
An Overview of the Role of Cerclage in the Prevention of Spontaneous Preterm Birth
*Corresponding Author(s):
Christopher A EnakpeneDivision Of Maternal Fetal Medicine, Department Of Obstetrics And Gynecology, Texas Tech University Health Sciences Center, 701 W. 5th Street, Suite 3212, Odessa, Texas 79763, Texas, United States
Tel:+1 3472175127,
Email:christopher.a.enakpene@ttuhsc.edu
Abstract
Premature cervical ripening; cervical shortening and /or dilatation is one of the three pronged processes (cervical remodeling, membranes reactivation and uterine contractility) linked to the etiopathogenesis of preterm birth. Short Cervical Length (CL) <25 mm is the strongest predictor of spontaneous Preterm Birth (PTB). Many interventions such as bed rest and vaginal progesterone have been tried to remedy this situation, but only the cerclage has been proven to improve the mechanical and functional length of the cervix thereby contributing to PTB reduction. However, cerclage is not a fit for all clinical situations, as it does not significantly reduce the rate of PTB in history-indicated cervical shortening alone or in twin pregnancies with or without short cervix except if associated with CL <15 mm and / or cervical dilatation >10 mm. Using cerclage in addition to clinically indicated vaginal progesterone or 17 alpha-hydroxyprogesterone caproate have also demonstrated proven benefits. Cervical “restoration” with vaginal pessaries, on the other hand, in the prevention of PTB is controversial due to mixed results. There are additional proven benefits when women with cerclage receive adjuvant Indomethacin and / or antibiotics in reducing PTB. In this narrative review, we reappraise the role of cerclage in the prevention of sPTB in various clinical scenarios.
Keywords
Arabin pessary; Cerclage; Preterm delivery; Short cervix; Singleton; Twins
INTRODUCTION
Preterm Birth (PTB) is the number one cause of neonatal morbidity and mortality worldwide, and a leading cause of long-term childhood disability in the United States [1-3]. Globally, approximately 15 million babies per year are born preterm, which are more than 1 in 10 births [4]. Prior history of preterm birth and short Cervical Length (CL) <25 mm in index pregnancy are the strongest predictors of spontaneous Preterm Birth (sPTB) [5-8]. The role of increased uterine contractility has been the focus as the etiology of preterm birth, but emerging evidence suggests that premature ripening of the uterine cervix plays a significant role [9,10]. PTB processes can be initiated by any or a combination of the following: increased uterine contractility, premature cervical ripening characterized by cervical shortening and dilatation and activation of the decidua-fetal interface resulting in Preterm Premature Rupture of Fetal Membranes (PPROM) [11]. Several interventions have been implemented to decrease PTB such as 17-alpha hydroxyprogesterone caproate, various formulations of vaginal progesterone, pessary including Arabin pessary and cervical cerclage. Among all the various preventive measures of PTB, cerclage has been in use for more than a century and it has evolved over time as one of the most valuable interventions. Cerclage can be placed via the vaginal or transabdominal route, and the primary objective is to reinforce the cervix at the level of the internal os, thereby increasing the functional length of the cervix and strengthening the cervical canal. The transabdominal cerclage is usually reserved for patients with cervical tissues deficiency following trachelectomy or multiple cervical conizations for treatment of cervical dysplasia, and history of failed transvaginal cervical cerclage.
METHODS
A thorough literature search of published articles from 1957 in English language using the MeSH was done. We searched MEDLINE, PubMed and Cochrane Central Register of Controlled Trials (CENTRAL) of relevant articles. The MeSH search as done; (Cervical OR cervix OR “cervical ripening” [mh] OR “cervical ripening” [tw] OR ‘cervix uteri” [tw] OR “short cervix” OR “cervical length measurement” [mh] OR “cervical length measurement” OR “cervical cerclage” [mh] “cerclage” OR “anatomy scan” OR “anatomy scan” OR “level 2 ultrasound” OR “level II ultrasound” OR “basic ultrasound” OR “level two ultrasound”). We included all relevant randomized controlled trials, prospective and retrospective cohort studies, case series, systematic review, and meta-analysis on the subject matter. Approximately 159 articles were identified but only 46 were eligible for inclusion in this literature review.
INDICATIONS OF CERCLAGE
There are three main indications for cervical cerclage: [12]
History-indicated cerclage is for patients who had cervical incompetence in previous pregnancy, and it is characterized by: 1) recurrent midtrimester pregnancy loses, 2) history of painless second trimester cervical dilatation with or without pregnancy loss and 3) history of preterm premature rupture of fetal membranes prior to 34 weeks.
Ultrasound-indicated cerclage is when cerclage is placed for transvaginal ultrasound measurement of CL <25 mm in women with prior history of sPTB, or for extremely short CL <10 mm with or without vaginal progesterone for incidental short cervix. Physical examination in index pregnancy showing painless asymptomatic cervical dilation in the second trimester with or without bulging fetal membranes. This premature cervical dilatation in women without uterine contractions is otherwise called physical-exam indication [12]. Owen et al., demonstrated that in women with prior spontaneous preterm birth less than 34 weeks and CL <25 mm, cerclage reduced previable birth and perinatal mortality but did not prevent sPTB <35 weeks, unless CL was <15 mm at midtrimester [5]. Comparison of cervical cerclage with no cerclage in women with singleton gestation with CL <25 mm without prior preterm birth did not show any difference in the rates of sPTB, but cerclage was found to be efficacious at lower CLs, such as <10 mm, and when tocolytics or antibiotics were used as additional therapy [13].
