
Age Factor Influencing on Patients Subjected to Coronary Artery Bypass Grafting
*Corresponding Author(s):
Abdurakhmanov ZMDepartment Of General Surgery, Bukhara State Medical Institute, Bukhara, Uzbekistan
Tel:+998 907180051,
Email:z_abdurakhmanov@yahoo.com
Abstract
Objective: To study age-dependent trends in long-term survival with its predictors in patients who underwent isolated CABG.
Methods: 177 consecutive patients, operated on within 2014 were included in our study. The patients were divided into two age groups for the purposes of the statistical analysis: <60 year’s (????=96), and ≥60 years (????=81). The mean age was 54.5±2.9 year’s in the group of <60 years, whereas 63.6±2.5 in the ≥60 years. In both groups, the impact of the prevalence of comorbidities, severity of coronary lesion, revascularization degree (complete/incomplete) on postoperative outcome was assessed. Furthermore, the whole predictors of mortality were identified according to both age groups by means of multivariate analysis. End point of this study was overall survival. All data were obtained from patients’ medical, out-patient follow-up records, operative reports.
Results: The mean follow-up of the overall cohort was 5.1±1.7 years. Chronic pulmonary disease, extracardiac arteriopathy, and neurologic dysfunction disease were significantly less frequent in the group of <60 years, whereas the prevalence of BMI ≥30, unstable angina, previous myocardial infarction, and preoperative severe depressed left ventricular ejection fraction were significantly higher in this population. At 5 years follow-up, survival rate was 94.8% in patients under 60 years (5 patients), 90.1% (8 patients) in those aged 60 and more year’s (p<0.001). By multivariate analysis, previous myocardial infarction, chronic renal failure, diabetes, chronic pulmonary disease, extracardiac arteriopathy and left main coronary artery disease were considered as independent predictors of mortality. The area under the receiver operating characteristic curve was 0.834 (p<0.001, 95% CI: 0.724-0.902).
Conclusion: Despite the coronary artery bypass grafting are more secure for both groups, a strict attention should be focused in order to design and improve preventive strategies aiming to reduce the impact of specific cardiovascular risk factors on younger patients, such as diet, lifestyle, weight control and more aggressive medical therapy. The reasonable revascularization strategy with its underscored threshold for elderly patients with multivessel and left main coronary artery diseases, potential risk factors for death as concomitant pathologies should be elaborated.
Keywords
Coronary artery bypass grafting; Coronary artery disease; Multivessel disease
INTRODUCTION
Considering the increase in life expectancy of the world population in general in recent decades and the prevalence of cardiovascular diseases among the elderly, the percentage of this population who needs cardiovascular surgery is increasing, including those who have reached or exceeded the average life expectancy for Uzbekistanians (72 years of age) [1]. Meanwhile, major surgeries in elderly populations, such as cardiac surgeries (especially those 65 years of age or older), are associated with high morbidity and mortality, while aging simultaneously results in the reduction of functional reserves of various organs and systems [2]. The prevalence of other comorbidities among the elderly is high [3].
With regard to young patients, premature Coronary Artery Disease (CAD) is a rapidly progressive form of the disease [4]. Numerous studies reported that young patients with CAD have a significant prevalence of classic cardiovascular risk factors [5,6], and that the premature clinical onset of their symptoms can be more aggressive than in elderly patients [7]. In fact, young adults who undergo coronary artery revascularization are a specific subpopulation of patients, and there have been few studies on survival data, cardiovascular events [8]. Young patients undergoing Coronary Artery Bypass Grafting (CABG) demonstrate survival rates similar to those of Percutaneous Coronary Intervention (PCI), but lower rates of repeated revascularization [9]. There are few long-term reports of the impact of age stratification on CABG outcomes both for young and elderly patients.
The aim of our study was to investigate age-dependent trends in long-term survival with its predictors in patients who underwent isolated CABG.
METHODS
Within 2014, data of all patients undergoing coronary CABG in Republican Specialized Center of Surgery (Tashkent, Uzbekistan) were gathered. All data were obtained from patients medical, out-patient follow-up records, operative reports. The requirement for individual patient consent was waived because of the retrospective design of the study and because data were collected from routine care procedures. All data were anonymized and deidentified prior to statistical analysis.
