
Arteriovenous Ulcers: The Mixed Ulcers - Still the Domain of Arterial Therapy? A Case Report
*Corresponding Author(s):
Ulf Th ZierauSaphenion Vein Care Centers, Berlin, Germany
Tel:+049 1708302447,
Email:dr.zierau@yahoo.de
Abstract
In western countries, 2% of people suffer from an open leg ulcer on the lower leg - in about 55% venous insufficiency (varicose veins) is the main cause of wound healing disorder (leg ulcers).
The term leg ulcer describes an ulcer, the is located on the lower leg. In Germany, at least 1 million people have or had a leg ulcer of various origins. It represents the endpoint of Chronic Venous Insufficiency (CVI) [1-7].
The Gold Standard of diagnostics is color duplex ultrasound diagnostics. With this, the superficial veins and the connecting veins to the deep venous system can be found very safe and pathological blood flow can be represented [1,2,4,5,8-10].
In addition to the surgical cleaning of the ulcer and the subsequent compression therapy, an operative rehabilitation of the defective skin vein system is essential. After radical surgical removal of all defective skin veins (Babcock-OP = stripping) since 1907, catheter-assisted procedures such as laser and radiofrequency ablation and microfoam occlusion have complemented radical surgery therapy and pushed it into the second row for more than 18 years [1-5,7,8,11,8, 10,12,13].
INTRODUCTION
Patients suffering from mixed atherovenous leg ulcers often linger long unsuccessful in the treatment of general practitioners and medical specialists. Often months or even years of therapy attempts remain frustration for doctors and patients. The crux is unfortunately still today in the cardinal error, the wound is often seen as a purely external problem, and vascular diagnosis of the arteries and veins depends only at the end of the diagnostic chain.
Long time passes with the conservative therapy with various ointments, wound dressings etc. without the basic illnesses, which led to the Ulcus, to consider [4,8-10,13,14-16].
The specific problem with the ulcus mixtum is the lack of a spontaneous healing tendency or in the opposite treatment approaches for the arterial portion of the disease and the venous part [4, 5,14-16].
The basic principle of therapy is still today the primacy of arterial rehabilitation. A venous restoration as a first therapeutic measure is taboo since in all common procedures (stripping, laser, radio wave, SONOVEIN, microfoam) because a post-operative compression therapy is necessary. However, this is completely contraindicated in the presence of an arterial circulatory disorder. A venous restoration after the opening of the beck arteries / leg arteries is common in only a few cases. At most, compression therapy is recommended [1, 2, 4,5,7,10,15,16,7].
The specific problem with the ulcus cruris mixtum is the lack of a spontaneous healing tendency or in the opposite treatment approaches for the arterial part of the disease and the venous part. The author, too, was trained with this paradigm of vascular surgery and has practiced this for years.
Glue approved for treatment of varicose veins in 2011. Glue is non thermal, non zumescent and normally don‘t need compression therapy. So we can say-the glue therapy of varicose veins can change the therapy concept of mixed - arteriovenous - ulcers [3, 5,14,17,18,]. We would like to describe the case of an 89 year old patient, in which we first remedied the venous problem of truncal varicous veins before the pelvic and leg arteries were repaired.
CASUISTRY
Vein glue for therapy of ulcus cruris?
The vein glue is also ideal for the treatment of chronic venous insufficiency with ulceration (CVI stage 5-6).
In our own practical work, we have seen in the last 8 years 16 patients with Chronic Venous Insufficiency CVI stage 5 - 6 (open leg). They were treated with VenaSeal glue and Sealing Microfoam achieved in all cases rapid healing of the venous leg ulcers (Figure 1)[3,5,14].

Figure 1: SaphenionScience - Arteriovenous Ulcer: 89-year-old patient with pelvic artery occlusion left and bilateral occlusions of the femoral - / lower leg arteries.
Casuistry of mixed arteriovenous ulcer
Our 89-year-old patient, As an example, we would like to present a case that has just passed a few weeks ago. An old man came 10 weeks ago to our center to present the GSV varicose veins on both legs, which were closed several times with a superficial thrombosis (Figure 2). The patient was on oral anticoagulants. On the left big toe, we found an ulcer, further tension bubbles and weakened peripheral arterial pulses. The trunk veins were palpable and partly brownish color (Figure 3).