MODERN MANAGEMENT OF SHORT CERVIX
There are multiple disease mechanisms that interact to manifest as short cervix and preterm birth syndrome. Most preterm births are spontaneous and CL screening is one tool that can be utilized to identify women at increased risk who may benefit from preventive interventions [14]. Transvaginal ultrasounds have become the gold standard test for the diagnosis of short cervix because it allows evaluation of both the internal and external cervical os in a sagittal long-axis view. Cervical length measurement in the midtrimester qualifies as a secondary level of prevention of PTB because it helps to identify at-risk patients. There is a growing body of evidence that suggests appropriate intervention in women with short cervix reduces the rate of PTB and improves overall perinatal outcomes. The treatment modalities are often influenced by the patient’s obstetric history, the number of fetuses, the prevailing clinical conditions and the degree of severity of cervical shortening. Therefore, interventions to prevent or treat short cervix should target many of these multiple disease mechanisms and interactions using a multi-modal approach in order to improve perinatal outcomes.
PATIENTS WITH PREVIOUS SPTB OR MIDTRIMESTER PREGNANCY LOSS
Recurrent PTB occurs in 50 - 60% of women with prior sPTB [15]. There is also an increased risk of sPTB in women with prior history of mid-trimester pregnancy losses or cervical incompetence. The American College of Obstetricians and Gynecologists (ACOG) and Society for Maternal-Fetal Medicine (SMFM) recommend that these women should be started on weekly doses of 17- alpha hydroxyprogesterone at 16 - 20 weeks and continue until 36 weeks [16,17]. In addition, serial CL measurement should be done every 1 - 2 weeks as determined by the clinical situation from 16 weeks to 24 weeks [17]. Women who develop short cervix with CL <25 mm prior to 24 weeks with or without 17-OHPC should have cervical cerclage, as shown in the graphic description of cerclage in figure 1. In one study, only 40% of women with singleton pregnancy with prior sPTB developed short CL <25 mm before 24 weeks, while 60% did not have short cervix [18]. Hence, placing prophylactic cerclage by the virtue of prior PTB will unnecessarily increase the number of patients who have cerclage even though they do not need it. In a large trial by Owen et al., of 302 women with prior sPTB between 16 and 34 weeks (mean GA of 24 weeks) and CL <25 mm who were randomized to cerclage versus no cerclage, cerclage was associated with significant reduction of recurrent PTB <37 weeks at 45% versus 60% and <24 weeks was 6.1% versus 14%. Cerclage was also associated with significant reduction in perinatal death, 8.8% versus 16% in women without cerclage [5].
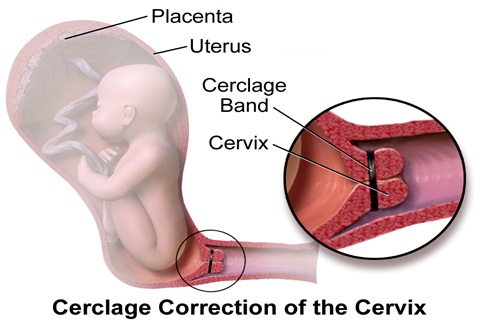
Figure 1: Images of graphic description of cervical cerclage.
The strongest evidence comes from meta-analysis of individual patient-level data derived from 5 Randomized Controlled Trial (RCT) which consisted of 504 women (250 women in the cerclage group) by Berghella et al., in 2011. In this meta-analysis, cervical cerclage reduced PTB <37 weeks by 30% and composite perinatal morbidity and mortality by 36%, and 20 cerclages were needed to prevent one perinatal death [8].
CERCLAGE IN WOMEN WITH INCIDENTAL SHORT CERVIX
Vaginal progesterone is the recommended treatment in women with short cervix with no prior sPTB or second trimester pregnancy loss. The ACOG and the SMFM recommend vaginal progesterone for women with incidental short cervix, CL <20 mm but more >10 mm [17]. The current available evidence does not support cerclage placement in women with sonographic short cervix without history of sPTB. In a meta-analysis of 4 RCT that included 607 of unselected women with asymptomatic short cervix <25 mm on ultrasound (305 women with cerclage and 302 women without cerclage), cerclage did not significantly prevent PTB, 29.2% versus 34.8%, (RR 0.84, 95% CI 0.67- 1.06, p = 0.29) [7]. However, in a planned subgroup analysis of singleton pregnant patients in this study, cerclage reduced sPTB < 35 weeks by 26%, (RR 0.74, 95% CI 0.51 – 0.96) [7]. Similarly, cerclage also reduced PTB <35 weeks in singleton pregnant women with prior sPTB (RR 0.61, 95% CI 0.40 - 0.92), and in singleton gestations with prior second trimester loss (RR 0.57, 95% CI 0.33 - 0.99). In regards to twin gestation in this study, cerclage significantly increased the rate of PTB < 35 weeks, (RR 2.15, 95% CI 1.15 - 4.01). Despite some promising benefits of cerclage as shown in table 1, there is presently still insufficient evidence to recommend cerclage in all singleton pregnant patients with asymptomatic sonographic short cervix without prior sPTB [12]. However, incidental short cervix should be treated differently in similar patients with sonographic acute painless cervical dilatation and effacement in whom emergency cerclage is appropriate.
