
Bart’s Syndrome: a case report
*Corresponding Author(s):
Mohamed SelloutiFaculty Of Medicine And Pharmacy, Neonatal Medicine And Intensive Care Unit, Mohammed V Military Teaching Hospital, Rabat, Morocco
Tel:+212-002-126-606-274-66,
Email:msellouti@gmail.com
Abstract
Bart's syndrome is a genodermatosis characterized by the absence congenital localized absence of skin, congenital epidermolysis bullosa, dystrophic nails, and the lesions of the mouth mucosa. It may be associated with any type of EB but is mostly reported with dominant dystrophic form. The clinical diagnosis is generally easy but the therapeutic management is difficult and the prognosis reserved.
We present a case of a newborn multiple ulcerations occupying almost all of the two lower limbs with some flaccid bubbles. Clinical appearence was sufficiently distinct to suggest the diagnosis of Bart’s syndrome.
Keywords
Bart’s Syndrome ; Epidermolysis bullosa; Skin aplasia.
Introduction
Bart syndrome is a rare neonatal pathology described in a large family in 1966 and consisted of any one or a combination of the he following three characteristics: congenital absence of skin, blistering and associated nail abnormalities [1].
Bart's syndrome is an autosomal dominant inheritance caused by mutations in the type VII collagen gene on chromosome 3p3. It was first described in a large family almost half a century ago [2]. Clinical diagnosis is easy but its management is delicate and the extended forms represent a real therapeutic challenge
The purpose of reporting this case is it being rare and how our timely conservative management of skin condition along with nutrition led to the favorable outcome of this non curable congenital disorder
Case Presentation
A 1-h-old female newborn presented with complete absence of skin over the anteromedial aspect of both lower legs and skin erosions all over the body since birth. The baby was delivered at term to a 38 year old mother via normal vaginal. She was the first child of a non-consanguinous couple and there was no family history of similar skin lesions. The pregnancy and delivery were uncomplicated. Mother had no history of drug intake or radiation exposure during her pregnancy. The baby's Apgar scores were normal, but he was admitted to the neonatal intensive care unit due to this skin lesion. Physical examination found a term newborn, with a weight of 2600 g (in the average), a height of 50cm (in the average), a head circumference of 34 cm (in the average). The hemodynamic state was stable, a skin recoloration time of less than three seconds, a normal heart rate of 160 beats/min, and a respiratory rate of 40 cycles/min. Otherwise, the patient presented an extensive skin defects on feet with multiple areas of skin erosions over scalp, trunk, nape of neck, and cheek. Few blisters could be appreciated around elbow and knee joint area which were suggestive of epidermolysis bullosa (figure 1a). The vascular network was clearly visible at the level of substance loss. The rest of the skin coating was normal (figure 1b)
 Figure 1a & 1b : Hemorragic bulla Absence of skin with Epidermolysis bullosa (Bart’s syndrome)
Figure 1a & 1b : Hemorragic bulla Absence of skin with Epidermolysis bullosa (Bart’s syndrome)
On the third day of life, nail abnormalities were observed: absence of some toenails and presence of intact bullous lesions on the lips and oral mucosa, which burst at minor friction. After 7 days, the baby developed blisters over the preexisting lesions. Blistering also appeared over normal skin in response to minor trauma or friction (figure 2).
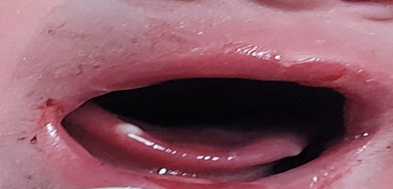 Figure 2 : Mucosal lesions
Figure 2 : Mucosal lesions
The diagnosis of Bart syndrome was retained based on features suggestive of epidermolysis bullosa and aplasia cutis. The proposed treatment was conservative, using gauze soaked in oil with essential fatty acids; the dressings were changed daily by a nurse with experience in dressing wounds. The mother was taught how to do the procedure and currently does so at home, but less frequently due to the almost complete healing (figure 3).
 Figure 3 : Healing of skin lesions
Figure 3 : Healing of skin lesions
The child is currently 3 months old, the lower limb injuries are fully healed. Care is being taken by the parents to avoid trauma and friction, and the child attends monthly follow-up consultations with a pediatric dermatologist.
Discussion
Bart syndrome was first described in 1966 by Bart and it is defined as the localized absence of the skin at birth [3]. It presents with the classic triad of congenital localized absence of skin over both lower legs, blistering of the skin, and nail dystrophy. It is most often sporadic, but familial cases have been reported [4]. The inheritance pattern of Bart syndrome appears to be autosomal dominant but sporadic cases have been reported [5]. This baby may be belongs to sporadic category due to absence of family history.
Bart syndrome has other associations such as pyloric atresia, microtia, flat nasal bridge, broad nasal root and widest eyes [6,7]. Clinically our patient had no other malformations.
