
Association of Self-Report and Performance-Based Instruments to Measure Functional Performance among Wheelchair Users
*Corresponding Author(s):
Hassan Izzeddin Sarsak (PhD, OT)Department Of Occupational Therapy, Batterjee Medical College, PO Box 6231 Jeddah 21442 KSA, Saudi Arabia
Email:hassan.sarsak@bmc.edu.sa
Abstract
The main objective of this study was to investigate associations of self-report and performance-based measures of functional performance for wheelchair users.
Method
The Functioning Everyday with a Wheelchair (FEW); a self-report measure, the FEW-Capacity (FEW-C); a performance-based measure for the clinic, and the FEW-Performance (FEW-P); a performance-based measure that measures clients’ skills in the home were the measures used in this study. The current study examines the associations among the different methods used with the FEW, FEW-C and FEW-P at pretest when participants used their customary wheel chairs and post test when participants used their new wheelchairs.
Results
Our hypothesis that there would be a stronger association between the FEW, FEW-C, and FEW-P at the pretest than the posttest due to the familiarity with the wheeled mobility device was partially confirmed. Overall, the relationships among the self-report (FEW) and the performance-based (FEW-C, FEW-P) total independence scores were significantly associated at both pretest and posttest as were the relationships between the two performance-based tools. However, these significant relationships were stronger at the pretest compared to the posttest.
Conclusion
Our hypothesis that there would be a stronger association between the FEW, FEW-C and FEW-P at the pretest when compared with the posttest was accepted for the total scores but was only partially confirmed for the individual items of these tools. Our findings indicate that both methods (self-report and performance-based) can yield useful information, may have potential roles in clinical and research settings, and may have complementary relationships.
Keywords
Association; FEW; Functional Performance; Performance-based; Self-report; Wheelchair Users
BACKGROUND
The extent of agreement between subjective self-report methods and objective performance methods remains an open question. For example, in a recent study, Rushton, Kirby and Miller hypothesized that the total scores of the Wheelchair Skills Test (WST) version 4.1, an observer-rated scale of wheelchair performance and the Wheelchair Skills Test Questionnaire (WST-Q) version 4.1 capacity score (can you do this skill?), a self-report of wheelchair skills, were highly correlated [2,9,10]. They had a sample of 89 community-dwelling, experienced manual wheelchair users ranging in age from 21 to 94 years. Participants used their own manual wheelchairs and the WST was conducted in one testing session following completion of the WST-Q. They found that the WST and WST-Q capacity total scores were highly correlated (rs = .89, p = 0.000), with the WST-Q scores slightly higher due to what the authors attributed to over-estimation of participant self-reports. For the 32 individual skills, the percent agreement between the WST and WST-Q capacity scores ranged from 82% to 100% [2]. Another study, using the same instruments, tested the hypothesis that therapists’ estimates of clients’ abilities to perform manual wheelchair skills accurately reflected the results from objective testing. Twenty-four hours prior to viewing videotapes of their clients’ WST, occupational therapists were asked to provide a global assessment of their clients’ manual wheelchair skills using a 100-mm visual analog scale. The therapists then viewed the videotapes of their clients (n = 66) and scored the WST. Their global estimates were then correlated with the users’ WST capacity scores (version 2.4) [11]. The results indicated only fair correlations between therapists’ estimates and wheelchair users’ WST scores (rs = 0.39, p value not reported). Verbal reports by therapists about the clinical utility of the objective WST, however, were quite positive. Because perceptions of the therapists were only fairly correlated with the wheelchair users’ objective performance skills, the authors noted that the therapists believed that use of the objective WST for training as well as assessment would be preferred. They found that objective measurement was especially important when assessment of specific manual wheelchair skills is required (e.g., moving the armrests away, reaching a high object, transferring out of and into the wheelchair, folding the wheelchair, and negotiation of irregular surfaces) in addition to propulsion.
Some may assume that objective methods of assessing wheelchair skills are more valid than subjective methods, but it is important to recognize that the converse could be true. If the wheelchair users experienced anxiety during objective performance testing, if they were tired or unwell, or if the test environment did not closely mirror the wheelchair users’ usual settings, the assessment may not have been valid. Therefore, the extent and nature of subjective-objective associations, and any bias based on method of assessment, should be measured rather than assumed [1]. Although many studies have examined associations between subjective and objective methods of assessing the wheelchair skills (e.g., propulsion, wheelies) of persons who use wheeled mobility devices, few have examined the associations between subjective and objective methods used to assess the ability of wheelchair users to carry out everyday activities with their wheelchairs [1,2,8]. Because subjective and objective wheeled mobility assessments differ in the amount of time and resources needed, it is important to evaluate their associations to determine if the methods of assessment are interchangeable and if associations remain stable from pretest to posttest. Therefore, this study focuses on examining associations between subjective and objective methods of data collection for documenting the everyday functional task performance of persons who use wheelchairs.