|
Authors, year |
Study type, N, End result |
Inclusion criteria
|
Cerclage n (%) |
No cerclage n (%) |
OR, or RR 95% CI |
P value |
|
Althuisius, 2001. CIPRACT 1 |
RCT, 35 sPTB <35
|
Prior sPTB <34, CL <25 mm |
n = 19 0 (0) |
n = 16 7 (43.8) |
|
0.002 |
|
Althuisius, 2003 CIPRACT II |
RCT, 23 sPTB <34 |
Dilated cervix & bulging membranes |
n = 13 7 (53.8) |
n = 10 10 (100) |
|
0.02 |
|
Berghella, 2004, UIC |
RCT, 61 sPTB <35 |
CL <25 mm |
n = 31 14 (45.2) |
n = 30 14 (47.6) |
0.94 (0.34-2.58) |
0.91 |
|
Berghella, 2005 IPD |
SR & MA, 607, sPTB <35 |
All women with CL <25 mm |
n = 305 89 (29.2) |
n = 302 105 (34.8) |
0.84 (0.71-0.99) |
0.29 |
|
Owen, 2009 Multicenter Study |
RCT, 301 sPTB <35 |
Prior sPTB <34 weeks. CL <25 mm. |
n = 148 48 (32) |
n = 153 64 (42) |
0.67 (0.42-1.09) |
0.09 |
|
Owen, 2009 Subgroup analysis |
RCT, 64 sPTB <35 |
Prior sPTB <34 weeks. CL <15 mm |
|
|
0.23 (0.08-0.66) |
0.006 |
|
Nicolaides, 2016 Pessary |
RCT, 932 sPTB <34 |
Short cervix CL <25 mm |
n = 465 (12.0) |
n = 467 (10.8) |
1.12 (0.75-1.69) |
0.57 |
|
Alfirevic, 2017 Cochrane |
SR, 2415, sPTB <37, 34 |
High risk for sPTB |
|
|
0.77 (0.66-0.89) |
|
|
Berghella, 2017 IPD |
SR & MA, 419 sPTB <35 |
Incidental CL <25 mm in singleton |
n = 224 49 (21.7) |
n = 195 54 (27.7) |
0.9 (0.63-0.89) |
|
|
Berghella, 2017 Subgroup analysis |
SR & MA 126 sPTB <35 |
Incidental short CL <10 mm |
n = 76 30 (39.5) |
n = 50 29 (58.0) |
0.68 (0.47-0.98) |
|
|
Dugoff, 2018 Pessary |
RCT, 122 sPTB <37 |
No sPTB CL <25 mm |
n = 61 23 (38.3) |
n = 61 20 (32.8) |
1.17 (0.72-1.19) |
0.59 |
|
Enakpene, 2018 |
RCS, 75 sPTB <37 |
On vaginal progesterone, CL < 10 mm |
36 15 (44.1) |
39 32 (84.2) |
0.52 (0.35-0.78) |
0.001 |
|
Li, 2019 |
MA, 1211 |
<15 mm |
n = 79 60 (75.9) |
n = 75 67 (89.3) |
0.86 (0.74-0.99) |
0.040 |
Table 1: Studies of cervical cerclage in women with singleton pregnancy at increased risk of spontaneous preterm birth.
sPTB: Spontaneous Preterm Birth, CL: Cervical Length; SR: Systematic Review, MA: Meta-Analysis, RCS: Retrospective Cohort Study, UIC: Ultrasound-Indicated Cerclage, N: Number of cases in the study
WOMEN WITH INCIDENTAL EXTREME SHORT CERVIX <10 MM
The risk of cervical dilatation and ascending infection is higher when CL <15 mm [5]. Women with extreme short CL <10 mm have been shown to benefit more from cerclage than vaginal progesterone alone; (Figure 2). Some patients develop progressively worsening short cervix <10 mm despite being on daily vaginal progesterone, or are diagnosed at first CL assessment with TVUS with short cervix, CL <10 mm. Unfortunately, vaginal progesterone has been found to be less effective in this category of patients. Hence, cervical cerclage is recommended in women with extreme short cervix <10 mm. In an Individual Patient Data (IPD) meta-analysis and systematic review by Berghella et al., in 2017, cervical cerclage was significantly more effective (39.5% versus 58.0%) than vaginal progesterone in patients with CL <10 mm (RR 0.68, 95% CI 0.47 - 0.98) [13]. Similarly, Enakpene et al., in their study of singleton pregnant women with short cervix on vaginal progesterone who develop progressively shortening CL <10 mm, cerclage in combination with vaginal progesterone compared to vaginal progesterone alone was more effective in the reduction of sPTB (RR 0.52, 95% CI 0.35 - 0.78, p = 0.001). Pregnancy was also more prolonged in the combined group; 14 weeks versus 7 weeks with associated reduction of overall adverse perinatal outcomes [19]. The positive outcomes of this study make serial CL surveillance in patients on vaginal progesterone for incidental short cervix a practice to be considered so that appropriate intervention can be promptly instituted. Individual institution should be discretional in adopting this practice because it will increase the number of clinic visits, workload for the healthcare staff as well as economic burden. However, the beneficial effect of prevention of one single preterm birth may quite outweigh the burden of having extremely premature babies in the neonatal intensive care unit, and its accompanied complications and sequelae.
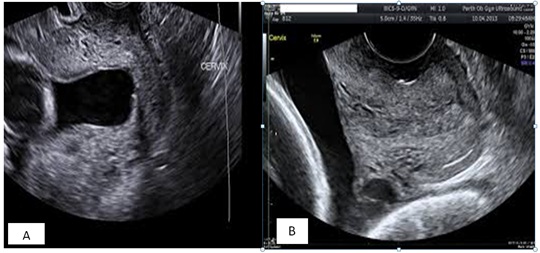 Figure 2: Pre-cerclage (A) and post-cerclage (B) cervical images of patient with CL <10 mm.