Bart syndrome is increasingly considered an intrauterine variant of dystrophic epidermolysis bullosa [4, 8,9]. This is due to the fact that the mutation of the p21 region of the short arm of chromosome 3, involved in Bart’s syndrome, is contiguous to the type VII collagen gene (COL7A1) which encodes for type 7 collagen fibers, the main constituent of anchoring fibrils allowing cohesion between the dermis and the basement membrane [10,11]. The mutation of the COL7A1 gene, which results in a substitution of glycine into arginine, is the main mutation of dystrophic epidermolysis bullosa [12]. That being said, since Bart syndrome can be found in any type of congenital epidermolysis bullosa [13-15] as in the case of our patient where Bart syndrome was associated with junctional epidermolysis bullosa, several authors consider that Bart syndrome is only the result of a simultaneous intrauterine presence of a localized absence of the skin and congenital epidermolysis bullosa.
Treatment for Bart syndrome is typically lifelong and can be challenging for patients and their caregivers .It is mainly based on supportive care to promote the epithelialization and healing of skin lesions conservatively without complications which are reported to be infections (secondary sepsis, localized superinfection), hemorrhage due to skin fragility, dehydration and hydro electrolytic disorders [2].
Local application of diluted povidone iodine, application of non-adhesive bandages impregnated with dexpanthenol and chlorhexidine are recommended forms of wound care and it is not recommended to give systemic antibiotics prophylactically. A bath is recommended every day or every other day, using diluted antiseptics, also used to remove dressings in the bath if they stick too much. Bubbles should be pierced, and handling should be as gentle as possible to avoid further skin trauma. To prevent syndactyly, small bands between the fingers and toes are recommended [16].
Conclusion
Bart syndrome is a rare and complex disorder that presents with a wide range of symptom. Regardless, early diagnosis, appropriate treatment, and comprehensive care are essential for patients with Bart syndrome to achieve optimal outcomes.
Consent
Written informed consent was obtained from the patient for publication of this case report.
Disclosure
This clinical case was written based on clinical observation without any funding
References
- Bart BJ, Gorlin RJ, Anderson VE, Lynch FW (1996) Congenital Localized Absence of Skin and Associated Abnormalities Resembling Epidermolysis Bullosa. A New Syndrome. Archives of Dermatology 93: 296-304.
- Cissouma A, Kassogue D, Sylla M, Demebele G, Traore SA, et al. (2021) Bart’s Syndrome: A Neonatal Observation About a Case Report. Open Journal of Pediatrics 11: 406-412.
- Grosshans E (1999) Malformations congénitales de la peau. EMC Dermatologie 59 : 10.
- Aparecida Pereira de Almeida, N, Serafini F, Marchiori, J (2010) Do You Know This Syndrome? Anais Brasileiros de Dermatologia, 85 : 951-953.
- Alfayez Y, Alsharif S, Santli A (2017) A Case of Aplasia Cutis Congenita Type VI: Bart Syndrome. Case Rep Dermatol 9: 112-118.
- Cicekci F (2022) Anesthesia Management in Bart’s Syndrome: A Case Report. Acta Medica Alanya 6: 114-117.
- Rajpal A, Mishra R, Hajirnis K, Shah M, Nagpur N (2008) Bart’s Syndrome. Indian J Dermatol 53: 88-90.
- Aygun AD, Yilmaz E, Kurt AN, Kurt A, Elkiran O, et al. (2010) Aplasia cutis congenita and epidemolysis bullosa: Bart syndrome. International Journal of Dermatology 49: 343-345.
- Gutzmer R, Herbst RA, Becker J, Kiehl P, Bisping-Kuske C, et al. (1997) Bart Syndrome-Separate Entity or a Variant of Epidermolysis Bullosa? Hautarzt, 48: 640-644.
- Zelickson B, Matsumura K, Kist D, Epstein EH Jr, Bart BJ (1995) Bart’s Syndrome. Ultrastructure and Genetic Linkage. Archives of Dermatology 131 : 663-668.
- Christiano AM, Bart BJ, Epstein EH Jr, Uitto J (1996) Genetic Basis of Bart’s Syndrome: A Glycine Substitution Mutation in Type VII Collagen Gene. Journal of Investigative Dermatology 106: 778-780.
- Ingen-Housz-Oro S, Blanchet-Bardon C (2004) Épidermolyses bulleuses héréditaires. EMC Dermatologie 11: 98-255-A-1.
- Morrell DS, Rubenstein DS, Briggaman RA, Fine JD, Pulkkinen L, et al. (2000) Congenital Pyloric Atresia in a Newborn with Extensive Aplasia Cutis Congenita and Epidermolysis Bullosa Simplex. British Journal of Dermatology 143 : 1342-1343.
- Maman E, Maor E, Kachko L, Carmi R (1998) Epidermolysis Bullosa, Pyloric Atresia, Aplasia Cutis Congenita: Histopathological Delineation of an Autosomal Recessive Disease. American Journal of Medical Genetics 78: 127-133.
- Jones EM, Hersh JH, Yusk JW (1992) Aplasia Cutis Congenita, Cleft Palate, Epidermolysis Bullosa, and Ectrodactyly: A New Syndrome? Pediatric Dermatology 9: 293-297.
- Kuvat SV, Bozkurt M (2010) Conservative treatment of a patient with epidermolysis bullosa presenting as Bart syndrome: a case report. Case Reports in Medicine
Citation: Sellouti M, Ayad A, Abilkassem R, Agadr A (2023) Bart’s Syndrome: a case report. J Neonatol Clin Pediatr 10: 113.
Copyright: © 2023 Mohamed Sellouti, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

