
Bilateral Genicular Nerve Radio Frequency Ablation (RFA) for the Treatment of Refractory Pain in a Patient with Pigmented Villonodular Synovitis (PVNS)
*Corresponding Author(s):
Mohammed SiddiquiLoyola University Medical Center, Maywood, Illinois, United States
Tel:+1 8478457356,
Email:Modman04@gmail.com
Abstract
Background: Patients suffering from Pigmented Villonodular Synovitis (PVNS) that have failed treatment with total knee replacement surgery do not have many targeted options in treating their chronic knee pain. We have been using Radio Frequency Ablation (RFA) to treat patients with chronic knee pain from knee osteoarthritis, but there have been no cases in the literature describing the use of genicular nerve RFA in the treatment of patients with PVNS who have knee pain and have failed knee surgery.
Hypothesis: RFA may be an effective way to reduce knee pain and improve function in patients that suffer from PVNS that have failed total knee reconstruction.
Study design: Retrospective case report on a single patient with PVNS who continued to have ongoing bilateral knee pain despite undergoing bilateral total knee replacements.
Methods: This was a case report of a single patient who had PVNS and failed bilateral knee replacements who underwent RFA with documented improvement in her percentage improvement in Pain scores and Oswestry Disability Index scores both pre and post Radiofrequency ablation.
Results: Patient’s Oswestry Disability Index score pre-ablation was 39% (considered moderate-severe disability) and at 6 month follow up her post-ablation score decreased to 24% (considered mild-moderate disability). The patient demonstrated a reduction in her pain score of 75% relief for 4 months on her left knee and a reduction of 62.5% relief of her pain on the right knee.
Conclusion: RFA may be a valuable tool to improve pain and disability in patients suffering from PVNS who have failed total knee replacement.
INTRODUCTION
Pigmented Villonodular Synovitis (PVNS) is a benign proliferative disease of the synovium. PVNS is predominantly monoarticular and frequently targets the knee joint. Even though this is a benign condition, it can be very aggressive with a high rate of local recurrence (8%-56%) [1,2]. PVNS has an incidence of about 1.8 per million [3].Those primarily affected are in their third to fourth generation of life with both genders affected approximately equally [4]. PVNS can result in severe joint degeneration with damage to surrounding bone and cartilage. If left untreated, PVNS can lead to severe chronic pain in the affected joint along with functional disability for the patient. There are currently two different forms of the disease; the localized form and diffuse form [5].
Surgery, either open or arthroscopic, for resection of synovial tissue has been primarily the treatment of choice [6-8]. In addition to surgery with possible synovectomies, radiation therapy has been used to prevent local recurrences of masses [9]. RFA has had a limited role in the treatment of PVNS thus far and the only documented use is for tumor ablation for areas of the knee not amenable to surgery. Currently, there is no data on radiofrequency therapy of the genicular nerves as a viable treatment option for chronic knee pain in patients with PVNS history and this case study aims to quantify the effectiveness of this approach.
PATIENT HISTORY
In 2005 the patient underwent a right knee arthroscopy with excision of knee mass, chondroplasty of patella of the lateral facet, and synovectomy major with medial plica excision. Pathology revealed giant cell tumor of tendon sheath, diffuse type PVNS of the medial patellar retinaculum. Between 2005-2009, patient had an unknown amount of steroid injections on the right knee for pain control.
In 2009 an MRI of her right knee showed no evidence of local recurrence of the patient’s giant cell tumor, diffuse PVNS. A right knee arthroscopy was performed with extensive debridement of the anterior fat pad, as well as chondroplasty for loose cartilage. The pathology reports showed cartilage with degenerative changes and synovium with mild chronic inflammation. The patient had continued difficulties with that knee, but also developed left knee pain with subsequent MRI of the left knee showing no evidence of a meniscal, cruciate ligament or collateral ligament tear. A left knee arthroscopy was performed on 2010 with debridement of loose bodies as well as a chondroplasty to the medial femoral condyle defect and excision of medial plica. Despite the treatment, the patient continued to have bilateral knee pain afterwards with nonsurgical measures attempted for about 2 years. She underwent bilateral total knee arthroplasty in 2012. The patient reported continued knee pain following the bilateral arthroplasty. CT was performed to evaluate rotational analysis of bilateral knee implants which was read as normal. Indolent infection and other possible causes of pain including spine etiology were ruled out. Ultimately a left total knee arthroscopy with revision of femoral and tibial component was performed. The surgery did not provide her long term pain relief and symptoms in both knees returned. It was decided not to pursue further surgical options. She was then referred to our pain clinic for interventional treatment options.
