
An Unusual Case of Widespread, Pruritic Metastatic Crohn’s
*Corresponding Author(s):
Michael SchultheisDepartment Of Dermatology, Universitaetsmedizin, Johannes Gutenberg University, Mainz, Germany
Email:Michael.Schultheis@unimedizin-mainz.de
Abstract
Patients suffering from Crohn’s disease often present with skin symptoms, mainly in the perianal area.
We here report on a patient with widespread granulomatous skin lesions covering a large body surface. Histology findings together with the clinical presentation led to the diagnosis of “metastatic” Crohn’s disease. This case report is interesting due to the diagnostic challenges this type of skin manifestation presented. Of note, the Crohn’s disease (CD) affecting the Gastro Intestinal (GI) tract presented less severe than the skin symptoms.
Extraintestinal manifestations and co-morbidities of Crohn’s disease are often challenging and require interdisciplinary management.
We here describe an unusual case of metastatic Crohn’s Disease.
Keywords
Crohn’s disease; Metastatic; Pruritic; Skin lesions; Skin manifestation
Case Presentation
A 68 year old female patient presented to dermatology with a highly pruritic rash for which she had received clobetasol and amitriptyline from accident and emergency services (A&E). The papular rash extended over arms, ankles and feet.
Concomittantly the patient also developed gastro-intestinal symptoms. Endoscopic and histological investigations revealed findings in keeping with CD presenting as proctosigmoiditis. There was no perianal CD. While a flare was treated with steroids gastro, intestinal symptoms thereafter remained quiescent and no maintenance therapy was required for the luminal CD at this stage.
A skin biopsy showed interstitial granulomatous disease. Itch and sleep loss remained a predominant issue for the patient and this was not alleviated by Ultraviolet radiation B (UVB) treatment, promethazine or topicals. Symptoms failed to respond to other treatments received including Lymecycline, clarithromycin, Hydroxychloroquine, fexofenadine and hydroxyzine.
Dermatology Life Quality Index (DLQI) scored 23 indicating very severe QoL impairment. A 30mg dose of prednisolone failed to be of clear benefit. Only a 60 mg dose resulted in almost complete temporary clearance of skin lesions, which however relapsed upon tapering.
A clinico-dermatohistology discussion confirmed the diagnosis of cutaneous Crohns (Figure 1). The inderdisciplinary decision was made to treat this patient with a TNF alpha inhibitor (TNFi) and adalinumab was approved to be given by dermatology. Unfortunately, the patient failed to have a convincing response to adalinumab from the side of the skin while the gastroenteric symptoms improved greatly. It was then decided to switch her to infliximab in combination with low dose Methotrexat (MTX) (10mg/week). This treatment scheme was of benefit for the patient (Figure 2). Systemic steroids could be discontinued. The patient however still showed new lesion formation about 2 weeks prior to her 8 weekly infliximab injections. She was completely symptom free when receiving the loading dose. The patient will continue on Infliximab.
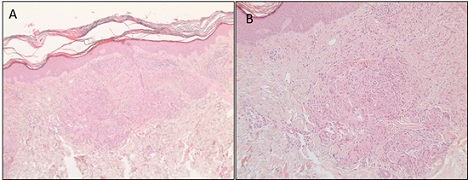 Figure 1: The histology (left hand side overview, right hand side magnification) shows non-caseating granulomas with giant cells. These were found in the papillary and reticular dermis. The granulomas are surrounded by an inflammatory infiltrate.
Figure 1: The histology (left hand side overview, right hand side magnification) shows non-caseating granulomas with giant cells. These were found in the papillary and reticular dermis. The granulomas are surrounded by an inflammatory infiltrate.
 Figure 2: Skin changes before initiation of infliximab in combination with methotrexate (A and D) and after initiation (C and B).
Figure 2: Skin changes before initiation of infliximab in combination with methotrexate (A and D) and after initiation (C and B).
Discussion
CD is well described to present with extra-intestinal symptoms [1,2]. Three different types of cutaneous involvements are distinguished: 1). Extension of bowel disease to the skin, often as perianal fistulas, ulcers or abscesses. 2). Metastatic Crohn’s is rarer and comes with Crohn’s typical histology of granulomata but at sites distant from the gastrointestinal involvement. 3). Reactive lesions which do not share a granulomatous histology such as Pyoderma gangraenosum, Sweet Syndrome or Erythema nodosum.
Metastatic Crohn’s (MCD) is rare [3-5]. MCD is poorly understood. One view on its pathogenesis is based on the idea that (intestinal) antigens circulate to and thus are expressed in the skin. Sensitisation to bacterial gut antigen and cross-reactivity with skin expressed antigenic material have also been discussed.