The specific aim of this study was to examine the associations among three tools which were used to assess task independence of wheelchair users by different methods: self-report (Functioning Everyday with a Wheelchair Beta Version 2.0 (FEW), clinic performance (Functioning Everyday with a Wheelchair - Capacity (FEW-C), and home performance (Functioning Everyday with a Wheelchair - Performance (FEW-P), before and following the provision of a new wheelchair provided by a qualified interdisciplinary team of clinicians. The FEW, FEW-C and FEW-P are used to assess a wheelchair user’s independence in performing nine tasks: ability to adjust wheelchair to meet comfort needs, ability to carry out health maintenance in the wheelchair, ability to operate the wheelchair, ability to reach various surface heights from the wheelchair, ability to transfer to various surface heights from the wheelchair, ability to perform personal care tasks from the wheelchair, ability to manage indoor mobility with the wheelchair, ability to manage outdoor mobility in the wheelchair, and ability to access personal and public transportation with the wheelchair. Clinically, given limited healthcare resources, our findings may provide guidance as to which methods are interchangeable for which items during the initial wheeled mobility assessment, and likewise for measuring outcomes after provision of the wheeled mobility device.
Why the FEW instruments were selected for this study
In response to the need for more comprehensive outcome measures to document function for third-party payers, and evaluate the efficacy of wheeled mobility interventions, a team of researchers at the University of Pittsburgh developed the FEW (a self-report measure), the FEW-Capacity (FEW-C, a performance-based measure for the clinic), and the FEW-Performance (FEW-P, a performance-based measure for the home) outcome measurement instruments. The FEW-C and FEW-P were structured after the Performance Assessment of Self-Care Skills (PASS) because of its measurement parameters (independence, safety, and adequacy) and its focus on four domains of functioning: Functional Mobility (FM), Activities of Daily Living (ADL) including self-care, Instrumental ADL (IADL) with a physical emphasis (PIADL), and IADL with a cognitive emphasis (CIADL).
The trio of FEW tools has been used in research and proved to be reliable, valid, and useful [6,7,14-17]. A study of 25 subjects showed that both the self-report FEW and FEW-C were able to detect significant changes in function over time following the provision of a new wheeled mobility and seating device. However, the FEW often significantly under estimated function compared to the FEW-C, and therefore documented greater changes in function over time [7]. Underestimation may have occurred because it is not unusual for individuals who are seeking interventions to underestimate their capabilities to obtain services or products [3]. The FEW tools have been used in telerehabilitation studies and also proved to be reliable and effective in that venue. A study of 98 adults with mobility impairments using wheeled mobility and seating devices (manual wheelchair, power wheelchair, scooter) were tested to determine whether or not the Telerehabilitation (TR) treatment condition at remote clinics was equally effective when compared to the standard In-person (IP) treatment at local clinics. The study findings were based on the level of function the participants showed with their new wheeled mobility and seating devices as measured by using the FEW outcome tool. They found that the telerehabilitation treatment condition was equally effective on all items except for the FEW transportation items [17]. Another study of 46 subjects with mobility impairments using wheeled mobility and seating devices evaluated the interrater reliability between a generalist clinician using the FEW-C In Person (IP) and an expert clinician observing through Telerehabilitation (TR) from a remote clinic. The expert clinician, located more than 100 miles away, was able to accurately evaluate the functional mobility needs of clients being assessed for new mobility devices [16].
Although there are several assessments of wheelchair skills, none address independence, safety and adequacy of performance of everyday tasks with a wheelchair. The FEW, FEW-C and FEW-P were developed to address the need for a more comprehensive assessment and outcomes tool for clients seeking and receiving wheeled mobility devices.
Hypothesis
METHODS
Design
N.B. FEW: The Functioning Everyday with a Wheelchair instrument (the self-report version);
FEW-C: FEW-Capacity (the clinic-version); FEW-P: FEW-Performance (the home-version)
Participants
Participants for the current study were a subset of participants from the studies by Mills and Schmeler [6,7]. The inclusion criteria for participants recruited for these studies were (a) existing manual/power wheelchair or scooter user, who had experienced a change in functional status; (b) 18 years of age or older; and (c) adequate cognitive and language status, that is participants would be able to understand and verbally respond to questions and carry out the tasks in the FEW, FEW-C and FEW-P. Cognition and language status were determined by information provided by team members from the Center for Assistive Technology (CAT) and the Center for Assistive and Rehabilitative Technology (CART). Although informed consent was obtained from 25 participants, only 19 participants had complete data for all three instruments, and therefore the secondary analyses were conducted with data from those 19 participants.
Instruments
FEW
|
Items/tasks |
|
Stability, Durability, Dependability |
|
Comfort Needs |
|
Health Needs |
|
Operate |
|
Reach |
|
Transfer |
|
Personal Care |
|
Indoor Mobility |
|
Outdoor Mobility |
|
Transportation |
Table 1: Items of the FEW, FEW-C, and FEW-P.
The FEW-C is a performance-based observation tool, for use by clinicians and researchers to measure functional outcomes of wheelchair and seating interventions in the clinical setting. Items 2 - 10 were structured using the criterion-referenced approach of the Performance Assessment of Self-Care Skills (PASS) [18,19] and designed to match the items of the FEW. The FEW-C was designed to measure function based on the International Classification of Functioning, Disability and Health (ICF) construct of capacity, namely, a person’s ability to execute a task under standardized conditions [20]. The FEW-C has demonstrated excellent interrater reliability (ICC = 0.99), excellent internal consistency (α = 0.97), and fair to good convergent validity when compared with tools measuring similar traits (e.g., the FEW, and the Functional Abilities in a Wheelchair (FAW) tools) by different methods [7].