After evaluation it was decided to proceed with a genicular nerve block of the left knee. The diagnostic block of the genicular nerves provided greater than 80% relief of the patient’s knee pain. Based on her positive response it was decided to pursue radiofrequency ablation of the left knee, which was done on the subsequent visit.
Similarly, on a later date, a diagnostic right genicular nerve block was performed with greater than 80% relief of her pain. This was then followed by radiofrequency ablation of the right knee.
On her follow-up visits, documented pain scores (rated from 0-10; 0 being an indication for no pain and 10 reflecting the worst pain a patient could imagine) and an Oswestry Disability Index (ODI) questionnaire (a self-reported questionnaire that evaluates how the patient’s pain limits activities of daily living such as walking, sitting, personal care, etc.) were performed for this patient following her radio frequency ablation procedures. Patient’s ODI score pre-ablation was 39% (considered moderate-severe disability). At the 6 month follow up, her post-ablation ODI score decreased to 24% (considered mild-moderate disability).
Patient reported improvement in her pain scores of 75% relief for 4 months at her 6 month follow up for her left knee post ablation. Her two month follow up for the right knee post ablation coincided with her 6 months follow up for her left knee post ablation. At that time she also reported 62.5% improvement of her right knee pain symptoms. Please refer to table 1 for a detailed timeline of patient history.
|
Date |
Type |
Findings |
|
11/3/2005 |
MRI |
Right knee: small knee joint effusion, no evidence for meniscal tear or abnormality of the cruciates |
|
12/21/2005 |
Procedure |
Right knee: arthroscopy with excision of knee mass, chondroplasty of patella of the lateral facet, synovectomy major with medial plica excision Pathology: diffuse type PVNS |
|
8/5/2006 |
MRI |
Right knee: the focal abnormality that was seen on medial aspect of the right knee on previous MRI has been surgically resected and is no longer visualized. Bones unremarkable. Small knee effusion/mild abnormal signal in the distribution of the synovium, mild abnormal enhancement along the lateral aspect of the right knee joint. |
|
11/16/2006 |
MRI |
Left knee: trace suprapatellar bursa effusion, focal abnormal signal in the superior aspect of the patella, focal contusion vs focal edema. |
|
2005-2009 |
Procedure |
Unknown amount of R knee cortisone injections |
|
5/12/2009 |
MRI |
Right knee: no evidence of local recurrence of the patient's giant cell tumor of the medial patellar retinaculum, mild focal thickening of the medial patellar retinaculum is presumably postsurgical in etiology |
|
6/16/2009 |
Office visit |
Office visit with Orthopedic Oncology for evaluation for PVNS recurrence; given last MRI, did not think knee pain due to PVNS recurrence, recommended trial of anti-inflammatories, PT and arthroscopy with synovial biopsies, possible synovectomy based on findings |
|
10/28/2009 |
Procedure |
Right knee: arthroscopy with extensive debridement of the anterior fat pad, as well as chondroplasty for loose cartilage on the medial femoral condyle that was not full thickness Pathology: cartilage with degenerative changes, synovium with mild chronic inflammation |
|
1/26/2010 |
MRI |
Left knee: no evidence of a meniscal, cruciate ligament or collateral ligament tear, knee joint effusion |
|
3/9/2010 |
Procedure |
Left knee: arthroscopy with debridement of loose bodies as well as a chondroplasty to the medial femoral condyle defect with microfracture as well as excision of medial plica Pathology: no report |
|
7/9/2012 |
Procedure |
Bilateral total knee arthroplasty Pathology: No report |
|
7/14/2016 |
Office visit |
Office visit with Orthopedic Oncology for evaluation of recurrent b/l knee pain. Recommended a CT scan to evaluate rotational analysis of b/l knee implants, check alignment, and obtain ESR/CRP to rule out indolent infection (both levels wnl) |
|
8/9/2016 |
Office visit |