Figure 2: Pre-cerclage (A) and post-cerclage (B) cervical images of patient with CL <10 mm.
Ultrasound images of the cervix before cerclage, and two weeks after cerclage placement.
MULTIPLE PREGNANCY WITH INCIDENTAL SHORT CERVIX
Management of short cervix in women with multiple pregnancies who have no history of sPTB poses serious dilemmas due to mixed outcomes associated with interventions to prevent PTB. Use of daily vaginal progesterone has been tried without proven benefits. In an IPD metaanalysis by Romero et al., in 2012, the use of vaginal progesterone in women with short cervix did not significantly reduce sPTB among subgroup analysis involving 52 women with twin pregnancy, (RR 0.70, 95% CI 0.34 - 1.44), but it significantly decreased the risk of composite neonatal morbidity and mortality, (RR 0.52, 95% CI 0.29 - 0.93) [20]. This was supported by another IPD metaanalysis by Schuit et al., in 2015 which included 13 trials consisting of 3768 women with twin pregnancy and incidental short cervix. It showed that vaginal progesterone did not reduce sPTB <32 weeks of gestation (RR 0.91, 95% CI 0.68 - 1.2) or reduce adverse perinatal outcomes (RR 0.97, 95% CI 0.77 - 1.2) [21]. The role of cervical cerclage in the reduction of PTB in twin pregnancy is debatable with mixed outcomes as shown in table 2. In a study by Roman et al., of 76 twin pregnancies with dilated cervix of 10 - 45 mm before 24 weeks, cerclage, indomethacin, and antibiotics significantly prolonged pregnancy from diagnosis to delivery by 10.5 + 5.6 weeks versus 3.7 + 3.2 weeks, (mean difference 6.7 weeks, 95% CI 4.71 -8.81), decreased sPTB rate <34 weeks, 52.6% versus 94.7% (aOR 0.06, 95% CI 0.03 - 0.34, p < 0.001) [22] and decrease perinatal mortality, 27.6% versus 59.2%, (aOR 0.24, 95% CI 0.11 -0.5, p < 0.001) when compared with expectant management. In a prior study by Roman et al., of 140 twin pregnancies with asymptomatic short cervix, CL <25 mm at 16 - 24 weeks, cerclage did not significantly reduce PTB <28 weeks, 21.2% versus 24.1%, (aOR 0.3, 95% CI 0.68 - 1.37); <32 weeks, 38.6% versus 43.4%, (aOR 0.34, 95% CI 0.1 - 1.13), and <34 weeks, 50.9% versus 63.9%, (aOR 0.37, 95% CI 0.16 - 1.1). Among these women with <25 mm, cerclage also did not prolong pregnancy when compared with no cerclage group [23]. However, in a subgroup analysis of women in this study with CL <15 mm, cerclage significantly decreased sPTB <34 weeks, 50% versus 79.5%, (aOR 0.51, 95% CI 0.31 - 0.83), and also prolonged pregnancy by 12.5 ± 4.5 versus 8.8 ± 4.6 weeks, p <0.001 respectively, and admission to NICU, 65.5% versus 82.9%, (aOR 0.42, 95% CI 0.24 - 0.81) [23].
|
Authors, year |
Study type Sample size End results |
Inclusion criteria |
Cerclage n (%) |
No cerclage n (%) |
OR, or RR 95% CI |
P value |
|
Saccone, 2015 IPD |
SR & MA 49, sPTB <34 |
Incidental CL <25 mm |
n = 24 15 (62.5) |
n = 25 6 (24) |
2.19 (0.72 - 6.63) |
|
|
Roman, 2015 UIC |
RCS 140 sPTB <34 |
Asymptomatic CL <25 mm, 16 - 24 weeks |
57 29 (50.9) |
83 53 (63.9) |
0.37 (0.16 - 1.1) |
|
|
Roman, 2015 Subgroup Analysis, UIC |
RCS 71, sPTB <34 |
CL <15 mm 16 - 24 weeks |
32 16 (50) |
39 31 (79.5) |
0.51 (0.31 - 0.83) |
|
|
Roman, 2016 Cerclage < 24 weeks |
RCS 76, sPTB <34 |
Dilated cervix >10 mm 16 - 24 weeks |
n = 38 20 (52.6) |
n = 38 36 (94.7) |
0.06 (0.03 - 0.34) |
<0.001 |
|
Abassi, 2018 Cerclage < 25 weeks |
RCS 36, sPTB <34 |
Dilated cervix >10 mm
|
n = 27 18 (66.7) |
n = 9 9 (100) |
|
0.046 |
|
Adams, 2018 Mean GA of cerclage 20.8 weeks |
RCS Unselected 82 women, sPTB <35 |
CL <25 mm before 24 weeks |
n = 43 15 (34.9) |
n = 39 19 (48.7) |
0.72 (0.38 - 1.36) |
0.260 |
|
Adams, 2018 Ssubgroup analysis |
RCS |
CL <15 mm |
(37) |
(71.4) |
0.49 (0.26 - 0.93) |
0.020 |
|
Han, 2019 History of sPTB |
RCS 135, sPTB <32 |
CL <25 mm, and / or dilated cervix >10 mm |
96 10 (10.4) |
39 11 (28.2) |
0.23 (0.08 - 0.70) |
0.017 |
Table 2: Studies of cervical cerclage in women with twin pregnancy with increased risk of spontaneous preterm birth.
sPTB: Spontaneous Preterm Birth, CL: Cervical Length; SR: Systematic Review, MA: Meta-Analysis, RCS: Retrospective Cohort Study, UIC: Ultrasound-Indicated Cerclage.