The FEW-P is a performance-based observation tool, for use by clinicians and researchers to measure functional outcomes of seating and wheeled mobility interventions in the home/community. Items 2 - 10 are performance-based, as in the FEW-C. The FEW-P was designed to measure function based on the ICF construct of performance in the “lived in” environment [20]. The FEW-P has demonstrated excellent inter-rater reliability and internal consistency (α = 0.95) [6].
Summary scores are based on a predefined 4-point ordinal scale for independence and scores are hierarchical, ranging from 3 (no assists given for task initiation, continuation, completion) to 0 (three physical assists or total assistance given for task initiation, continuation, or completion) [6,7] (Table 2). For each item, the assessor observes the wheelchair user perform the task and rates the level of independence based on the type and number of assists given. The manual provides detailed information on the administration, scoring and interpretation for each item [6].
|
Score |
Independence data |
|
3 |
No assists |
|
2 |
No physical assists; Occasional verbal and/or Visual assists |
|
1 |
Occasional physical assists; Continuous verbal and/or Visual assists |
|
0 |
Continuous physical assists; Total assistance |
Table 2: Summary independence scores of the FEW-C and FEW-P.
PROCEDURES
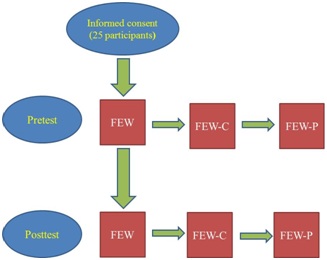
Participants were assessed with their current wheelchairs at pretest, and later at posttest when they received their new wheelchairs. The FEW was administered first followed by the FEW-C and the FEW-P (Figure 2). Mean duration between pretest and posttest for the three tools was 57 days (SD ± 46) with a median of 44 days and a range from 9 to 189 days. Time between pretest and posttest assessments varied based on insurance funding, transportation resources to the clinic, and the duration the participants had to wait to get their new wheelchairs. Participants had to have their new mobility device a minimum of 2 weeks before the posttest.
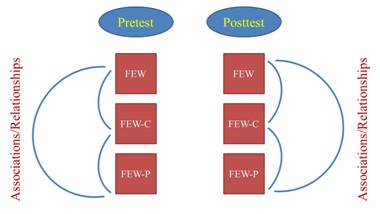 Figure 2: Association of the FEW, FEW-C and FEW-P instruments at pretest and posttest.
Figure 2: Association of the FEW, FEW-C and FEW-P instruments at pretest and posttest.N.B. FEW: The Functioning Everyday with a Wheelchair instrument (the self-report version);
FEW-C: FEW-Capacity (the clinic-version); FEW-P: FEW-Performance (the home-version)
The FEW and FEW-C pretest assessments occurred on a regularly scheduled clinic visit for a seating evaluation, followed by the FEW-P (home) assessment within 1 week. The posttest assessments occurred in the same sequence (FEW, FEW-C, FEW-P) after receiving the new wheelchair [6,7]. A fixed rather than a random order of assessment methods was followed, with self-report before performance because perceptions (self-reports) are more likely to be biased by performance than the reverse.
Data analysis
We then examined the associations among the total scores and the items of the FEW, FEW-C and FEW-P at pretest and posttest (Figure 2) using Spearman correlation coefficients. As a general guideline, correlations ranging from 0.00 to 0.25 indicate a poor relationship; those from 0.26 to 0.50 suggest a fair degree of relationship; values of 0.51 to 0.75 are moderate; and values that are 0.76 and above are considered excellent [21]. We defined statistical significance as p < .05. Given our small sample size and adjustment was not applied for multiple correlations.
RESULTS
Participants
|
Demographics |
Mean (SD) [range] |
n |
|
Age (mean, SD) [range] |
53.1 (± 11.0) [36 - 72] |
|
|
Gender |
||
|
Male (n) |
9 |
|
|
Female (n) |
10 |
|
|
Race |
||
|
Caucasian (n) |
17 |
|
|
African American (n) |
2 |
|
|
Years using a wheelchair (mean, SD) |
9.5 (± 11.3) [1 - 45] |
|
|
Age of current wheelchair (mean, SD) |
3.74 (± 2.5) [1 - 9] |
|
|
Number of wheelchairs owned currently |
||
|
1 (n) |
11 |
|
|
2 (n) |
7 |
|
|
3 (n) |
1 |
|
|
Primary medical condition |
||
|
Above Knee Amputation (n) |
1 |
|
|
Cardiac Disease (n) |
1 |
|
|
Cerebral Palsy (n) |
1 |
|
|
Cerebral Vascular Accident (n) |
2 |
|
|
Lupus (n) |
1 |
|
|
Mitochondrial Disease (n) |
1 |
|
|
Multiple Sclerosis (n) |
7 |
|
|
Orthopedic Disorder (n) |
1 |
|
|
Parkinson Disease (n) |
1 |
|
|
Spina Bifida (n) |
2 |
|
|
Traumatic Brain Injury (n) |
1 |
|
At pretest, 3 of the wheelchairs were power and 16 were manual. The manual wheelchairs, on average, were 3.7 years old with sling seats (n = 15), and no seat functions other than manual elevating leg rests. At posttest, all wheelchairs used by the participants were power chairs. The power wheelchairs were equipped with power elevating foot supports (n = 10), full-length adjustable height arm supports (n = 10), and multiple seat functions (n = 9) (Tables 4 and 5 for detailed characteristics of the participants’ wheelchairs).