Office visit with ortho joints for evaluation of recurrent b/l knee pain. Recommended MRI of lumbar spine given recent onset of left leg numbness and rule out lumbar spine pathology |
|
8/19/2016 |
MRI |
Findings: minimal degenerative changes without evidence for significant spinal canal or neural foraminal narrowing at any level |
|
10/26/2016 |
Procedure |
Left knee: revision total knee arthroplasty, femoral and tibial components Pathology: no histologic sections taken |
|
10/9/2017 |
Office visit |
Office visit with Pain Management Recommendation for genicular nerve block |
|
11/17/2017 |
Office visit |
Office visit with Pain Management. Not approved for genicular nerve block, recommended acupuncture |
|
4/16/2018 |
Office visit |
Office visit with Pain Management. Patient has tried acupuncture with no relief. Planning on left knee genicular nerve block |
|
5/15/2018 |
Procedure |
Left knee genicular nerve block. 80% resolution of pain |
|
7/13/18 |
Procedure |
Left knee genicular nerve RFA |
|
9/10/2018 |
Office visit |
Office visit with Office visit with Pain Management |
|
10/9/2018 |
Procedure |
Right knee genicular nerve block with 80% resolution of pain |
|
11/9/2018 |
Procedure |
Right knee genicular nerve RFA |
|
1/14/2019 |
Office visit |
Office visit Office visit with Pain Management |
Table 1: Patient time course.
METHODS
Anatomy of the knee, innervation of genicular nerve
Hilton’s law states that nerves that supply a joint are the same nerves that supply adjacent and extending muscles acting on that given joint [10-12]. Thus, sensory nerves of the quadriceps and hamstring muscles largely innervate the knee joint. The knee joint is primarily innervated by articular branches of the tibial, obturator, saphenous, femoral, and common peroneal nerves [13]. The anterior portion of the knee is primarily divided into four quadrants to better understand its sensory innervations. These four quadrants are the superolateral, superomedial, inferolateral, and inferomedial.
The tibial nerve is responsible for articular branches that innervate the superomedial and inferomedial genicular nerves [14]. The superomedial quadrant is furthermore innervated by nerve branches of the femoral and obturator nerves [15]. The inferomedial sensation of the knee joint is also innervated by the infrapatellar branch of the saphenous nerve [16]. The inferolateral sensation of the knee joint is innervated by the peroneal division of the sciatic nerve. The superolateral sensation of the knee joint is innervated by the common peroneal division of the sciatic nerve that originates about 8-10 cm superior to the knee joint [14]. The targeted nerves for lesion in genicular radiofrequency ablation are those that supply only sensory innervation to the superomedial, superolateral and inferomedial quadrants. The inferior lateral genicular branch should not be lesioned due to the concern for motor nerve lesioning of the common fibular nerve innervation and the possibility of foot drop.
PROCEDURES
Diagnostic nerve blocks
Prior to the ablative procedure, patients who are candidates for interventional pain procedures using radiofrequency ablation undergo diagnostic nerve blocks. These blocks, as explained to patients, are for diagnostic purposes. The superolateral, superomedial and inferomedial genicular nerves are targeted using fluoroscopic guidance. The three targets for the block (which will mimic the same target areas for the ablation) are the junction of the shaft of the femur and bilateral epicondyles for the superior genicular nerves and the shaft of the medial tibia and epicondyle for inferomedial block. The needles are advanced to the 50th percentile of the femoral or tibia shaft where the genicular nerves run. The block consists of 1 ml of equal parts 1% lidocaine and 0.25% bupivacaine at each of the above listed sites. If the patient obtains substantial relief immediately following the block with greater than 80% relief of pain, than the patient is considered a good candidate for radiofrequency ablation.
