
Appendiceal Intussusception in Pediatric Patient - Case Report
*Corresponding Author(s):
Ivan PetracicDepartment Of Pediatric Surgery, Children's Hospital Zagreb, University Of Zagreb, Croatia
Tel:+ 385 918901180,
Email:ivanpetracicmd@gmail.com
Abstract
Appendiceal intussusception is a very rare cause of acute abdomen in pediatric patients. It is a cause of acute abdominal pain in 0.01% of all patients who underwent appendectomy. We would like to present a case of a 14-years-old boy who was administered to our hospital because of abdominal pain which lasted for about 12 hours. After the initial diagnostic investigation was performed, a decision for operative treatment was made. The pathohistological investigation showed that tumorous structure which was found intraoperatively was actually inflamed appendix with fecalith, invaginated into the cecal wall. We will give a brief review of the relevant literature concerning this topic.
Keywords
Acute abdomen; Appendiceal intussusception; Appendicitis; Children; Ultrasound
INTRODUCTION
According to literature, appendiceal intussusception (invagination) was first described by McKidd in 1858. An incidence of appendiceal invagination is only about 0.01% of all patients undergoing appendectomy. It usually remains unrecognized during routine diagnostic procedures and it is not confirmed until the surgery. There are no pathognomonic findings on ultrasound, barium enema, CT-scan or colonoscopy. Sometimes it can only be diagnosed by pathohistological examination. We will present a case of appendiceal invagination in a 14-years-old boy.
CASE REPORT
We would like to present a case of a 14-years-old boy who was administered to our hospital because of abdominal pain which lasted for about 12 hours. He had no history of recent vomiting or fever. His past history included a surgical treatment of sigmoid colon intussusception at the age of 7. The surgical reduction of volvulus and sigmoid colon intussusception was performed. During the postoperative follow-up period patient had no abdominal symptoms.
Physical examination revealed abdominal pain during palpation, more intense in lower right abdominal quadrant. The laboratory tests showed elevated leukocytes count. Preoperative ultrasound examination of the abdomen was performed. Ultrasound demonstrated an appendix 12mm in diameter with an inflamed wall. Appendix had radiological criteria for gangrenous inflammation. The decision for open appendectomy was made. Intraoperatively, after approaching the cecum, a tumorous structure about 5 cm in diameter was found. The structure was part of cecum and packages of enlarged lymph nodes were surrounding it. The resection of the tumorous structure along with mesentery and lymph nodes was performed. Terminal ileum and ascending colon were connected with termino-lateral anastomosis. The undefined tumor was sent to pathohistology. The PHD showed that tumorous structure was actually inflamed appendix with fecalith, invaginated into the cecal wall (Figures 1 and 2). Also, the ileal mucosa was full of small polyps (around 50) that were analysed immunohistochemically (CD3, CD20, bcl-2, Ki-67) and diagnosed as follicular nodular hyperplasia (Figure 2). No signs of malignancy were found. During postoperative follow-up (duration of follow-up was about 14 months) he had no further abdominal symptoms.
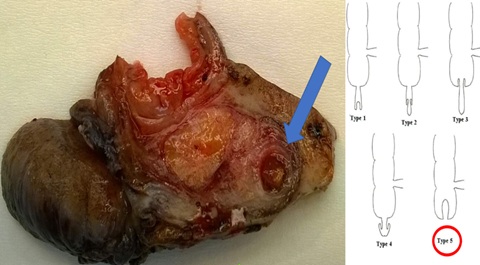
Figure 1: Inflamed appendix with fecolith, invaginated into the cecal wall. As described by McSwain, this a type V of appendiceal invagination [1].
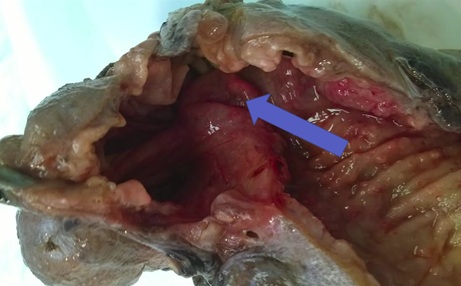
Figure 2: The arrow shows appendix invaginated into the cecal wall, as seen from the bowel lumen. Follicular nodular hyperplasia can be seen.
DISCUSSION
Appendiceal intussusception is a very rare cause of pediatric acute abdomen. As mentioned in the introduction, it was first described in 1858 by McKidd in a 7-years-old child. In 1963, based on a prospective study by Collins which 71,000 cases of appendectomy during 40 years, that the incidence of appendiceal intussusception was 0.01%. In 2009, Chaar et al., did the comprehensive review of the literature written in English language and found 190 cases of intussusception of appendix [2]. They reported that intussusception is more common in adults (76%) than in children (24%). Female patients (72%) are 2 times more affected than men (28%) in the adult population, whereas male patients (58%) may be slightly more affected in the pediatric population. Patient age varies from 5 months to 85 years. Average age of presentation is 7 years in pediatric patients.