Exclusion study criteria were emergency, cardiogenic shock, associated valve surgery procedures, major aortic surgery, and supra-aortic vessels disease requiring surgery. After these exclusions, we filtered 177 patients subjected to isolated CABG. The patients were divided into two age bands for the purposes of the statistical analysis: <60 years (????=96), and ≥60 years (????=81).
Decisions about the type of treatment were taken according to local practices and there were no standard regional protocols. The choice of CABG technique, performed either with the use of extracorporeal circulation or off-pump, was left to the surgeon’s discretion. Whenever possible, the left internal thoracic artery was used preferentially for revascularization of the Left Anterior Descending artery (LAD). Complete revascularization was performed with other arterial conduits, namely, radial artery or and saphenous vein grafts. Follow-up angiography was not performed routinely in either group of patients. All-cause death included overall mortality occurring during the index hospital admission or thereafter. Cardiac death was defined as any death due to a cardiac cause (e.g., Myocardial Infarction (MI), low output failure, and fatal arrhythmia), and other types were procedure-related death and death of unknown cause.
STATISTICAL ANALYSIS
Demographic and clinical features of the patients were presented as counts, percentages, and were compared between the two age classes, using the Chi-square test. Independent predictors of 5 years mortality risk were estimated using a stepwise multivariable Cox proportional hazards model. All the analyses were performed with SPSS version 22.0.
RESULTS
The entire study cohort showed that patient risk profiles differed significantly between the groups (Table 1). The prevalence of patients under 60 is 54.2% (96 of 177 patients). Patients over 60 show a significantly higher prevalence of baseline comorbidities. In particular, serum creatinine, diabetes, chronic pulmonary disease, systemic arterial hypertension, extracardiac arteriopathy, and neurologic dysfunction disease were significantly less frequent in this younger population (Table 1).
|
Patients characteristics |
<60 yrs (n=96)% |
≥60 yrs (n=81)% |
p |
|
|
Age |
54.5±2.9 |
63.6±2.5 |
<0.001 |
|
|
Male, n (%) |
82 (85.4) |
71 (90.1) |
<0.0001 |
|
|
BMI ≥ 30 kg/m2, n (%) |
24 (25) |
17 (20.9) |
<0.0001 |
|
|
Urgency, n (%) |
1(1) |
- |
=0.038 |
|
|
Unstableangina, n (%) |
15 (15.6) |
12 (14.8) |
<0.0002 |
|
|
III/IV CCS class, n (%) |
74 (77) |
67 (82.7) |
<0.0001 |
|
|
LVEF (%) |
51.3±6.5 |
51.1±6.5 |
=0.147 |
|
|
LV Dysfunction, n (%) |
Severe (EF 30-44%) |
19 (19.8) |
14 (17.3) |
=0.45 |
|
Moderate (EF 45-54%) |
41 (42.7) |
35 (45.6) |
||
|
Mild (EF≥55%) |
36 (37.5) |
28 (37.0) |
||
|
III/IV NYHA class, n (%) |
10 (10.4) |
9 (11.1) |
<0.001 |
|
|
Previousmyocardialinfarction, n (%) |
44 (45.8) |
35 (43.2) |
<0.0001 |
|
|
Serum creatinine ≥177 mmol/l, n (%) |
3 (3.1) |
5 (6.1) |
=0.037 |
|
|
Diabetes, n (%) |
18 (18.7) |
16 (21) |
<0.0001 |
|
|
SAH, n (%) |
64 (66.7) |
66 (81.5) |
=0.824 |
|
|
Chronicpulmonarydisease, n (%) |
1 (1) |
2 (2.5) |
<0.0001 |
|
|
Extracardiacarteriopathy, n (%) |
3 (3.1) |
5 (6.2) |
<0.0001 |
|
|
Neurologicaldysfunctiondisease, n (%) |
- |
2 (2,5) |
=0,048 |
|
|
Off-pump |
4 (4.2%) |
10 (12.3%) |
<0.001 |
|
|
Previous PCI |
1 (1) |
- |
<0.001 |
|
|
CPB time (min) |
93.98±23.72 |
88.81±16.67 |
=0.035 |
|
Table 1: Baseline characteristics and preoperative clinical data of patients according to different age classes.