In addition, metaanalysis from 16 studies by Li et al., of 1211 women elucidated the benefits of cerclage in twin pregnancy. In their review, they concluded that cerclage was more beneficial in prolonging pregnancy and reducing sPTB <37 weeks among women with CL <15 mm or cervical dilatation >10 mm. Among women with CL <15 mm, sPTB rate <37 weeks was decreased; (risk ratio of 0.86, 95% CI 0.74 - 0.99, p <0.001) and pregnancy was prolonged with mean difference of 3.89 weeks of gestation, (95% CI, 2.19 - 5.59, P <0.001) [24]. However, there was no significant benefit in twin pregnancies who had history-indicated or twin alone indicated cerclage [25].
MULTIPLE PREGNANCY WITH PRIOR SPTB OF SINGLETON PREGNANCY
Unlike in singleton pregnancy, the use of weekly 17-alpha OHPC prophylaxis from 16 - 36 weeks in women with prior singleton sPTB who are now carrying twin pregnancy has not been proven to be effective in preventing recurrence of PTB. Some experts have suggested the use of pessary in combination with vaginal progesterone long before they develop short cervix, but this is not supported by any scientific evidence. There is no consensus on whether cervical cerclage reduces the rate of PTB in women with twin pregnancy with prior history of singleton sPTB who develop short cervix. However, in a study by Han et al., of 135 women with twin pregnancy with history of sPTB, who had CL <25 mm and / or cervical dilation ≥10 mm, cerclage reduced the rate of recurrent PTB <32 weeks of gestation compared to no cerclage, 10.4% versus 28.2%, (OR 0.23, 95% CI 0.08 - 0.70, p = 0.017) [25].
Adams et al., showed that in an unselected 82 pregnant women with twins and CL <25 mm with or without prior preterm birth, cerclage did not significantly reduce sPTB <35 weeks when compared to women without cerclage, 34.9% versus 48.7%, (aRR 0.72, 95% CI 0.38 - 1.36, p = 0.260). Subgroup analysis of patients with CL <15 mm, cerclage reduced sPTB rate <35 weeks by almost 50%; 37% versus 71.4%, (aRR 0.49, 95% CI 0.26 - 0.93, p = 0.020) [26].
PATIENTS WITH EXPOSED MEMBRANES
Exposed fetal membranes are often a great challenge because of fear of inadvertent rupture of the membranes, as shown in figure 3. There is also potential risk of infection due to fetal membranes exposed to vaginal flora. Hence, various interventions such as antibiotic prophylaxis and the use of a Foley balloon to push the fetal membranes cephalad before placing a cervical cerclage have been shown to reduce the occurrence of these complications.
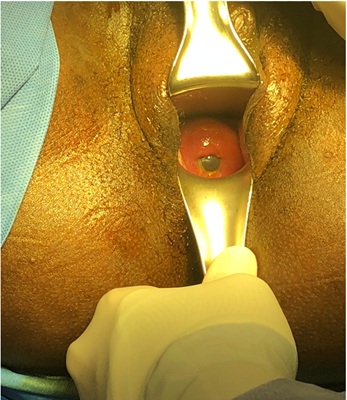
Figure 3: Exposed fetal membranes in extremely shortened cervix.
Foley catheter with balloon inflated to 10 - 30 mL can be used to push the fetal membranes into the uterine cavity before placing a cerclage suture.
Antibiotic prophylaxis
The use of antibiotics prior to cerclage insertion in patients with exposed fetal membranes has been shown to be effective in reducing preterm birth. In the subgroup analysis of IPD by Berghella et al., showed that the rate of preterm birth was lower in patients who receive prophylactic antibiotics, 18.3% versus 31.5%; RR, 0.58 (95% CI, 0.33 - 0.98) and tocolytics, 17.5% versus 25.7%; RR, 0.61 (95% CI, 0.38 - 0.98) than in women who did not [13].
Foley catheter balloon
A Foley catheter is often inserted into the cervical canal and the balloon inflated with 10 - 30 ml of saline or sterile water during the cerclage procedure. This helps to push the exposed fetal membranes cephalad and shield the membrane from rupturing when the cerclage suture is being placed. After the insertion of the suture in a pulse-string manner as close as possible to the internal os, the balloon is deflated by an assistant simultaneously as the surgical knot is tight in a coordinated manner [27].
PESSARY FOR THE TREATMENT OF SHORT CERVIX
The use of cervical pessary for the prevention of sPTB was not known until 1959 when it was first brought to the public following publication of its use in Lancet [28]. Even after this publication, its use in the United States was not popular until recently when researchers started to explore the effectiveness of cervical pessary in the prevention of sPTB. This generated interest which has culminated into multiple ongoing trials on the use of pessary in both singleton and multiple pregnancies worldwide. The most studied cervical pessary device is the Arabin pessary: a silicone ring-shaped pessary which is designed specifically for use in pregnancy. Past studies on the effectiveness of pessary in the prevention of sPTB have been sporadic, but recent studies of the use of Arabin pessary has produced mixed results. In RCT in 2012 by Goya et al., involving 385 singleton women with CL ≤25 mm with or without prior PTB, Arabin pessary significantly reduced sPTB, 6% versus 27% compared to control, (OR 0.18, 95% CI 0.08 - 0.37) [29]. Contrarily, a smaller RCT study (PECEP) in China by Hui et al., did not find any significant difference in reducing PTB prior to 34 weeks between pessary and control, 5.5% versus 9.4%, p = 0.46 [30]. In the PECEP study, the sample size was small; of 108 women, 53 were in the pessary group and 55 were controls. Moreover, women included in this study were those diagnosed with short cervix <25 mm between 20 - 24 weeks. In a larger RCT by Nicolaides involving 932 women (465 with pessary and 467 women without pessary), pessary did not prevent sPTB <34 weeks; 12.0% versus 10.8%, (OR 1.12, 95% CI 0.77 - 1.69, p = 0.57) [31]. Similarly, Dugoff et al., in another small RCT study of 391 women with CL <25 mm, only 122 agreed to participate (61 women assigned to pessary and 61 to no pessary group), there was no difference in reducing sPTB <37 weeks, 38.3% versus 32.8%, (RR 1.17, 95% CI 0.72 - 1.19, p = 0.59). In this study, all women with CL <20 mm also received vaginal progesterone [32].
