
Balloon Assisted Technique in Peripheral Interventions: A Useful Tool
*Corresponding Author(s):
Pozzi Mucelli Roberta AnteaDepartment Of Radiology, Azienda Sanitaria Universitaria Integrata Di Trieste, Trieste, Italy
Tel:+39 0403994372,
Email:roberta.pozzimucelli@gmail.com
Abstract
Balloon Assisted Technique (BAT) consists in the use of a balloon catheter advanced in a parallel fashion to main catheter in the same artery to overcome problems during endovascular interventions. We describe three different cases of BAT. The first case is an example of pancreatic-duodenal artery aneurysm treated with a flow-diverter stent; in the second case BAT was used to help the advancement of a covered stent in the renal artery during a “Chimney” deployment in an advanced EVAR procedure. The third case BAT allowed improving visibility and catheterization of a diaphragmatic artery feeding a small HCC during TACE procedure.
These are some possible applications of BAT technique. More than a technique we believe that BAT is a “maneuver” to be tailored for every complex situation with specific materials.
Keywords
INTRODUCTION
CASES DESCRIPTION
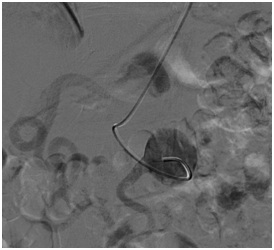
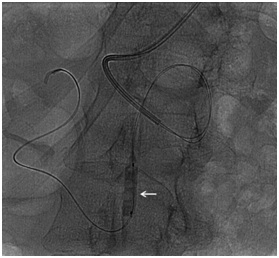
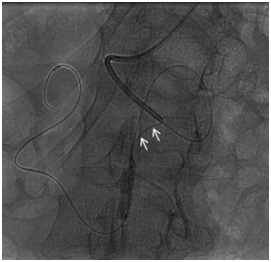

 Figure 1e: A 65 yrs woman with aneurysm of pancreatic-duodenal artery; CT follow-up after 3 months showed correct position of the flow diverter and exclusion of the aneurysmal sac.
Figure 1e: A 65 yrs woman with aneurysm of pancreatic-duodenal artery; CT follow-up after 3 months showed correct position of the flow diverter and exclusion of the aneurysmal sac.Abdominal aortic aneurysm treated with parallel stent grafting technique. Male, 75 yrs an asymptomatic juxtarenal abdominal aortic aneurysm of 5 cm of maximum diameter, was detected during abdominal US performed for unrelated pathology. CT-angiography confirmed the lesion starting just below the origin of SMA and involving both renal arteries. Patient preferred to be treated immediately instead of undergoing an imaging surveillance. An advanced EVAR treatment was planned with “parallel” stenting of both renal arteries and SMA because at that time this was our first choice of treatment for these type aneurysms. After surgical cut-down of the axillary artery two long introducer-sheaths were advanced, one in SMA and one in left renal artery. Right renal artery was approached from one of two femoral accesses; however advancement of stiff guidewire (Amplatz Super stiff-Boston) was problematic due to unfavorable angle. For this reason we decided to inflate an occlusion balloon (Reliant Medtronic) just over the origin of renal arteries while advancing the stiff wire in the right renal artery (Figure 2a) and after this, with the same modality, a 7F long introducer sheath (Destination Terumo) was introduced inside the artery (Figure 2b). After correct positioning of all sheaths the balloon covered stents were advanced and deployed at the origin of target vessels and EVAR treatment was completed as usual (Figure 2b).
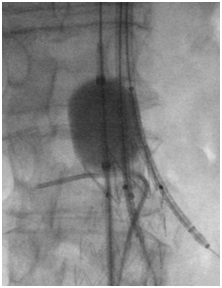
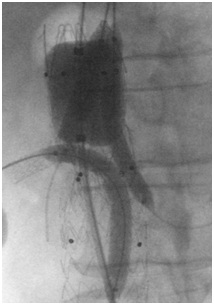 Figure 2b: A 75 yrs man with asymptomatic iuxtarenal abdominal aortic. An advanced EVAR treatment was planned with “parallel” stenting of both renal arteries and SMA; after a 7F long introducer sheath was introduced inside the artery and all balloon covered stents were advanced and deployed at the origin of target vessels.
Figure 2b: A 75 yrs man with asymptomatic iuxtarenal abdominal aortic. An advanced EVAR treatment was planned with “parallel” stenting of both renal arteries and SMA; after a 7F long introducer sheath was introduced inside the artery and all balloon covered stents were advanced and deployed at the origin of target vessels.Transarterial Chemoembolization (TACE) for Hepatocellular Carcinoma (HCC) with atypical feeding artery. Male, 68 yrs History of HCC treated with multiple chemoembolization procedures. At CT follow-up an incomplete response was detected in a nodule of the 7th segment and a feeding artery supplied by right diaphragmatic artery was suspected. Selective angiography of celiac trunk was done but visualization of right diaphragmatic artery was faint. To increase visibility of this artery a second femoral access was done and a balloon catheter inflated in the proximal celiac trunk improving detection of right diaphragmatic artery which was then easily catheterized. Selective injection confirmed feeding artery to the 7th segment HCC nodule and TACE procedure could be done.
DISCUSSION
CONCLUSION
CONFLICT OF INTEREST
REFERENCES
- Moret J, Cognard C, Weill A, Castaings L, Rey A (1997) [Reconstruction technic in the treatment of wide-neck intracranial aneurysms. Long-term angiographic and clinical results. Apropos of 56 cases]. J Neuroradiol 24: 30-44.
- Cohen JE, Gomori JM, Itshayek E (2011) Balloon-assisted looping technique to perform carotid artery stenting. J Clin Neurosci 18: 1538-1540.
- Prieto LR, Bellotti CA (2013) Balloon-assisted techniques for advancing long sheaths through difficult anatomy. Pediatr Cardiol 34: 1125-1129.
- Chen MC, Chang SC, Weng MJ, Tzeng WS, Wu RH, et al. (2006) Use of angioplasty balloon-assisted Seldinger technique for complicated small vessel catheterization. J Vasc Interv Radiol 17: 2011-2013.
- Lynch FC (2009) Balloon-assisted removal of tilted inferior vena cava filters with embedded tips. J Vasc Interv Radiol 20: 1210-1214.
Citation: Pozzi Mucelli F, Pozzi Mucelli RA, Sacconi F, Braini M, Belgrano MG, Cova MA (2019) Balloon Assisted Technique in Peripheral Interventions: A Useful Tool. J Angiol Vasc Surg 4: 022.
Copyright: © 2019 Pozzi Mucelli Fabio, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