BMI: Body Mass Index; CCS: Canadian Cardiovascular Society grading of angina pectoris; LVEF: Left Ventricular Ejection Fraction; NYHA: New York Heath Association; SAH: Systemic Arterial Hypertension; PCI: Percutaneous Coronary Intervention; LMCA: Left Main Coronary Artery; CPB: Cardiopulmonary Bypass
On the other hand, the prevalence of Body Mass Index (BMI) ≥30 Kg/m2, unstable angina, Previous Myocardial Infarction (PMI) was higher in the group of <60 year’s than in patients aged 60 and more year’s. Moreover, patients <60 reported more frequently a preoperative severe depressed Left Ventricular Ejection Fraction (LVEF), although this was not statistically significant (p=0.147). We found that coronary revascularization was performed off-pump more frequently in patients over 60, whereas patients under 60 received more frequently on pump total arterial revascularization (p<0.001) (Table 1).
Analysis of the coronaroangiography results showed that the most pronounced changes in the coronary bed were detected in patients over 60 years. Multivessel disease in patients of the latter group significantly prevailed over that of <60 years group. (96.3%, 89.6% respectively). Moreover, left main coronary artery disease was observed significantly 3,7 times more in patients over 60 (Figure 1).
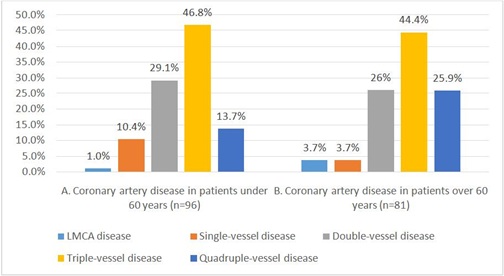
Figure 1: Coronaroangiography data (n=177).
According to the study data, patients of the both groups mostly experienced a triple-vessel disease. The latter disease was identified more often in both groups with concomitant diabetes (43.7% and 44.4% respectively). On top of that, a quadruple-vessel disease occurred in 25% patients of ≥60 years who had diabetes.
As shown in table 2, LAD was mostly exposed to atherosclerotic stenosis in both groups. Circumflex artery lesions were more often found in patients ≥60 years old in comparison to ≥60 years old, 17% and 12%, respectively, while right coronary artery lesions were more common in patients <60 years old compared to ≥60 years old, 11% and 8 %, respectively.
|
Coronary artery disease |
<60 yrs |
≥60 yrs |
p |
|
Total lesions (n=250) |
Total lesions (n=232) |
||
|
LAD, n (%) |
95 (31%) |
80 (34.5%) |
<0.001 |
|
DA, n (%) |
14 (4%) |
18 (7.7%) |
<0.001 |
|
Cx, n (%) |
29 (11.6%) |
40 (17.2%) |
<0.001 |
|
OM-1, n (%) |
36 (14.4%) |
28 (12%) |
<0.001 |
|
OM-2, n (%) |
2 (1%) |
4 (1.7%) |
<0.001 |
|
AI, n (%) |
11 (4.4%) |
8 (3.4%) |
<0.001 |
|
RCA, n (%) |
27 (10.8%) |
19 (8.1%) |
<0.001 |
|
PDA, n (%) |
36 (14.4%) |
35 (15%) |
<0.001 |
|
Complete arterial grafts revascularization, n (%) |
87 (90.6) |
68 (83.4) |
<0.0001 |
Table 2: Types and quantity of coronary artery disease.