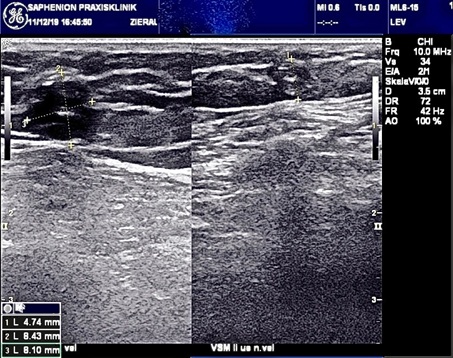
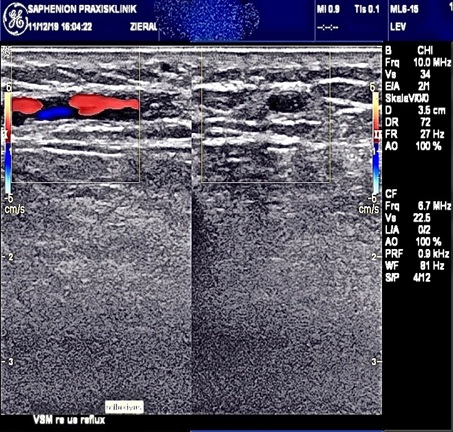
Figure 2: Duplex ultrasound truncal varicose veins both legs - residuals of phlebitis.



Figure 3: Arteriovenous Ulcer: Patient with a blistering and ulcer on the D.p.1 left leg with pelvic / femoral artery occlusion and truncal varicose veins of both GSV and condition after multiple superficial thrombophlebitis - VenaSeal both GSV. VenaSeal - Catheter inside GSV.
After specifying the pain symptoms and taking into account the long history, a Doppler/Duplex sonographic examination of the pelvic/leg arteries and leg veins was carried out. The result showed several artery occlusions on both legs and a pronounced truncal varicose vein of GSV on both legs and a SSV on left leg. There was also sciatic back/leg pain (Figures 1&2).
Postphlebitic truncal varicose veins were detectable in the sonogram (Figure 2). The pain in the lumbar vertebrae and legs was defined with a contrast agent MRI as metastases of an unknown tumor and as multiple occlusion of the pelvic and leg arteries (Figure 1).
Nearly 6 weeks after varicose vein ablation of all 3 truncal veins simultaneously and following the PTA we have examined the old patient. The mixed ulcer left leg was healed (Figure 4).

Figure 4: Clinical aspect 4 weeks after vascular therapy.
The clinical picture is to be seen in the pictures below:
ARTERIOVENOUS ULCER: OUR THERAPY RECOMMENDATION
Our therapy recommendation included the entire range of the diseases identified. This includes the rehabilitation of the arteries - if possible as a PTA (Figure 5) - and the therapy of truncal varicose veins endovenously using endovenous nonthermal, nontumescent technology (Figure 3). It was also important to us that post-operative compression therapy after endovenous therapy is not necessary.
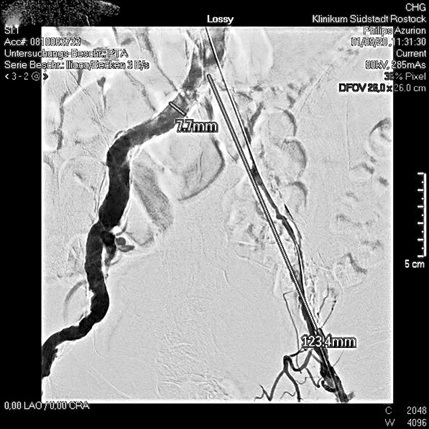
Figure 5: PTA of both pelvic arteries.
At the same time, the metastasis of the lumbal spine, which has now been verified as the cause of prostate carcinoma, must be discussed in the medical council.
In view of the advanced stage of the skin changes on the leg and the recurrent venous thrombosis of the cutaneous veins, we decided, in this case, to first carry out the veins simultaneously without anesthesia and while continuing the antithrombotic medication. This procedure was also necessary with the appointment for arterial therapy since there will still be a few days waiting before the admission date (Figure 6).
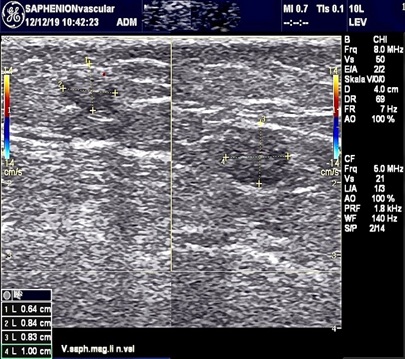
Figure 6: Ultrasound control after sealing both GSV and both SSV with VenaSeal®.
It was also important to us that the mentally fresh elderly patient initially had a thinking time of 6 weeks to be able to think through and discuss the whole complex event. Years had passed without a therapy recommendation for vascular diseases [4,5,14-16).
ARTERIOVENOUS ULCERS: OUR CONCLUSION
When overcoming the diagnostic hurdle of clarifying the multifactorial ulcer genesis - the therapy is often lengthy and the treating doctor has to “stay tuned“. There are valid data on the need for arterial AND venous reconstruction concerning the expected ulcer healing: An arterial intervention + varicose therapy -> 95% healing. An arterial intervention + PTS after TVT -> 41% dep. (but: 13% amputation rate!).