One could also argue about an important role of skin homing receptors. Cutaneous lymphocyte Antigen (CLA) is known to be specifically upregulated by Interleukin-12 (IL-12) and the involvement of IL-12 in CLA expression on leukocytes could be an argument for considering ustekinumab in the therapeutic pathway.
Differential Diagnosis
The two main differential diagnoses include disseminated Granuloma annulare and cutaneous sarcoidosis. The well defined granuloma [6] are not typically seen in Granuloma annulare which presents with palisading histiocytosis and necrobiosis not seen in our biopsy. Thus cutaneous sarcoidosis remains as a main differential. Indeed, a case with co-existence of sarcoidosis and GI Crohn’s has been described [7] and both entities are known to respond to infliximab. However, our patient lacks any lung or other involvement of sarcoidosis, has a normal angiotensin-converting enzyme (ACE) level and, in addition, the co-incidence between onset of Crohn’s and skin symptoms strongly favours the diagnosis of MCD.
Pruritus
Cutaneous Crohn’s lesions are not described to go along with pruritus but often present as indolent lesions. However, our patient presented with granulomata and accompanying inflammatory infiltrate near the epidermal layer. Lymphocytic intraepidermal infiltration does usually cause itch. Of note, other case reports also highlight pruritus as symptom.
Other Treatment Options (Ustekinumab)
Infliximab has been described as a successful therapy for MCD [8]. We were surprised about the lack of response to adalinumab [9,10]. However Infliximab is well known to have a superior efficacy in difficult to treat inflammatory patterns. Ustekinumab was discussed as an alternative approach and this therapy has been successfully used for MCD.
Summary and Conclusion
In the case of granulomatous skin lesions associated with Crohn's disease, three main clinical pictures can be considered because of similar histological findings and clinical manifestations: metastatic Crohn’s disease, Granuloma annulare disseminatus and cutaneous sarcoidosis. An immunomodulatory therapy should be selected to treat non-caseating granulomatous diseases.
References
- Ko JS, Uberti G, Napekoski K, Patil DT, Billings SD (2016) Cutaneous manifestations in inflammatory bowel disease: a single institutional study of non-neoplastic biopsies over 13 years. J Cutan Pathol. 43: 946-55.
- Pagani K, Lukac D, Bhukhan A, McGee JS (2022) Cutaneous Manifestations of Inflammatory Bowel Disease: A Basic Overview. Am J Clin Dermatol. 23: 481-497.
- Aberumand B, Howard J, Howard J (2017) Metastatic Crohn's Disease: An Approach to an Uncommon but Important Cutaneous Disorder. Biomed Res Int. 2017: 8192150.
- Ickrath F, Stoevesandt J, Schulmeyer L, Glatzel C, Goebeler M, et al. (2021) Metastatic Crohn's disease: an underestimated entity. J Dtsch Dermatol Ges. 19: 973-82.
- Streight KL, Braun TL, Lowe N, Kim SJ (2020) A Rare Clinical Presentation of Metastatic Crohn's Disease. Cureus. 12: e8285.
- Chatterjee D, Bhattacharjee R, Khullar G, Kumaran S, De D, et al. (2020) Metastatic Crohn Disease: A Clinicohistological Appraisal From a Tertiary Care Center in India. Am J Dermatopathol. 42: 506-12.
- Chung J, Rosenbach M (2014) Extensive cutaneous sarcoidosis and coexistant Crohn disease with dual response to infliximab: case report and review of the literature. Dermatol Online J. 21: 13030/qt6m04m5s3.
- Yoong C, Schofield C, Rodins K, Faulkner C (2014) Cutaneous Crohn's disease treated with infliximab and 4 years of follow up. Australas J Dermatol. 55: e40-3.
- Miller FA, Jones CR, Clarke LE, Lin Z, Adams DR, et al. (2009) Successful use of adalimumab in treating cutaneous metastatic Crohn's disease: report of a case. Inflamm Bowel Dis. 15: 1611-2.
- Evans J, Sapsford M, McDonald S, Poole K, Raine T, et al. (2021) Prevalence of axial spondyloarthritis in patients with inflammatory bowel disease using cross-sectional imaging: a systematic literature review. Ther Adv Musculoskelet Dis. 13: 1759720X21996973.
Citation: Pugalenthy S, Edwards S, Schultheis M, Selinger C, Helliwell PS, et al. (2024) An Unusual Case of Widespread, Pruritic Metastatic Crohn’s. J Clin Stud Med Case Rep 11:227
Copyright: © 2024 Sarajeni Pugalenthy, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