LAD: Left Anterior Descending Artery; DA: Diagonal Artery; Cx: Circumflex artery; OM-1: Obtuse Marginal-1 artery; OM-2: Obtuse Marginal-2 artery; AI: Intermedia Artery; RCA: Right Coronary Artery; PDA: Posterior Descending Artery
Table 3 reports multivariate analysis with significant independent predictors of mortality at 5 years. The area under the receiver operating characteristic curve was 0,834 (P<0.001, 95% CI: 0.715-0.914).
|
Parameter |
HR |
95% CI of HR |
P |
|
|
<60 years old |
Previousmyocardialinfarction |
1.7 |
1.1-1.6 |
=0.0048 |
|
≥60 years old |
Serum creatinine ≥ 177 mmol/l |
2.5 |
1.5-3.2 |
<0.0002 |
|
Diabetes |
1.8 |
1.3-1.8 |
<0.0002 |
|
|
Chronic pulmonary disease |
2.1 |
1.3-2.5 |
<0.0005 |
|
|
Extracardiac arteriopathy |
1.9 |
1.4-2.1 |
<0.0001 |
|
|
LMCA disease |
2.7 |
1.2-4.4 |
=0.023 |
|
Table 3: Predictors for 5-year’s mortality risk (Cox proportional hazards model).
CI: Confidence Interval; HR: Hazard Ration; LMCA: Left Main Coronary Artery
As given in figure 2, despite the indication to operation, few patients of <60 (6.3%) and ≥60 (16%) did not undergo CABG due to multiple risk factors and severity of atherosclerotic disease, consequently ≥60 aged patients 9.7% less operated in comparison to the patients group of <60 (p<0.05). Besides complete revascularization was carried out in the group of ≥60 aged on 7.2 % less than in that of <60 (p<0.05).
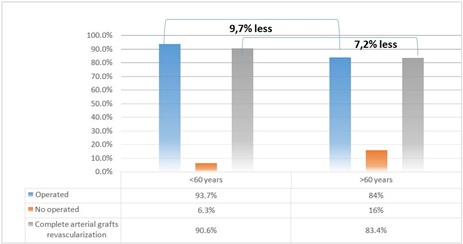
Figure 2: Percentage of operated/no operated patients, complete revascularization of both groups (n=177).
The mean follow-up of the overall cohort was 5.1±1.7 years. At follow-up, survival rate was 94.8 % in patients under 60 years (5 patients), 90.1% (8 patients) in those aged 60 and more years.
DISCUSSION
Recent studies conducted in Western Countries have found that the incidence of CAD has declined in the general population over the last few decades [10,11], probably due to better prevention of cardiovascular risk. On the other hand, the incidence of CAD, including acute coronary artery syndromes, among young to middle-aged adults has been shown to have increased [12]. Previous studies of CAD in young adults have mostly been single-center analyses [7,8], and few have been designed with the aim of studying young patients undergoing coronary revascularization [6,8,9,13-15].
The aim of our retrospective study was to investigate age-dependent trends in mortality in a population of patients undergoing isolated CABG. The main findings of this study are as follows. Of particular interest is that at 5 years the <60 group who underwent CABG reported unadjusted significantly lower long-term mortality than older patients (5.2% versus 9.9%).
It is well known that cardiovascular risk factors vary with regard to their impact on age of presentation with CAD. Our study confirms that patients younger than 60 have a different clinical pattern of presentation of CAD in comparison with elderly patients. Particularly, obesity, the history of previous myocardial infarction, the presence of depressed LVEF, and a history of previous PCI have been found to be highly prevalent among patients <60, confirming the results of a recent study by Moussa et al., [16]. Obesity has already been recognized as an independent risk factor for CAD [17] and recently a close association between severity of obesity, measured by BMI >30 kg/m2, and a progressive reduction in the mean age of patients with symptomatic CAD has been demonstrated [18]. In particular, abdominal obesity has been found to be closely associated with the risk of myocardial infarction [19] and this is observed more often in men [20,21]. On the basis of these observations and our results, it is reasonable to postulate that the risk of CAD due to obesity may be higher in men than women. On the other hand, systemic comorbidities usually associated with severe CAD, such as chronic pulmonary disease, diabetes, stroke, and extracardiac arteriopathy in our study, proved to be less frequent in patients aged <60. This is consistent with the previous international literature [22,23] and may be explained by the fact that the onset of diabetes mellitus and systemic hypertension usually occurs later in life, and their effect on the pathogenesis of CAD may require several years or decades to become clinically evident. Obviously, in terms of our data, the accumulation of these concomitant pathologies explains the higher rate of off-pump bypass grafting in elderly group. The purpose of this study was not to primarily investigate the risk factors determining premature CAD, but our findings clearly confirm that the pathogenesis of coronary artery disease remains complex and that both genetic and environmental factors contribute to the early onset of coronary artery disease.