Without arterial reconstruction (+ all vein disorders) -> 0% (25% amputations !!).
WHAT IS NEW IN THIS CONTEXT?
Is that: varicose vein therapy no longer has to be at the back. There we have now non thermal procedures that can be performed minimally invasively, without anesthesia and without compression therapy, which is normally necessary [4,5,10].
Our case description shows for the first time the possibility that the venous component of an arteriovenous ulcer can be carried out simultaneously or BEFORE arterial therapy. This fact has not previously been discussed in the international discussion of non-thermal, nontumescent non compression pathways on varicose veins.
Furthermore, the pathophysiology of high venous pressure should be weighted differently if there is low arterial blood flow to the legs. In our opinion, this venous high pressure in the system of muscle capillaries plays a much larger role in reducing the oxygen supply than previously discussed. From this, however, a significant reduction in the venous high pressure is also crucial for a successful improvement in arterial blood flow.
However, this is not possible with compression therapy alone. Existing truncal varicose veins should definitely be treated as well.
From this perspective, the use of minimally invasive nonthermal, nontumescent and non compression therapy in varicose vein treatment is a decisive advantage. The development of so-called nonthermal therapy methods (e.g. vein glue) also allows primary outpatient treatment of varicose vein diseases in the complex of causes of arteriovenous ulcers in the often elderly and old patients [4,5,9,15].
CONFLICT OF INTERESTS
There are no conflicts of interest; the present research paper was not sponsored
REFERENCES
- AWMF (2020) Leitlinien. Berlin, Germany.
- https://www.derma.de/de/daten/leitlinien/leitlinien/ulcus-cruris-venosum/
- Hach W, et al. (2006) Venen Chirurgie. Schattauer GmbH, Stuttgart, Germany.
- http://www.saphenion.de/news/venenkleber-beim-offenen-bein-sealing-veins-in-ulcera-crures-update3 /?preview_id=8666&preview_nonce=07928588b5&preview=true&_thumbnail_id=10349
- Zierau UT (2020) SaphenionScience - Arteriovenous Ulcers: Against all odds. Practice for vascular diseases and venous center, Germany.
- Jürgen W, Robert M (1990) Funktionelle Phlebologie. Georg Thieme Verlag, Stuttgart, Germany.
- Wuppermann T (1986) Varizen, Ulcus cruris und Thrombose. Springer-Verlag Berlin and Heidelberg GmbH & Co. KG, Heidelberg, Germany.
- Fellmann L, Stadelmann E (2014) Venous ulcus cruris: the higher the pressure, the better the healing. Krankenpfl Soins Infirm 107: 30-31.
- Ghauri AS, Nyamekye I, Grabs AJ, Farndon JR, Poskitt KR (1998) The diagnosis and management of mixed arterial/venous leg ulcers in community-based clinics. Eur J Vasc Endovasc Surg, 16: 350-355.
- https://phlebology.de/leitlinien-der-dgp-mainmenu/archiv/6-leitlinie-diagnostik-und-therapie-des-ulcus-cruris-venosum-kurzfassung
- https://eurocom-info.de/wp-content/uploads/2015/11/eurocom_aktuell_08_2012.pdf.
- Kalinin RE, Suchkov IA, Shanaev IN (2016) Errors in crural perforant veins ligation. Khirurgiia (Mosk) Vol: 45-48.
- Münter KC (2005) Ulcus cruris venosum--therapeutic principles. MMW Fortschr Med. 147: 41-42.
- http://www.saphenion.de/news/saphenionscience-muskelvenenkrampfadern-und schaufensterkrankheit/
- Treiman GS, Copland S, McNamara RM, Yellin AE, Schneider PA, et al. (2001) Factors influencing ulcer healing in patients with combined arterial and venous insufficiency. J Vasc Surg 33: 1158-1164.
- Wollina U, Heinig B, Stelzner C, Hansel G, Schönlebe J, et al. (2018) The Role of Complex Treatment in Mixed Leg Ulcers - A Case Report of Vascular, Surgical and Physical Therapy. Open Access Maced J Med Sci 6: 67-70.
- Zierau UT (2019) SaphenionScience: Muscle vein varicosis and intermittend claudicatio disorder – real risk for arteries? Practice for vascular diseases and venous center, Germany.
- Zierau UT (2019) SaphenionScience: muscle vein foot varicose veins. Practice for vascular diseases and venous center, Germany.
Citation: Zierau UT, Martell L, Lahl W (2020) Arteriovenous Ulcers: The Mixed Ulcers - Still the Domain of Arterial Therapy? A Case Report. J Clin Stud Med Case Rep 7: 082.
Copyright: © 2020 Ulf Th Zierau, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