The use of pessary in twin pregnancy was also not found to reduce sPTB as shown by two RCT studies. The largest RCT study, by Nicolaides et al., involved 1180 women and did not find any difference between Arabin pessary groups compared to control in reducing the rate of sPTB before 34 weeks of gestation (RR 1.05, 95% CI 0.79 - 1.41) [33]. A post hoc subgroup analysis of 106 women with CL <25 mm in this study showed that rate of reduction of sPTB <32 weeks of gestation was not significantly different between the pessary and control groups, 31% versus 26%, (RR 1.2, 95% CI 0.8 - 1.8). In another RCT study that consisted of 808 unselected women with twin pregnancies (The ProTWIN trial), there was no significant difference in reducing the rate of PTB before 32 weeks; 10% versus 12%, (RR 0.86, 95% CI 0.65 - 1.15) [34]. In addition, there was no significant reduction in adverse perinatal outcome (RR 0.98, 95% CI 0.69 - 1.39) [35]. However, a subgroup analysis of the ProTWIN study involving women with CL <38 mm showed a significant reduction of the rate of sPTB <32 weeks of gestation, 16.2% versus 39.4%, (RR 0.41, 95% CI 0.22 - 0.76).
TRANSABDOMINAL CERVICOUTERINE CERCLAGE
Several case series have demonstrated that transabdominal cervicoisthmic cerclage in patients with ultra-short cervix or previously failed transvaginal cerclage is effective in prolonging pregnancy and preventing PTB. Benson and Durfee performed their procedures preconception and in early pregnancy via open laparotomy. However, with the advent of minimally invasive surgery, use of laparoscopic or robotic-assisted approach confers better aesthesis and faster recovery. Kim et al., demonstrated in their study that apart from the many advantages of minimally invasive surgery, obstetric outcomes were similar compared to open abdominal cerclage [35]. Performing minimally invasive surgery during pregnancy has also been demonstrated to be safe and effective. Zeybek et al., showed that robotic-assisted abdominal cerclage in 6 patients with a median gestational age of 12 weeks (range 10 - 15 weeks) had median gestational age at delivery of 37 weeks (range, 33 - 39 weeks) [36]. Tyan et al., in their study of 68 consecutive patients who underwent Robot-Assisted Transabdominal Cerclage (RA-TAC) due to previous poor obstetric outcomes, showed that the odds of delivery after 34 and 37 weeks were 4.0 and 3.6 times greater when they had RA-TAC in subsequent pregnancies. The odd of neonatal survival was 12.6 times greater after RA-TAC compared to prior pregnancy outcomes [37]. In a systematic review of 26 studies consisted of 1116 patients with Transabdominal Cerclage Placed by laparotomy (TAC-lap) compared with 15 studies of 728 patients with cerclage placement via laparoscopy (TAC-lsc), there was no significant difference in overall neonatal survival between the groups; 89.9% versus 90.8%, p - .80. However, the TAC-lsc had a higher rate of deliveries at GA >34 weeks (82.9% vs 76%; p <0.01), and a lower rate of deliveries at GA between 23 to 33.6 weeks (6.8% vs 14.8%; p <0.01). The TAC-lsc also had fewer second trimester losses (3.2% vs 7.8%; p <0.01). Hence, TAC-lsc approach offers the benefits of minimally invasive surgery with better obstetric outcomes compared with TAC-lap [38].
SPECIAL CONSIDERATIONS
Two stitches versus one stitch in cerclage
The use of two stitches versus one stitch at the time of cerclage placement has also been debated. In a study by Giraldo-Isaza et al., compared the effectiveness of 2 stitches versus 1 stitch at the time of cerclage placement to decrease sPTB <37 weeks. They demonstrated that the addition of a second stitch did not improve pregnancy outcomes in both history-indicated and ultrasound-indicated cerclage procedures [39].
Sutures types for cerclage placement
Various suture materials have been used during cerclage placement. This includes the 5 mm Mersilene tape, polyester non-absorbable braided (Ethibond), Ticron and Prolene. Predominantly, the type of suture material used in cerclage is influenced by the indication. In their study, Childress et al., found that Mersilene tape was more likely to be used for cerclage placed at earlier gestation and history-indicated cerclage as compared to other non-absorbable sutures. However, they did not find any difference in gestational age at delivery, latency period, preterm birth rates, cerclage complications or adverse neonatal outcomes between Mersilene and other non-absorbable sutures when used for cervical cerclage [40].