|
Characteristics |
Pretest |
Posttest |
|
Type of wheelchair |
||
|
Manual |
16 |
0 |
|
Power |
3 |
19 |
|
Scooter |
0 |
0 |
|
Weight of manual wheelchairs |
||
|
Standard |
8 |
0 |
|
Lightweight |
3 |
0 |
|
High strength lightweight |
4 |
0 |
|
Ultra-lightweight |
1 |
0 |
|
Power wheelchair |
||
|
Front-wheel drive |
1 |
9 |
|
Mid-wheel drive |
1 |
6 |
|
Rear-wheel drive |
1 |
2 |
|
Missing data |
0 |
2 |
|
Characteristics |
Pretest |
Posttest |
|
Back supports |
||
|
Sling upholstery |
15 |
0 |
|
Adjustable tension back |
1 |
1 |
|
Rigid back |
1 |
8 |
|
Custom-contoured back |
0 |
2 |
|
Captain-style seat |
1 |
3 |
|
Foot supports |
||
|
Power elevating |
0 |
10 |
|
Manual elevating |
7 |
1 |
|
Fixed |
1 |
3 |
|
Swing-away |
7 |
2 |
|
Flip-up |
1 |
4 |
|
Removable |
3 |
1 |
|
Arm supports |
||
|
Full-length, fixed height |
6 |
0 |
|
Full-length, adjustable height |
1 |
10 |
|
Desk-length, fixed height |
6 |
2 |
|
Desk-length, adjustable height |
3 |
3 |
|
Swing-away |
0 |
3 |
|
Flip-up |
4 |
9 |
|
Removable |
5 |
0 |
|
Other (e.g. front anti-tippers) |
3 |
0 |
|
Seatbelt |
||
|
Yes |
1 |
1 |
|
No |
18 |
18 |
|
Seat functions |
||
|
Power tilt in space only |
1 |
3 |
|
Power reclining backrest only |
0 |
0 |
|
Power seat elevator only |
1 |
1 |
|
Tilt-in-space and reclining back only |
0 |
1 |
|
All of the above |
0 |
9 |
|
All of the above plus passive standing |
0 |
1 |
Descriptive statistics (FEW, FEW-C, FEW-P)
|
Tool |
Pretest |
95% CI |
Posttest |
95% CI |
|
FEW |
1.35 ± 0.67 (0.00-2.44) |
[1.04, 1.70] |
2.43 ± 0.36 (1.67-3.00) |
[2.26, 2.61] |
|
FEW-C |
1.90 ± 0.74 (0.17-2.91) |
[1.55, 2.27] |
2.59 ± 0.32 (1.67-3.00) |
[2.43, 2.74] |
|
FEW-P |
2.12 ± 0.67 (0.59-3.00) |
[1.80, 2.44] |
2.45 ± 0.43 (1.39-3.00) |
[2.25, 2.66] |
|
Item |
Pretest |
95% CI |
Posttest |
95% CI |
|
FEW |
|
|||
|
Comfort |
1.47 ± 0.96 (0.00-3.00) |
[1.01, 1.94] |
2.68 ± 0.48 (2.00-3.00) |
[2.45, 2.91] |
|
Health |
1.47 ± 0.96 (0.00-3.00) |
[1.01, 1.94] |
2.74 ± 0.56 (1.00-3.00) |
[2.50, 3.01] |
|
Operate |
1.32 ± 1.11 (0.00-3.00) |
[0.78, 1.85] |
2.68 ± 0.48 (2.00-3.00) |
[2.45, 2.91] |
|
Reach |
0.74 ± 0.93 (0.00-2.00) |
[0.29, 1.20] |
2.00 ± 1.05 (0.00-3.00) |
[1.50, 2.51] |
|
Transfer |
1.74 ± 1.10 (0.00-3.00) |
[1.21, 2.27] |
2.37 ± 1.01 (0.00-3.00) |
[1.88, 2.86] |
|
Personal Care |
1.63 ± 1.12 (0.00-3.00) |
[1.10, 2.17] |
2.21 ± 0.92 (0.00-3.00) |
[1.77, 2.65] |
|
Indoor |
1.63 ± 1.01 (0.00-3.00) |
[1.14, 2.12] |
2.58 ± 0.61 (1.00-3.00) |
[2.30, 2.87] |
|
Outdoor |
0.74 ± 0.87 (0.00-3.00) |
[0.32, 1.16] |
2.53 ± 0.96 (0.00-3.00) |
[2.10, 2.99] |
|
Transportation |
1.47 ± 1.22 (0.00-3.00) |
[0.89, 2.10] |
2.11 ± 1.20 (0.00-3.00) |
[1.53, 2.68] |
|
FEW-C |
|
|||
|
Comfort |
2.29 ± 0.92 (0.00-3.00) |
[1.85, 2.73] |
2.89 ± 0.27 (2.00-3.00) |
[2.77, 3.02] |
|
Health |
2.37 ± 0.75 (1.00-3.00) |
[2.01, 2.73] |
2.83 ± 0.41 (1.33-3.00) |
[2.63, 3.03] |
|
Operate |
2.29 ± 1.13 (0.00-3.00) |
[1.74, 2.83] |
2.95 ± 0.18 (2.25-3.00) |
[2.86, 3.03] |
|
Reach |
2.26 ± 1.15 (0.00-3.00) |
[1.71, 2.82] |
2.71 ± 0.45 (1.67-3.00) |
[2.49, 2.93] |
|
Transfer |
1.66 ± 1.32 (0.00-3.00) |
[1.02, 2.29] |
2.13 ± 0.97 (0.00-3.00) |