Anatomical factors, such as a hypermobile appendix, a wide lumen and a thin mesoappendix can facilitate the intussusception. More often, pathological factors such as fecalith, parasites, foreign bodies, follicular nodular hyperplasia, mucocele [3,4] or benign or malignant neoplasms can be leading points of the invagination [5,6]. It has been reported that in pediatric age, the most frequent cause is appendicitis itself. When comparing our patient's history, physical examination and pathohistological findings we can see that he had 4 risk factors for appendiceal invagination: he was a boy, he had acute appendicitis with fecalith in lumen of appendix and he had follicular nodular hyperplasia.
The preoperative diagnosis of invaginated appendix is difficult. The symptoms may be similar to acute appendicitis or a bowel intussusception. The pain is usually colic-like abdominal pain (the most common symptom, 78%) with vomiting (26%) and with or without blood in the stool (23%).
Another fact that can lead to misdiagnosing the condition is that intussusception can be reversed, especially if it is not associated with a lead point. Patients may present with symptoms of abdominal pain, nausea, and vomiting which can be completely resolved with spontaneous reduction of the intussusceptum. A lot of patients (63%) can have a chronic presentation during a period of weeks to months [2]. This can be applied to adults as well as children.
According to literature patients with chronic abdominal pain and even asymptomatic patients who were diagnosed with appendiceal intussusception were usually diagnosed by CT or colonoscopy [2,4]. Only a few cases of asymptomatic or chronic invaginaion were diagnosed by abdominal ultrasound [2,7]. In these cases, the conservative, hydrostatic disinvagination is usually impossible and appendectomy is treatment of choice [2].
In 1910, Moschowitz made the first classification of appendiceal intussusception. The classification was later modified by McSwain in 1941 [1,8]. Their classification is based on anatomy and describes which part of the appendix is the intussusceptum and where the intussuscipiens is located. McSwain described 5 types of appendiceal intussusception. In type I, the tip of the appendix is intussusceptum and is invaginated into proximal part of appendix. Type II is a form of intussusception when invagination starts at some point along the length of the appendix. When the invagination starts at the junction of appendix and cecum, we are talking about type III. Type IV is retrograde intussusception - the proximal appendix is invaginated into the distal appendix. And finally, type V is complete invagination of appendix into the cecum and is usually the progression of type I, II or III.
Appendiceal intussusception can also be classified as primary (compound) or secondary. Each type of the previously described primary appendiceal intussusceptions, possibly with the exception of type IV, can initiate a secondary intussusception. The anatomy of cecum and degree of irritation of cecum by presence of invaginated appendix will define whether the intussuscepted appendix will trigger a secondary intussusception. As mentioned before, a fixed caecum has small chances for intussusception. It has been reported decades ago that intussuscepted appendix can lead to complete colonic intussusception and protrusion of inverted appendix from the anus [9].
The literature proposes three treatment options for intussuscepted appendix: conservative, minimally invasive or surgical. Few factors have to be considered when the decision has to be made: Patient’s age, recurrence, eventual comorbidities and risk of neoplasm. The risk of neoplasm is extremely low in pediatric patients. The reduction of intussusception using hydrostatic reduction is preferable in children but only in cases where diagnosis is certain. However, there is a high recurrence rate. Also, pneumatic reduction producing cecal distension by rectal tube is an option. In these cases a close follow-up is indicated, because of the high rate of recurrence.
Minimally invasive treatment includes colonoscopy. Many authors suggest that when the diagnosis of appendiceal intussusception is suspected, the colonoscopy should be performed if possible. During colonoscopy, the intussusception may be reduced by performing several insufflations of air. It is very advisable to avoid endoscopic removal because perforation and subsequent peritonitis are common and serious complications. The resection of appendix with looping and snare retrieval should be performed only by experienced gastroenterologists and only when the diagnosis of appendiceal intussusception is certain.
Most of the authors agree that the treatment of choice for the appendiceal intussusception is surgical removal of the appendix. It can be done either with laparotomy or laparoscopy. Wolf and Boller suggest that during surgical intervention, an attempt to manually reduce the intussuscepted appendix should be made if it is possible. If the intussusception is not reducible, cecotomy (along a taenia band) should be performed. In our presented case the resection of cecum along with intussuscepted appendix was performed because the diagnosis was not certain: macroscopically, the cecum was appearing as tumorous mass with no apparent appendix which was invaginated into cecal wall in total length of 5cm. Due to inflammation, follicular nodular hyperplasia and the invagination itself it was not possible to determine what the exact pathology in situ was. Therefore, the resection of the tumorous structure along with surrounding caecum and terminal ileum with mesentery and lymph nodes was performed.