Long-term mortality was considerably lower in patients <60 years than in patients ≥60, and this result is consistent with mortality rates reported in previous studies of young patients undergoing CABG [9,12,16,24].
In fact, in our study multivariate analysis confirmed that all classic clinical cardiac conditions and systemic comorbidities (history of previous myocardial infarction in the younger group, whereas, chronic renal failure, diabetes, chronic pulmonary disease, extra-cardiac arteriopathy, and left main coronary disease in the elderly group) are independent risk factors for mortality at 5 years.
The significantly lower rate of extracardiac arteriopathy reported in younger patient subgroups may also partly explain the significantly better stroke rates in patients under 60.
Of particular interest is that multivessel disease in patients of the ≥60 years group significantly prevailed over that of <60 years group that coincides with previous study [25]. Basing on our data results, ≥60 aged patients were conducted CABG 9.7% less in comparison to the patients’ group of <60. This may be explained by the fact that the incidence of significant arterial calcification increases with age, raising the complexity of operation [26]. Due to severe diffuse coronary lesion, incomplete revascularization was higher in ≥60 years group that may consistent with a lower survival rate as demonstrated in the latest study [27].
CONCLUSION
To conclude, CABG is safe and effective for both groups. Nevertheless, to increase the durability (considering not only the survival rates, but also the influence of the outcomes of surgery on quality of life) of myocardial revascularization, a strict attention should be focused in order to design and improve preventive strategies aiming to reduce the impact of specific cardiovascular risk factors on younger patients, such as diet, lifestyle, weight control, and more aggressive medical therapy. On top of that more often elderly patients are not capable of being operated due their complicated coronary anatomy that induces us to work out the strategy and borderline of the need for surgery. The reasonable revascularization strategy, with its underscored threshold for elderly patients with multivessel and left main coronary artery diseases, concomitant pathologies determined as potential risk factors for death, should be also elaborated.
REFERENCES
- Knoema (2017) The state committee of the Republic of Uzbekistan on statistics. Knoema, Tashkent, Uzbekistan.
- Lakatta EG, Levy D (2003) Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part II: the aging heart in health: links to heart disease. Circulation 107: 346-354.
- Oskvig RM (1999) Special problems in the elderly. Chest 115: 158-164.
- Klein LW, Nathan S (2003) Coronary artery disease in young adults. Journal of the American College of Cardiology 41: 529-531.
- Zimmerman FH, Cameron A, Fisher LD, Ng G (1995) Myocardial infarction in young adults: Angiographic characterization, risk factors and prognosis (coronary artery surgery study registry). J Am Coll Cardiol 26: 654-661.
- Mukherjee D, Hsu A, Moliterno DJ, Lincoff AM, Goormastic M, et al. (2003) Risk factors for premature coronary artery disease and determinants of adverse outcomes after revascularization in patients < or =40 years old. Am J Cardiol 92: 1465-1467.
- Cole JH, Miller JI 3rd, Sperling LS, Weintraub WS (2003) Long-term follow-up of coronary artery disease presenting in young adults. J Am Coll Cardiol 41: 521-528.
- Khawaja FJ, Rihal CS, Lennon RJ, Holmes DR, Prasad A (2011) Temporal trends (over 30 years), clinical characteristics, outcomes, and gender in patients ≤50 years of age having percutaneous coronary intervention. Am J Cardiol 107: 668-674.
- Biancari F, Gudbjartsson T, Heikkinen J, Anttila V, Mäkikallio T, et al. (2014) Comparison of 30-day and 5-year outcomes of percutaneous coronary intervention versus coronary artery bypass grafting in patients aged≤50 years (the Coronary aRtery diseAse in younG adultS Study). Am J Cardiol 114: 198-205.
- Ford ES, Capewell S (2007) Coronary heart disease mortality among young adults in the U.S. from 1980 through 2002: concealed leveling of mortality rates. J Am Coll Cardiol 50: 2128-2132.