Surgical techniques
The McDonald and Shirodkar surgical techniques have been in use since the 1950s but they are still the two most commonly used surgical techniques in contemporary cervical cerclage placement [41-43]. While both techniques aim to place the suture high up, close to the internal os, but the Shirodkar technique involves dissection of the urinary bladder. There is a suggestion that the higher the suture is placed (close to the internal os), the more effective the cerclage because it provides a longer functional CL [44]. Though both techniques are equally effective in preventing preterm birth but there are no randomized controlled trials to determine which of the two techniques is superior. In a secondary analysis of 172 women from the 580 women who met the inclusion criteria of short CL <15 mm, Odibo et al., did not find any difference in the rate of prevention of sPTB <33 weeks between McDonald and Shirodkar cerclage [45]. Use of abdominal cerclage via laparotomy or minimally invasive procedures with either laparoscopic or robotic is gradually gaining grounds in obstetric practice.
CONCLUSION
Preventing sPTB in women with short cervix has evolved over time as newer interventions become available. There are general consensuses and guidelines on how to manage women with incidental short cervix or ultrasonographic short cervix <25 mm before 24 weeks in women with prior sPTB. However, controversies still exist on how to manage short cervix in twin pregnancies, and which treatment modality best suits women with singleton pregnancy with extremely short CL <10 mm. Current interventions aim towards preventing progressive cervical shortening, but a multi-modal approach may be more beneficial in women with extreme short cervix and/or dilated cervix.
DECLARATION OF INTEREST
We declare that none of the authors of this manuscript or their family members has conflict of interest in any of the products mentioned in this manuscript. There is also no financial sponsorship or funding to declare by any of the authors. All the authors listed herewith participated and contributed immensely in the drafting and writing of this manuscript, and it has neither been published nor submitted for publication elsewhere.
REFERENCES
- Koullali B, Oudijk MA, Nijman TA, Mol BW, Pajkrt E (2016) Risk assessment and management to prevent preterm birth. Semin Fetal Neonatal Med 21: 80-88.
- Goldenberg RL, Culhane JF, Iams JD, Romero R (2008) Epidemiology and causes of preterm birth. Lancet 371: 75-84.
- Moster D, Lie RT, Markestad T (2008) Long-term medical and social consequences of preterm birth. N Engl J Med 359: 262-273.
- The World Health Organization (2018) Preterm birth. WHO, Geneva, Switzerland.
- Owen J, Hankins G, Iams JD, Berghella V, Sheffield JS, et al. (2009) Multicenter randomized trial of cerclage for preterm birth prevention in high-risk women with shortened midtrimester cervical length. Am J Obstet Gynecol 201: 375.
- Berghella V, Haas S, Chervoneva I, Hyslop T (2002) Patients with prior second-trimester loss: Prophylactic cerclage or serial transvaginal sonograms? Am J Obstet Gynecol 187: 747-751.
- Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM (2005) Cerclage for short cervix on ultrasonography: meta-analysis of trials using individual patient-level data. Obstet Gynecol 106: 181-189.
- Berghella V, Rafael TJ, Szychowski JM, Rust OA, Owen J (2011) Cerclage for short cervix on ultrasonography in women with singleton gestations and previous preterm birth: A meta-analysis. Obstet Gynecol 117: 663-671.
- Wapner RJ, Cotton DB, Artal R, Librizzi RJ, Ross MG (1995) A randomized multicenter trial assessing a home uterine activity monitoring device used in the absence of daily nursing contact. Am J Obstet Gynecol 172: 1026-1034.
- Iams JD, Newman RB, Thom EA, Goldenberg RL, Mueller-Heubach E, et al. (2002) Frequency of uterine contractions and the risk of spontaneous preterm delivery. N Engl J Med 346: 250-255.
- Fonseca EB, Celik E, Parra M, Singh M, Nicolaides KH, et al. (2007) Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med 357: 462-469.
- ACOG (2014) Practice Bulletin No. 142: Cerclage for the Management of Cervical Insufficiency. Obstetrics & Gynecology 123: 372-379.
- Berghella V, Ciardulli A, Rust OA, To M, Otsuki K, et al. (2017) Cerclage for sonographic short cervix in singleton gestations without prior spontaneous preterm birth: Systematic review and meta-analysis of randomized controlled trials using individual patient-level data. Ultrasound Obstet Gynecol 50: 569-577.
- McIntosh J, Feltovich H, Berghella V, Manuck T (2016) The role of routine cervical length screening in selected high- and low-risk women for preterm birth prevention. Am J Obstet Gynecol 215: 2-7.
- Meis PJ, Klebanoff M, Thom E, Dombrowski MP, Sibai B, et al. (2003) Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med 348: 2379-2385.
- Society of Maternal Fetal Medicine Clinical Guideline, Berghella V (2012) Progesterone and preterm birth prevention: Translating clinical trials data into clinical practice. Am J Obstet Gynecol 206: 376-386.
- ACOG (2018) Practice bulletin no. 130: prediction and prevention of preterm birth. Obstet Gynecol 120: 964-973.
- Villar J, Papageorghiou AT, Knight HE, Gravett MG, Iams J, et al. (2012) The preterm birth syndrome: A prototype phenotypic classification. Am J Obstet Gynecol 206: 119-123.
- Enakpene CA, DiGiovanni L, Jones TN, Marshalla M, Mastrogiannis D, et al. (2018) Cervical cerclage for singleton pregnant patients on vaginal progesterone with progressive cervical shortening. Am J Obstet Gynecol 219: 397.
- Romero R, Nicolaides K, Conde-Agudelo A, Tabor A, O'Brien JM, et al. (2012) Vaginal progesterone in women with an asymptomatic sonographic short cervix in the midtrimester decreases preterm delivery and neonatal morbidity: A systematic review and metaanalysis of individual patient data. Am J Obstet Gynecol 206: 124.
- Schuit E, Stock S, Rode L, Rouse DJ, Lim AC, et al. Effectiveness of progestogens to improve perinatal outcome in twin pregnancies: an individual participant data meta-analysis. BJOG 122: 27-37.