In pediatric patients the treatment of choice is the laparoscopic approach. Laparoscopic reduction is successful in 50% to 65% [10]. Exploratory laparotomy is the management of choice if there is any suspicion of appendiceal mass (as it was in presented case), cecal neoplasm or compound ileocaecal-appendiceal intussusception. Sometimes, right hemicolectomy with lymph node resection is the treatment of choice. When the tumor is larger than 2 cm in diameter or malignancy is suspected, right hemicolectomy should be performed. For simple cases, when the diagnosis in apparent, simple appendectomy may be sufficient [11]. A large number of appendiceal intussusception is caused by benign mucoceles (benign mucinous tumors). They should be approached with special care because they can be mistaken for mucinous cystadenocarcinoma. Usually, mucocele can be cured with appendectomy (simple excision) but the tumor rupture has to be avoided as a measure of precaution because mucinous cystadenocarcinoma can cause pseudomyxoma of peritoneum. In case of pseudomyxoma peritonei, treatment should include appendectomy, omentectomy and in females bilateral oophorectomy. Intraperitoneal chemotherapy may be useful.
In cases of mobile caecum or ascending colon, in order to prevent invagination, it is recommended that during laparotomy these structures are attached to the lateral abdominal wall by sutures. Finally, some authors suggest that surgical intervention may be unnecessary in patients with long-standing asymptomatic appendiceal intussusception. A close follow up is indicated in these cases [12].
CONCLUSION
Appendiceal intussusception is a very rare cause of acute abdomen in children. There are no pathognomonic findings during routine radiological diagnostic procedures. Due to these facts it often remains unrecognized until opened surgery or even pathohistological analysis. The aim of this case presentation was to contribute to general awareness of the possibility that appendiceal intussusception could cause acute abdomen in pediatric patients and to contribute to literature data from which further literature reviews can be performed. The review of the literature reveals some different opinions on appendiceal invagination approach - from strictly conservative (close follow-up) to surgical (laparoscopic, open laparotomy).
As the appendiceal intussusception is a very rare entity, it is very hard to gain experience on a local level. Therefore, more experience should be acquired globally, more cases should be presented in literature and more systematic literature reviews should be performed.
CONFLICT OF INTEREST
The authors whose names are listed immediately below certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
REFERENCES
- McSwain B (1941) Intussusception of the appendix. South Med J 34: 263-271.
- Chaar CIO, Wexelman B, Zuckerman K, Longo W (2009) Intussusception of the appendix: Comprehensive review of the literature. Am J Surg 198: 122-128.
- Blondiaux E, Savoye-Collet C, Foulatier O, Lemoine F, Dacher JN (2007) Appendiceal intussusception caused by a mucocele of the appendix: Imaging findings. Dig Liver Dis 39: 1087.
- Waseem T, Javaid-ur-Rehman, Sabir NU, Hussain S, Amir E, et al. (2007) Rare association: Ileocaeco-colic intussusception secondary to mucinous cystadenoma of the appendix in an adult. ANZ J Surg 77: 1021–1022.
- Butte JM, Torres J, Henriquez IM, Pinedo G (2007) Appendicular mucosal intussusception into the cecum secondary to an intramural mucinous cystadenoma of the appendix. J Am Coll Surg 204: 510.
- Takahashi M, Sawada T, Fukuda T, Furugori T, Kuwano H (2003) Complete appendiceal intussusception induced by primary appendiceal adenocarcinoma in tubular adenoma: A case report. Jpn J Clin Oncol 33: 413-415.
- Pumberger W, Hormann M, Pomberger G, Hallwirth U (2000) Sonographic diagnosis of intussusception of the appendix vermiformis. J Clin Ultrasound 28: 492-496.
- Moschowitz AV (1910) Intussusception of the appendix. Med Rec N Y 78: 1087-1095.
- Dunavant D, Wilson H (1952) Intussusception of the appendix, with complete inversion of the appendix and protrusion from the anus. Ann Surg 135: 287-288.
- Schier F (1997) Experience with laparoscopy in the treatment of intussusception. J Pediatr Surg 32: 1713-1714.
- Chen YC, Chiang JM (2000) Appendiceal intussusception with adenocarcinoma mimicking a cecal polyp. Gastrointest Endosc 52: 130-131.
- Salehzadeh A, Scala A, Simson JN (2010) Appendiceal intussusception mistaken for a polyp at colonoscopy: Case report and review of literature. Ann R Coll Surg Engl 92: 46-48.
Citation: Petracic I, Pajic A, Visnjic S, Gliha A, Car A, et al. (2020) Appendiceal Intussusception in Pediatric Patient - Case Report. J Surg Curr Trend Innov 4: 026.
Copyright: © 2020 Ivan Petracic, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