- Nedkoff LJ, Briffa TG, Preen DB, Sanfilippo FM, Hung J, et al. (2011) Age- and sex-specific trends in the incidence of hospitalized acute coronary syndromes in Western Australia. Circ Cardiovasc Qual Outcomes 4: 557-564.
- Agarwal S, Sud K, Thakkar B, Menon V, Jaber WA, et al. (2017) Changing Trends of Atherosclerotic Risk Factors Among Patients with Acute Myocardial Infarction and Acute Ischemic Stroke. Am J Cardiol 119: 1532-1541.
- Flather M, Rhee JW, Boothroyd DB, Boersma E, Brooks MM, et al. (2012) The effect of age on outcomes of coronary artery bypass surgery compared with balloon angioplasty or bare-metal stent implantation among patients with multivessel coronary disease. A collaborative analysis of individual patient data from 10 randomized trials. J Am Coll Cardiol 60: 2150-2157.
- Lichtman JH, Wang Y, Jones SB, Leifheit-Limson EC, Shaw LJ, et al. (2014) Age and sex differences in inhospital complication rates and mortality after percutaneous coronary intervention procedures: evidence from the NCDR(®).Am Heart J 167: 376-383.
- Kaneko H, Yajima J, Oikawa Y, Tanaka S, Fukamachi D, et al. (2014) Impact of aging on the clinical outcomes of Japanese patients with coronary artery disease after percutaneous coronary intervention. Heart Vessels 29: 156-164.
- Moussa ID, Klein LW, Shah B, Mehran R, Mack MJ, et al. (2013) Consideration of a new definition of clinically relevant myocardial infarction after coronary revascularization: an expert consensus document from the Society for Cardiovascular Angiography and Interventions (SCAI). J Am Coll Cardiol 62: 1563-1570.
- Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB, et al. (2014) Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1·8 million participants. Lancet 383: 970-983.
- Atique SM, Shadbolt B, Marley P, Farshid A (2016) Association between Body Mass Index and Age of Presentation with Symptomatic Coronary Artery Disease. Clin Cardiol 39: 653-657.
- Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, et al. (2004) Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 364: 937-952.
- See R, Abdullah SM, McGuire DK, Khera A, Patel MJ, et al. (2007) The association of differing measures of overweight and obesity with prevalent atherosclerosis: the Dallas Heart Study. J Am Coll Cardiol 50: 752-759.
- Matsis K, Holley A, Al-Sinan A, Matsis P, Larsen PD et al. (2017) Differing Clinical Characteristics between Young and Older Patients Presenting with Myocardial Infarction. Heart Lung Circ 26: 566-571.
- Choudhury L, Marsh JD (1999) Myocardial infarction in young patients. American Journal of Medicine 107: 254-261.
- Reibis R, Treszl A, Wegscheider K, Bestehorn K, Karmann B, et al. (2012) Disparity in risk factor pattern in premature versus late-onset coronary artery disease: A survey of 15,381 patients. Vasc Health Risk Manag 8: 473-481.
- Dalén M, Ivert T, Holzmann MJ, Sartipy U (2015) Coronary artery bypass grafting in patients 50 years or younger: a Swedish nationwide cohort study. Circulation 131: 1748-1754.
- Posenau JT, Wojdyla DM, Shaw LK, Alexander KP, Ohman EM, et al. (2017) Revascularization Strategies and Outcomes in Elderly Patients with Multivessel Coronary Disease. Ann Thorac Surg 104: 107-115.
- Newman AB, Naydeck BL, Sutton-Tyrrell K, Feldman A, Edmundowicz D, et al. (2001) Coronary artery calcification in older adults to age 99: prevalence and risk factors. Circulation 104: 2679-2684.
- Diegeler A, Börgermann J, Kappert U, Hilker M, Doenst T, et al. (2019) Five-Year Outcome After Off-Pump or On-Pump Coronary Artery Bypass Grafting in Elderly Patients. Circulation 139: 1865-1871.
Citation: Adilova IG, Salomova AF, Abdurakhmanov ZM (2020) Age Factor Influencing on Patients Subjected to Coronary Artery Bypass Grafting. J Angiol Vasc Surg 5: 038.
Copyright: © 2020 Adilova IG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