[1.66, 2.60] |
|
Personal Care |
2.30 ± 0.94 (0.00-3.00) |
[1.84, 2.75] |
2.56 ± 0.76 (0.00-3.00) |
[2.19, 2.93] |
|
Indoor |
2.21 ± 1.04 (0.00-3.00) |
[1.71, 2.71] |
2.89 ± 0.23 (2.25-3.00) |
[2.79, 3.00] |
|
Outdoor |
0.78 ± 1.19 (0.00-3.00) |
[0.19, 1.37] |
2.88 ± 0.26 (2.00-3.00) |
[2.76, 3.00] |
|
Transportation |
0.87 ± 1.12 (0.00-3.00) |
[0.31, 1.43] |
1.30 ± 1.27 (0.00-3.00) |
[0.65, 1.96] |
|
FEW-P |
|
|||
|
Comfort |
2.50 ± 0.78 (0.00-3.00) |
[2.12, 2.88] |
2.82 ± 0.42 (1.50-3.00) |
[2.62, 3.02] |
|
Health |
2.40 ± 0.86 (0.00-3.00) |
[1.99, 2.82] |
2.78 ± 0.45 (1.50-3.00) |
[2.57, 2.99] |
|
Operate |
2.61 ± 0.84 (0.00-3.00) |
[2.20, 3.01] |
2.61 ± 0.84 (0.00-3.00) |
[2.20, 3.01] |
|
Reach |
2.75 ± 0.58 (0.67-3.00) |
[2.48, 3.03] |
2.75 ± 0.58 (0.67-3.00) |
[2.48, 3.03] |
|
Transfer |
1.79 ± 1.24 (0.00-3.00) |
[1.19, 2.39] |
2.05 ± 1.18 (0.00-3.00) |
[1.49, 2.62] |
|
Personal Care |
2.46 ± 0.83 (0.00-3.00) |
[2.06, 2.86] |
2.46 ± 0.75 (0.33-3.00) |
[2.10, 2.82] |
|
Indoor |
2.33 ± 1.01 (0.00-3.00) |
[1.84, 2.81] |
2.79 ± 0.44 (1.50-3.00) |
[2.58, 3.00] |
|
Outdoor |
0.91 ± 1.19 (0.00-3.00) |
[0.34, 1.48] |
2.32 ± 1.08 (0.00-3.00) |
[1.80, 2.84] |
|
Transportation |
0.81 ± 1.24 (0.00-3.00) |
[0.02, 1.59] |
0.97 ± 1.23 (0.00-3.00) |
[0.23, 1.72] |
Relationships among the FEW, FEW-C, and FEW-P at pretest and posttest
|
Tool |
Pre FEW |
Pre FEW-C |
Tool |
Post FEW |
Post FEW-C |
||
|
Pre |
FEW |
--- |
Post |
FEW |
--- |
||
|
Pre |
FEW-C |
0.69** |
--- |
Post |
FEW-C |
0.61** |
--- |
|
Pre |
FEW-P |
0.76** |
0.64** |
Post |
FEW-P |
0.47* |
0.63** |
The Spearman’s rho correlation coefficients for the individual items indicated that 16 correlations were stronger at pretest than posttest, and 11 were stronger at posttest than pretest. At pretest, the relationships among all three tools were stronger than at posttest for Indoor Mobility and Outdoor Mobility, but all three were significant only for Outdoor Mobility. At posttest, the relationships among the three tools were stronger than at pretest for Comfort Needs and Transportation, but all three were significant only for transportation (Tables 9-17). At pretest, no significant relationships among the three tools were found for Comfort Needs or Transportation, and at posttest, no significant relationships were found for Operate, Reach, Indoor Mobility or Outdoor Mobility.
|
Tool |
Pre FEW |
Pre FEW-C |
Tool |
Post FEW |
Post FEW-C |
||
|
Pre |
FEW |
--- |
Post |
FEW |
--- |
||
|
Pre |
FEW-C |
-0.06 |
--- |
Post |
FEW-C |
-0.29 |
--- |
|
Pre |
FEW-P |
0.02 |
0.39 |
Post |
FEW-P |
-0.1 |
0.87** |
|
Tool |
Pre FEW |
Pre FEW-C |
Tool |
Post FEW |
Post FEW-C |
||
|
Pre |
FEW |
--- |
Post |
FEW |
--- |
||
|
Pre |
FEW-C |
0.44 |
--- |
Post |
FEW-C |
0.05 |
--- |
|
Pre |
FEW-P |
0.36 |
0.59** |
Post |
FEW-P |
0-0.07 |
0.63** |
|
Tool |
Pre FEW |
Pre FEW-C |
Tool |
Post FEW |
Post FEW-C |
||
|
Pre |
FEW |
--- |
Post |
FEW |
--- |
||
|
Pre |
FEW-C |
0.67** |
--- |
Post |
FEW-C |
0.16 |
--- |
|
Pre |
FEW-P |
0.52* |
0.3 |
Post |
FEW-P |
0.46 |
0.37 |
Table 11: Relationships among the FEW, FEW-C, and FEW-P for Operate at pretest and posttest.