Cooled radiofrequency ablation
After successful diagnostic nerve block, the patient was a candidate for radiofrequency ablation. Cooled RFA is used in this procedure given that it produces a larger lesion size than traditional RFA. Traditional RFA produces its therapeutic effect by generating an electric field through the inserted electrode and a grounding pad. The electric field causes a vibration of ions resulting in ion movement and thereby the generation of heat due to friction, which in turn can then lesion the nerve. In cooled RFA the lesioning is done in a comparable way, but to increase the ablation zone the electrode is cooled by perfusing an internal water source through the electrode. Without electrode cooling, the tissue region of the highest temperature is located next to the electrode, since that is the location of the highest electrical current density. However, by actively cooling the electrode the tissue in close proximity of the electrode is also cooled, thereby resulting in location of highest tissue temperature being moved further into the tissue producing a larger ablation zone [17]. The lesion created by traditional RFA produced an elliptical pattern, versus cooled RFA that produced a more spherical lesion pattern. Comparing the lesion sizes in volumes of traditional to cooled RFA, it was found that cooled RFA produced lesions that were 2.8-3.4 times larger lesion volumes than the traditional 18g or 20g RFA needle with 10mm active tips respectively [18].
Patient was given antibiotics 30 minutes prior to the procedure due to proximity of needle placement to a joint with instrumentation. Patient was placed in the supine position with the knee slightly bent with a rolled towel under the knee. The knee was also placed in slight internal rotation and leg was taped and stabilized. After sterile prep, drape and localization of the area using fluoroscopy, local infiltration was performed and three 50 mm Cooled RFA needles were advanced along the superior lateral geniculate nerve where the lateral femoral shaft meets the epicondyle, the superior medial geniculate nerve where the medial femoral shaft meets the epicondyle, and the inferior medial geniculate nerve where the medial tibial shaft meets the epicondyle at the depth of ~ 50% of the femur and tibia. AP and lateral imaging showed appropriate placement at each level along half the distance of the shaft of the femur and tibia. Local anesthetic given with 1% lidocaine and cooled RFA performed at each level for approximately 150 seconds at a 60°C.
RESULTS
The Oswestry Disability Index questionnaire was completed by the patient pre-ablation and post ablation. The questionnaire measures functional disability with topics pertaining to pain in relation to pain intensity, personal care, ability to lift heavy objects, quantity of walking, ability to stand, sleep, one’s social life, and ability to travel. Each section is scored from 0-5 and tallied up for a final score. A score of 0 indicates no pain, and a score of 5 indicates severe disabling pain [7]. A sample ODI questionnaire is presented in figure 1 [19]. The total score is multiplied by 100 for a percentage. A final percentage 0-20% is deemed minimal disability, 21-40% moderate disability, 41-60% severe disability, 61-80% crippling pain in all aspects of life, and 81-100% is pain that requires bed bound patient or severe exaggeration [19]. The patient’s Oswestry Disability Index score pre-ablation was 39%. Her score decreased post-ablation score to 24%.
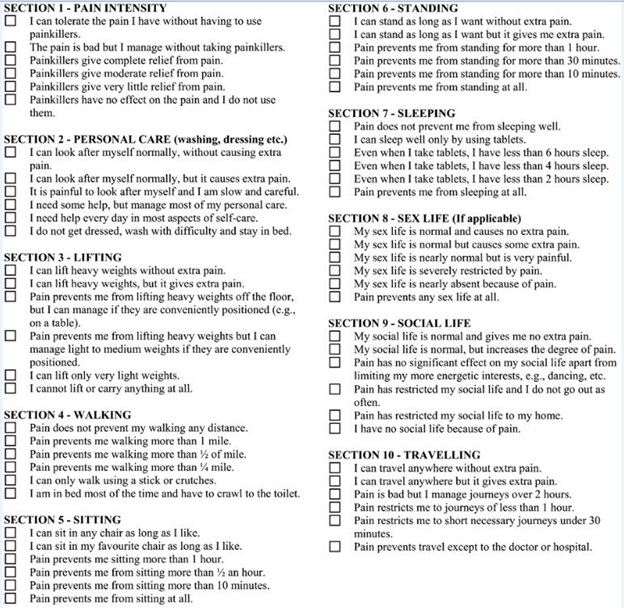 Figure 1: Sample ODI questionnaires.
Figure 1: Sample ODI questionnaires.