- Roman A, Rochelson B, Martinelli P, Saccone G, Harris K, et al. (2016) Cerclage in twin pregnancy with dilated cervix between 16 to 24 weeks of gestation: Retrospective cohort study. Am J Obstet Gynecol 215: 98.
- Roman A, Rochelson B, Fox NS, Hoffman M, Berghella V, et al. (2015) Efficacy of ultrasound-indicated cerclage in twin pregnancies. Am J Obstet Gynecol 212: 788.
- Li C, Shen J, Hua K (2019) Cerclage for women with twin pregnancies: A systematic review and metaanalysis. Am J Obstet Gynecol 220: 543-557.
- Han MN, O'Donnell BE, Maykin MM, Gonzalez JM, Tabsh K, et al. (2019) The impact of cerclage in twin pregnancies on preterm birth rate before 32 weeks. J Matern Fetal Neonatal Med 32: 2143-2151.
- Adams TM, Rafael TJ, Kunzier NB, Mishra S, Calixte R, et al. (2018) Does cervical cerclage decrease preterm birth in twin pregnancies with a short cervix? J Matern Fetal Neonatal Med 31: 1092-1098.
- Holman MR (1973) An aid for cervical cerclage. Obstet Gynecol 42: 468-469.
- Cross RG (1959) Treatment of habitual abortion due to cervical incompetence. Lancet 274: 127.
- Goya M, Pratcorona L, Merced C, Rodó C, Valle L, et al. (2012) Cervical pessary in pregnant women with a short cervix (PECEP): An open-label randomised controlled trial. Lancet 379: 1800-1806.
- Hui SY, Chor CM, Lau TK, Lao TT, Leung TY (2013) Cerclage pessary for preventing preterm birth in women with a singleton pregnancy and a short cervix at 20 to 24 weeks: A randomized controlled trial. Am J Obstet Gynecol 30: 283-288.
- Nicolaides KH, Syngelaki A, Poon LC, Picciarelli G, Tul N, et al. (2016) A randomized trial of cervical pessary to prevent preterm singleton birth. N Engl J Med 374: 1044-1052.
- Dugoff L, Berghella V, Sehdev H, Mackeen AD, Goetzl L, et al. (2018) Prevention of preterm birth with pessary in singletons (PoPPS): Randomized controlled trial. Ultrasound Obstet Gynecol 51: 573-579.
- Nicolaides KH, Syngelaki A, Poon LC, De PacoMatallana C, Plasencia W, et al. (2016) Cervical pessary placement for the prevention of preterm birth in unselected twin pregnancies: A randomized controlled trial. Am J Obstet Gynecol 214: 1-9.
- Liem S, Schuit E, Hegeman M, Bais J, De Boer K, et al. (2013) Cervical pessaries for prevention of preterm birth in women with a multiple pregnancy (ProTWIN): A multicenter, open-label randomized controlled trial. Lancet 382: 1341-1349.
- Kim S, Hill A, Menderes G, Cross S, Azodi M, et al. (2018) Minimally invasive abdominal cerclage compared to laparotomy: A comparison of surgical and obstetric outcomes. J Robot Surg 12: 295-301.
- Zeybek B, Hill A, Menderes G, Borahay MA, Azodi M, et al. (2016) Robotic-Assisted Abdominal Cerclage during Pregnancy. JSLS 20: 1-7.
- Tyan P, Mourad J, Wright B, Winter M, Garza D, et al (2019) Robot-assisted transabdominal cerclage for the prevention of preterm birth: A multicenter experience. Eur J Obstet Gynecol Reprod Biol 232: 70-74.
- Moawad GN, Tyan P, Bracke T, Abi Khalil ED, Vargas V, et al. (2018) Systematic Review of Transabdominal Cerclage Placed via Laparoscopy for the Prevention of Preterm Birth. J Minim Invasive Gynecol 25: 277-286.
- Giraldo-Isaza MA, Fried GP, Hegarty SE, Suescum-Diaz MA, Cohen AW, et al. (2013) Comparison of 2 stitches vs 1 stitch for transvaginal cervical cerclage for preterm birth prevention. Am J Obstet Gynecol 208: 1-9.
- Childress KM, Dickert EJ, Flick AA, Myles TD, Amon E, et al. (2016) A Comparison of Mersilene Suture to other Non-Absorbable Suture in Cervical Cerclage. Obstet Gynecol 127: 68S-69S.
- McDonald IA (1980) Cervical cerclage. Clin Obstet Gynecol 7: 461-479.
- Shirodkar VN (1955) A new method for operative treatment for habitual abortions in the second trimester of pregnancy. Antiseptic 52: 299-300.
- McDonald IA (1957) Suture of the cervix for inevitable miscarriage. J Obstet Gynecol Br Emp 64: 346-350.
- Katz M, Abrahams C (2005) Transvaginal placement of cervicoisthmic cerclage: Report on pregnancy outcome. Am J Obstet Gynecol 192:1989 -1992.
- Odibo AO, Berghella V, To MS, Rust OA, Althuisius SM, et al. (2005) Shirodkar versus McDonald cerclage for the prevention of preterm birth (PTB) in women with short cervical length. Am J Obstet Gynecol 193: S155.
Citation: Enakpene CA, Dijeh FC, Vengalil ET, Mastrogiannis D (2020) An Overview of the Role of Cerclage in the Prevention of Spontaneous Preterm Birth. J Reprod Med Gynecol Obstet 5: 048.
Copyright: © 2020 Christopher A Enakpene, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