Note: Pre = Pretest. Post = Posttest. Number of participants (N=19). * p < .05. ** p <.01
|
Tool |
Pre FEW |
Pre FEW-C |
Tool |
Post FEW |
Post FEW-C |
||
|
Pre |
FEW |
--- |
Post |
FEW |
--- |
||
|
Pre |
FEW-C |
0.46* |
--- |
Post |
FEW-C |
-0.02 |
--- |
|
Pre |
FEW-P |
0.06 |
0.60** |
Post |
FEW-P |
-0.18 |
0.09 |
Table 12: Relationships among the FEW, FEW-C, and FEW-P for Reach at pretest and posttest
Note: Pre = Pretest. Post = Posttest. Number of participants (N=19). * p < .05. ** p <.01
|
|
Tool |
Pre FEW |
Pre FEW-C |
|
Tool |
Post FEW |
Post FEW-C |
|
Pre |
FEW |
--- |
Post |
FEW |
--- |
||
|
Pre |
FEW-C |
0.68** |
--- |
Post |
FEW-C |
0.48* |
--- |
|
Pre |
FEW-P |
0.71** |
0.59** |
Post |
FEW-P |
0.62** |
0.62** |
Table 13: Relationships among the FEW, FEW-C and FEW-P for Transfer at pretest and posttest
Note: Pre = Pretest. Post = Posttest. Number of participants (N=19). * p < .05. ** p <.01
|
|
Tool |
Pre FEW |
Pre FEW-C |
|
Tool |
Post FEW |
Post FEW-C |
|
Pre |
FEW |
--- |
Post |
FEW |
--- |
||
|
Pre |
FEW-C |
0.37 |
--- |
Post |
FEW-C |
0.59** |
--- |
|
Pre |
FEW-P |
0.28 |
0.87** |
Post |
FEW-P |
0.17 |
0.38 |
Table 14: Relationships among the FEW, FEW-C, and FEW-P for Personal Care at pretest and posttest.
Note: Pre = Pretest. Post = Posttest. Number of participants (N=19). ** p <.01
|
|
Tool |
Pre FEW |
Pre FEW-C |
Tool |
Post FEW |
Post FEW-C |
|
|
Pre |
FEW |
--- |
Post |
FEW |
--- |
||
|
Pre |
FEW-C |
0.73** |
--- |
Post |
FEW-C |
0.11 |
--- |
|
Pre |
FEW-P |
0.42 |
0.29 |
Post |
FEW-P |
0.21 |
0.26 |
Table 15: Relationships among the FEW, FEW-C, and FEW-P for Indoor Mobility at pretest and posttest.
Note: Pre = Pretest. Post = Posttest. Number of participants (N=19). ** p <.01
|
Tool |
Pre FEW |
Pre FEW-C |
Tool |
Post FEW |
Post FEW-C |
||
|
Pre |
FEW |
--- |
Post |
FEW |
--- |
||
|
Pre |
FEW-C |
0.56*a |
--- |
Post |
FEW-C |
-0.14 |
--- |
|
Pre |
FEW-P |
0.58** |
0.82**b |
Post |
FEW-P |
0.34 |
0.08 |
Table 16: Relationships among the FEW, FEW-C, and FEW-P for Outdoor Mobility at pretest and posttest.
Note: Pre = Pretest. Post = Posttest. Number of participants (N=19). a = number of participants (N=18). b = number of participants (N=18). * p < .05. ** p <.01
|
Tool |
Pre FEW |
Pre FEW-C |
Tool |
Post FEW |
Post FEW-C |
||
|
Pre |
FEW |
--- |
Post |
FEW |
--- |
||
|
Pre |
FEW-C |
0.25a |
--- |
Post |
FEW-C |
0.64**d |
--- |
|
Pre |
FEW-P |
0.38b |
0.58c |
Post |
FEW-P |
0.64*e |
0.81**f |
Table 17: Relationships among the FEW, FEW-C and FEW-P for Transportation at pretest and posttest.
Note: Pre = Pretest. Post = Posttest. a = number of participants (N=18). b = number of participants (N=12). c = number of participants (N=11).d = number of participants (N=17). e = number of participants (N=13). f = number of participants (N=13). * p < .05. ** p <.01
At pretest, four FEW and FEW-C individual items were significantly and moderately correlated with each other, namely, Operate, Transfer, Indoor Mobility, and Outdoor Mobility, and Reach had a significant and fair relationship. For the FEW and FEW-P, only three items were significantly and moderately correlated: Operate, Transfer, and Outdoor Mobility. The FEW-C and FEW-P items of Personal care and Outdoor Mobility were significantly correlated at an excellent level of strength while significant and moderate relationships were found for Health Needs, Reach, and Transfer. The rest of the items were not significantly correlated. At posttest, for the FEW and FEW-C only two individual items were significantly and moderately correlated --- Personal Care, and Transportation, and one item, Transfer, had a significant and fair relationship. For the FEW and FEW-P, only two items were significantly and moderately correlated --- Transfer and Transportation. Four FEW-C and FEW-P individual items were significantly correlated: Comfort Needs and Transportation with excellent relationships, and Health Needs, and Transfer with moderate relationships.
