfast and exercise contingently affect postprandial metabolism and energy balance in physically active males. Br J Nutr 110: 721-732.
- Stannard SR, Buckley AJ, Edge JA, Thompson MW (2010) Adaptations to skeletal muscle with endurance exercise training in the acutely fed versus overnight-fasted state. J Sci Med Sport 13: 465-469.
- Van Proeyen K, Szlufcik K, Nielens H, Pelgrim K, Deldicque L, et al. (2010) Training in the fasted state improves glucose tolerance during fat-rich diet. J Physiol 588: 4289-4302.
- De Bock K, Derave W, Eijnde BO, Hesselink MK, Koninckx E, et al. (2008) Effect of training in the fasted state on metabolic responses during exercise with carbohydrate intake. J Appl Physiol 104: 1045-1055.
- Ardérius M, Alves M, Ardérius C, Jordão A (2018) Cardiovascular Exercise in the Fasted State in Healthy Young Adults?: Analysis of the Glycemic Profile. Rev Port Diabetes. 13: 14-17.
- Poirier P, Mawhinney S, Grondin L, Tremblay A, Broderick T, et al. (2001) Prior meal enhances the plasma glucose lowering effect of exercise in type 2 diabetes. Med Sci Sport Exerc 33: 1259-1264.
- Gaudet-Savard T, Ferland A, Broderick TL, Garneau C, Tremblay A, et al. (2007) Safety and magnitude of changes in blood glucose levels following exercise performed in the fasted and the postprandial state in men with type 2 diabetes. Eur J Cardiovasc Prev Rehabil. 14: 831-836.
- Hansen D, de Strijcker D, Calders P (2017) Impact of Endurance Exercise Training in the Fasted State on Muscle Biochemistry and Metabolism in Healthy Subjects: Can These Effects be of Particular Clinical Benefit to Type 2 Diabetes Mellitus and Insulin-Resistant Patients? Sport Med 47: 415-428.
- Terada T, Wilson BJ, Myette-Côté E, Kuzik N, Bell GJ, et al. (2016) Targeting specific interstitial glycemic parameters with high-intensity interval exercise and fasted-state exercise in type 2 diabetes. Metabolism 65: 599-608.
- Liepinsh E, Makrecka M, Kuka J, Makarova E, Vilskersts R, et al. (2014) The heart is better protected against myocardial infarction in the fed state compared to the fasted state. Metabolism 63: 127-136.
- Simonsen S, Kjekshus JK (1978) The Effect of Free Fatty Acids on Myocardial Oxygen Consumption During Atrial Pacing and Catecholamine Infusion in Man. Circulation 58: 484-491.
- Aird TP, Davies RW, Carson BP (2018) Effects of fasted vs fed-state exercise on performance and exercise metabolism: A systematic review and meta-analysis. Scand J Med Sci Sport. 28: 1476-1493.
- La Bounty PM, Campbell BI, Wilson J, Galvan E, et al. (2011) International Society of Sports Nutrition position stand: meal frequency. J Int Soc Sports Nutr 8: 4.
- American Diabetes Association (2017) Standards of Medical Care in Diabetes—2017: Summary of Revisions. Diabetes Care 40: 4-5.
- Moser O, Yardley J, Bracken R (2018) Interstitial glucose and physical exercise in type 1 diabetes: integrative physiology, technology, and the gap in-between. Nutrients 10.
- Fokkert MJ, Dijk PR Van, Edens MA, Abbes S, de Jong D, et al. Performance of the FreeStyle Libre Flash glucose monitoring system in patients with type 1 and 2 diabetes mellitus. BMJ Open Diabetes Res Care 5: 1-8.
- Giani E, Macedoni M, Barilli A, Petitti A, Mameli C, et al. (2018) Performance of the Flash Glucose Monitoring System during Exercise. Diabetes Res Clin Pract 146: 321-329.
Citation: Ardérius M, Gómez N, Alves M, Rodrigues A, Ardérius C, et al. (2020) Aerobic Exercise in the Fasted State for Type 2 Diabetic Patient with Coronary Artery Disease - Protocol and Case Report. J Clin Stud Med Case Rep 7: 078.
Copyright: © 2020 M Ardérius, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

