
Applicability of Dermoscopy in the Atypical Presentation of Tinea Pedis: A Case Report
*Corresponding Author(s):
Balachandra S AnkadDepartment Of Dermatology, S. Nijalingappa Medical College, Navanagar, Bagalkot-587102, Karnataka, India
Tel:+91 9980410056,
Email:drbsankad@gmail.com
Introduction
Sir,
Tinea pedis, also known as athlete’s foot or foot ringworm is an infection of the feet or toes with dermatophyte fungus [1]. Trichophyton rubrum is the most common isolate accounting for 70% of cases. Other species include Trichophyton interdigitale, Trichophyton mentagrophytes and Epidermophyton floccosum. The ideal conditions for fungal growth include hot and humid environment, prolonged use of occlusive footwear, excessive sweating and prolonged exposure to water [2]. The maceration of the skin due to above risk factors along with keratinases released by fungus helps in easy invasion of the keratin layer. The mannans contained in the fungal cell wall also further suppress the body’s immunity thus, contributing to tinea pedis. Herein we describe a case of recurrent vesiculobullous type of tinea pedis who was inappropriately managed previously.
A 25-year-old male, presented to the outpatient department of dermatology at our institute, with history of recurrent painful pus filled lesions over plantar aspect of right great toe extending to the toe cleft since five months. Lesions used start as vesicles with minimal itching. Patient earlier received topical steroid and, topical and oral antibiotics. Lesions healed temporarily only to recur. On examination, multiple vesicles, frank pustules with along with a single deep fissure over plantar aspect of great toe covered with scaling and sero-hemorrhagic crusts was observed (Figure 1). There were no similar lesions elsewhere in the body, and nails were also spared. Possibility of allergic contact dermatitis, pompholyx, eczema, localized pustular psoriasis and tinea pedis with secondary infection were thought as differentials. Dermoscopy was done with 10x magnification that demonstrated red and reddish-brown, globules, along with circular and circular and linear white scales (Figure 2a). Bedside investigations including potassium hydroxide (KOH 10%) mount from edge of the lesion and Gram’s stain from pustule was obtained which respectively revealed branched septate hyphae with arthrospores (Figure 2b), and cocci arranged in chains. Patient was started on Itraconazole (Sporanox®) 100mg twice daily for 4 weeks and topical mupirocin ointment with oral antihistamines. After 2 weeks, the lesions appeared dry with healing of the fissure, and few scales with pinkish background was noted (Figure 3a). He showed gradual improvement and complete resolution with disappearance of pustules and oozing areas by 4th week of treatment. Minimal brownish scales were noted at the periphery (Figure 3b).Topical antifungal was added to treatment protocol at this stage. The treatment was continued for further 2 weeks. He was advised to avoid prolonged occlusive footwear and in keeping the feet dry. Patient had no relapse even after 3months of follow up.
 Figure 1: Clinical image of tinea pedis showing multiple vesicles with pustules and scaling and sero-hemorrhagic crusts. Area of dermoscopic examination is denoted by box.
Figure 1: Clinical image of tinea pedis showing multiple vesicles with pustules and scaling and sero-hemorrhagic crusts. Area of dermoscopic examination is denoted by box.
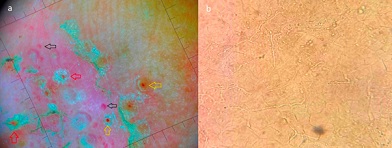 Figure 2: (a) Dermoscopy reveals red (black arrows), reddish-brown globules (yellow arrows), and circular and linear white scales (red arrows). (b) KOH mount demonstrated branched septate hyphae with arthrospores.
Figure 2: (a) Dermoscopy reveals red (black arrows), reddish-brown globules (yellow arrows), and circular and linear white scales (red arrows). (b) KOH mount demonstrated branched septate hyphae with arthrospores.
 Figure 3: (a) After 2 weeks of treatment, lesions are dry with few scales with pinkish background. (b) After 4 weeks, almost complete resolution with minimal brown scales is seen.
Figure 3: (a) After 2 weeks of treatment, lesions are dry with few scales with pinkish background. (b) After 4 weeks, almost complete resolution with minimal brown scales is seen.
Tinea pedis is a common, prevalent, superficial dermatophyte infection of feet. It presents in several clinical varieties such as hyperkeratotic, intertriginous, vesiculobullous, ulcerative or in any combination. It is usually accompanied by dermatophytic infection of other parts of the body (groin, hands or nails). Chronic infection is common in patients with concomitant diabetes, atopy and immunosuppression [3]. Tinea pedis has also been found to be a significant risk factor for acute bacterial cellulitis of the leg, hence requires prompt treatment [4].
In this report, patient was an immunocompetent, non diabetic with absence of fungal infections in other body parts presented with tinea pedis. Even though, recurrent lesion is attributed to topical steroid usage, localization of the lesion was unique in this case. Topical anti-fungal agents are the first line of treatment; he was started with oral itraconazole for 6 weeks due to chronic lesions and history of recurrence. It is an orally active triazole by action through inhibition of cytochrome p450 dependent demethylation stage in formation of ergosterol on the fungal cell membrane [5]. KOH mount is the mainstay to investigate dermatophytosis. Recently dermoscopy is proven to be a non-invasive and rapid tool as an adjunctive in the diagnosis of dermatophytosis in which brown, black and reddish-brown globules, dotted vessels, and white scales are typically observed [6]. Similar findings were noted in this case too. Dermoscopy and KOH were best utilized in the diagnosis. Patient improved drastically with relief from pain and itching.
To conclude, keeping broad vision of differentials and befitting the use of simple bedside investigations helps in early righteous diagnosis and treatment of tinea pedis. Therefore, high index of suspicion in atypical clinical presentation and appropriate utility of dermoscopy and KOH mount in the accurate diagnosis and proper management of tinea pedis are highlighted in this report.
References
- Rajagopalan M, Inamadar A, Mittal A, Miskeen AK, Srinivas CR, et al. (2018) Expert Consensus on The Management of Dermatophytosis in India (ECTODERM India). BMC Dermatol 18: 6.
- Wang R, Song Y, Du M, Yang E, Yu J, et al. (2018) Skin microbiome changes in patients with interdigital tinea pedis. Br J Dermatol 179: 965-968.
- Szepietowski JC, Reich A, Garlowska E (2006) Factors influencing coexistence of toenail onychomycosis with tinea pedis and other dermatomycoses: A survey of 2761 patients. Arch Dermatol 142: 1279-1284.
- Roujeau JC, Sigurgeirsson B, Korting HC, Kerl H, Paul C (2004) Chronic dermatophytoses of the foot as risk factors for acute bacterial cellulitis of the leg: a case-control study. Dermatology 209: 301-317.
- Sahoo AK, Mahajan R (2016) Management of tinea corporis, tinea cruris, and tinea pedis: A comprehensive review. Indian Dermatol Online J 7: 77-86.
- Ankad BS, Mukherjee SS, Nikam BP, Reshme AS, Sakhare PS, et al. (2020) Dermoscopic Characterization of Dermatophytosis: A Preliminary Observation. Indian Dermatol Online J 11: 202-207.
Citation: Ankad BS, Koti VR (2022) Applicability of Dermoscopy in the Atypical Presentation of Tinea Pedis: A Case Report. J Clin Dermatol Ther 8: 0101.
Copyright: © 2022 Balachandra S Ankad, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