DISCUSSION
Our hypothesis that there would be a stronger association between the FEW, FEW-C and FEW-P at the pretest than the posttest due to the familiarity with the wheeled mobility device was partially confirmed. Overall, the relationships among the self-report (FEW) and the performance-based (FEW-C, FEW-P) total independence scores were significantly associated at both pretest and posttest as were the relationships between the two performance-based tools. However, these significant relationships were stronger at the pretest compared to the posttest.
Although familiarity with their wheeled mobility device could be one explanation for the stronger relationship at pretest, our data suggested another possible explanation. The participants tended to underestimate their capabilities at the pretest self-report compared to pretest performance, which is not unusual for individuals who are seeking interventions to obtain health services or a new product and/or equipment [3,5].
The relationships among individual items of the three tools indicated that for 7 of the 9 items, the mean strength of the relationships among the three tools was greater at pretest than posttest, however 13 of 27 relationships were statistically significant at pretest and 9 of 27 relationships were significant at posttest. This might be due to the fact that 16 of the participants changed from a manual chair to a power chair, and the new power wheelchairs were given to the clients a minimum of 2 weeks before the posttest and they were less familiar with operating them. Only one item, Transfer, had significant relationships among the three tools at both pretest and posttest, and for only one item, Health Needs, relationships were significantly associated among the FEW-C and FEW-P indicating that the two tools had similar ratings regardless of time or the environment.
At pretest, Transfer (moderate relationship) and Outdoor Mobility (moderate to excellent relationship), and at posttest, Transfer (fair to moderate relationships) and Transportation (moderate to excellent relationships), had significant relationships among all three tools, indicating that participant perceptions were significantly associated with their performance in the clinic and the home. In contrast, at pretest, there were no significant relationships among the tools for Transportation, and at posttest there were no significant relationships among the tools for Outdoor Mobility.
It is unclear why Outdoor Mobility would be more strongly associated at pretest, with the majority of subjects using a manual wheelchair, and less so at posttest when all subjects used a power wheelchair, which would require less strength and endurance. Moreover, all wheelchairs were properly fitted as they were prescribed by qualified clinicians. Properly fitted and correctly prescribed wheelchairs benefit the users and aid in provision of the best quality wheelchairs [23-25]. These power wheelchairs were equipped with multiple power seat functions such as seat elevator, tilt in space, and recline or passive standing. Perhaps the complexity and adjustment required to use these wheelchairs might have led to a lower strength of the relationships among the three tools at posttest when compared with pretest where all participants had used more familiar and simpler manual wheelchairs with no seat functions. Additionally, at the pretest, participants did not engage in outdoor mobility activities because their current wheelchairs did not support them. Hence the stronger correlation.
Similarly, it is unclear why perceptions and performance were more strongly associated for Transportation at posttest when a van is needed to transport a power wheelchair versus pretest when a manual wheelchair can be stored in the trunk of a car. However, the Transportation results should be interpreted with caution. The correlations for this specific item might be misrepresented because of the missing data. Several participants were not able to complete all subtasks related to this item due to unavailability of personal and/or public transportation, inability to get the wheelchair out of the house, fatigue, or due to bad weather conditions at the time of the assessment. It is also possible that these new wheelchairs met the participants’ transportation needs and stronger relationships among the three tools at posttest for this item.
For some items at both pretest and posttest, no significant relationships were found among ratings on the three tools. At pretest no significant relationships were found for Comfort Needs and Transportation, and at posttest no significant relationships were found for Operate, Reach, Indoor Mobility or Outdoor Mobility.
Because there are differences in the resources required for self-report versus performance assessments, examining the relationships among the FEW, FEW-C, and FEW-P at two time points has clinical significance. Our findings suggest that asking clients about their independence in Transfer and Outdoor Mobility during an intake interview will be almost as accurate as a performance test, however for Comfort Needs and Transportation, self-report may not be associated with their current performance. Following provision of a wheeled mobility device, for Transfers, our data indicate that self-report of current independence may be just as accurate as performance, and so may self-report of Transportation. However, self-report of independence for Operate, Reach, Indoor Mobility and Outdoor Mobility may not be associated with current performance. Finally, for Health Needs, performance assessment in the clinic was significantly associated with performance in the home, which again could save on resources needed for a home visit.
For some items at both pretest and posttest, no significant relationships were found among ratings on the three tools. At pretest no significant relationships were found for Comfort Needs and Transportation, and at posttest no significant relationships were found for Operate, Reach, Indoor Mobility or Outdoor Mobility.
At pretest, the clinical significance of our findings provides guidance as to which methods are interchangeable for which items. At posttest, the clinical significance of our findings provides guidance as to which items (outcome measures) should be performance tested. Thus, our findings indicate that there are differences in the level of associations among the three methods of assessing wheeled mobility independence, and that the strength of the associations varied by item, time and environment.
STUDY LIMITATIONS AND FUTURE DIRECTIONS
CONCLUSIONS
CONFLICT OF INTERESTS
REFERENCES
- Newton AM, Kirby RL, Macphee AH, Dupuis DJ, Macleod DA (2002) Evaluation of manual wheelchair skills: Is objective testing necessary or would subjective estimates suffice? Arch Phys Med Rehabil 83: 1295-1299.
- Rushton PW, Kirby RL, Miller WC (2012) Manual Wheelchair Skills: Objective testing versus subjective questionnaire. Arch Phys Med Rehabil 93: 2313-2318.
- Cress ME, Schechtman KB, Mulrow CD, Fiatarone MA, Gerety MB, et al. (1995) Relationship between physical performance and self-perceived physical function. J Am Geriatr Soc 43: 93-101.
- Rogers JC, Holm MB (1994) Accepting the challenge of outcome research: Examining the effectiveness of occupational therapy practice. American Journal of Occupational Therapy 48: 871-876.
- Sager MA, Dunham NC, Schwantes A, Mecum L, Halverson K, et al. (1992) Measurement of activities of daily living in hospitalized elderly: A comparison of self-report and performance-based methods. J Am Geriatr Soc 40: 457-462.
- Mills TL (2003) Functioning Every Day with a Wheelchair (FEW): Development and validation of self-report and performance-based observation instruments to measure functional outcomes of seating-mobility interventions Doctoral Dissertation, University of Pittsburgh, Pennsylvania, USA.
- Schmeler M (2005) Development and Testing of a Clinical Outcome Measurement Tool to Assess Wheeled Mobility and Seating Interventions. Doctoral Dissertation, University of Pittsburgh, Pennsylvania, USA.
- Warms CA, Whitney JD, Belza B (2008) Measurement and description of physical activity in adult manual wheelchair users. Disabil Health J 1: 236-244.
- Lindquist NJ, Loudon PE, Magis TF, Rispin JE, Kirby RL, et al. (2010) Reliability of the performance and safety scores of the wheelchair skills test version 4.1 for manual wheelchair users. Arch Phys Med Rehabil 91: 1752-1757.
- Mountain AD, Kirby RL, Smith C (2004) The Wheelchair Skills Test, version 2.4: Validity of an algorithm-based questionnaire version. Arch Phys Med Rehabil 85: 416-423.
- Kirby RL, Dupuis DJ, Macphee AH, Coolen AL, Smith C, et al. (2004) The wheelchair skills test (version 2.4): measurement properties. Arch Phys Med Rehabil 85: 794-804.
- Cress ME, Kinne S, Patrick DL, Maher E (2002) Physical functional performance in persons using a manual wheelchair. J Orthop Sports Phys Ther 32: 104-113.
- Stanley RK, Stafford DJ, Rasch E, Rodgers MM (2003) Development of a functional assessment measure for manual wheelchair users. J Rehabil Res Dev 40: 301-307.
- Mills T, Holm MB, Trefler E, Schmeler M, Fitzgerald S, et al. (2002) Development and consumer validation of the Functional Evaluation in a Wheelchair (FEW) instrument. Disabil Rehabil 24: 38-46.
- Mills TL, Holm MB, Schmeler M (2007) Test-retest reliability and cross validation of the functioning everyday with a wheelchair instrument. Assist Technol 19: 61-77.
- Schein RM, Schmeler MR, Holm MB, Pramuka M, Saptono A, et al. (2011) Telerehabilitation assessment using the Functioning Everyday with a Wheelchair-Capacity instrument. J Rehabil Res Dev 48: 115-124.
- Schein RM, Schmeler MR, Holm MB, Saptono A, Brienza DM (2010) Telerehabilitation wheeled mobility and seating assessments compared with in person. Arch Phys Med Rehabil 91: 874-878.
- Holm MB, Rogers JC (1999) Functional assessment: The Performance Assessment of Self Care Skills (PASS). In: Hemphill-Pearson BJ (ed.). Assessment in Occupational Therapy Mental Health: An Integrative Approach. Slack, Thorofare, USA. Pg no: 431.
- Rogers JC, Holm MB (2014) Performance Assessment of Self-care Skills (PASS). University of Pittsburgh, Pennsylvania, USA.
- World Health Organization (2001) International Classification of Functioning, Disability and Health (ICF). WHO, Geneva, Switzerland.
- Portney LG, Watkins MP (2009) Foundations of clinical research: Applications to practice (3rded.). Upper Saddle River, NJ: Pearson Prentice Hall.
- Rogers H, Berman S, Fails D, Jaser J (2003) A comparison of functional mobility in standard vs. ultralight wheelchairs as measured by performance on a community obstacle course. Disabil Rehabil 25: 1083-1088.
- Brienza D, Kelsey S, Karg P, Allegretti A, Olson M, et al. (2010) A randomized clinical trial on preventing pressure ulcers with wheelchair seat cushions. J Am Geriatr Soc 58: 2308-2314.
- Karmarkar AM, Collins DM, Kelleher A, Cooper RA (2009) Satisfaction related to wheelchair use in older adults in both nursing homes and community dwelling. Disabil Rehabil Assist Technol 4: 337-343.
- Smith C, McCreadie M, Unsworth J (1995) Prescribing wheelchairs: The opinions of wheelchair users and their carers. Clinical Rehabilitation 9: 74-80.
Citation: Sarsak HI (2019) Association of Self-Report and Performance-Based Instruments to Measure Functional Performance among Wheelchair Users. J Phys Med Rehabil Disabil 4: 029.
Copyright: © 2019 Hassan Izzeddin Sarsak (PhD, OT), et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