The patient’s knee pain was documented both pre and post-ablation on a scale of 0-10. Pre-ablation for the left knee, the patient had a score of 7 out of 10 documented. Post left genicular nerve ablation; patient reported 70% decrease in pain during her 3 month follow up. On her 6 month follow up, she reported 75% relief that lasted for 4 months before the pain started to worsen to a level of 6 out of 10 at the 6 month follow-up. Patient’s pre-ablation score on the right knee was 8 out of 10. On 2 month follow up for the right genicular nerve ablation, patient reported pain of 3 out of 10 or a 62.5% decrease in her pain symptoms.
DISCUSSION/CONCLUSION
Radio Frequency Ablation (RFA) has been frequently used in a number of clinical scenarios since the 1980’s. RFA works by heating via an electric current using an electrode to lesion the targeted area. RFA began as a viable treatment option for certain cardiac arrhythmia in the 1980’s and expanded to treatments for cancers and interventional pain procedures [17].
Lalam et al., demonstrated the use of RFA as a possible treatment modality in patients with PVNS by lesioning tumors in areas not amenable to surgery [18]. Other studies have shown efficacy of RFA in providing pain reduction in chronic knee pain secondary to knee osteoarthritis. Choi W et al., performed a randomized trial that measured pain reduction at 1,4 and 12 week follow-ups using radiofrequency treatment for osteoarthritis of the knee. The results showed a reduction of knee pain by at least 50% during each follow up [20]. None of the studies above looked at disability scores as measures for functional improvement.
Possible complications of RFA have been skin burns, especially during use of tumor ablations when the power needs to be in the higher range and for a longer duration of time. Of note, there have not been many documented complications using the RFA technique for pain management of the genicular nerves.
To our knowledge, no report has been published on the effectiveness of genicular nerve RFA for chronic knee pain in patients with PVNS using the Pain and Oswestry Disability Index scores to demonstrate improvement in pain and function. In this case report, we reviewed the pain and functional disability improvement of a patient with chronic bilateral knee pain secondary to PVNS diffuse type status post bilateral total knee arthroplasty who underwent bilateral knee radiofrequency ablation.
After receiving cooled RFA ablation on her left and right knees, her Oswestry disability score had a 15% reduction over a period of 6 months for her left knee and 2 months for her right knee. Her initial score pre-ablation (39%) put her borderline between moderate to severe disability category. Post-ablation, her score (24%) had dropped significantly putting her in the mild to moderate disability category. This reflects a vast improvement in her functional ability on a daily basis and her overall quality of life over an extended period of time of up to 6 months. Thus, these improvements as it pertains to functional disability demonstrated a significant improvement for a prolonged period of time.
Her pain score pre-ablation was 7 out of 10. On sixth month follow-up after the left knee RFA; she reported a 75% decrease in pain that lasted 4 months with gradual return of pain to a level of 6 out of 10 by 6 months. Patient’s pre-ablation score on the right knee was 8 out of 10 and on 2 month follow up post RFA, patient reported a 62.5% decrease in her right knee pain. Her vast improvement in pain shows promise that RFA can possibly be an option for those patients suffering from chronic knee pain secondary to PVNS. Furthermore, the longevity of her pain reduction is another consideration to be investigated in the future. Her pain relief lasting about 6 months on the left knee is quite remarkable as she had reported severe chronic pain not adequately controlled by any other treatment therapies in the past.
Some limitations to this case report include that it is a retrospective study with memory bias, selection bias, and limited reproducibility as only one patient was evaluated. However, it is worth noting that the patient did obtain excellent results in both knees that were treated with genicular nerve RFA at different times.
Future studies should investigate using genicular nerve RFA earlier in the disease progression of PVNS to possibly avoid more invasive procedures for pain control. Furthermore, future studies should utilize genicular nerve RFA for destructive joint diseases not amenable to other treatment options for possible symptom relief. Outcomes from future studies should also include evaluation of improvement in disability along with pain scores. As this is a retrospective study with limitations stated above, a prospective study with a larger sample size looking at RFA as a treatment modality for this condition would be very beneficial. Finally, this case report furthers the literature on potential treatment of chronic knee pain from a variety of different disease processes using genicular nerve RFA.
REFERENCES
- Ogilvie-Harris DJ, McLean J, Zarnett ME (1992) Pigmented villonodular synovitis of the knee. The results of total arthroscopic synovectomy, partial, arthroscopic synovectomy, and arthroscopic local excision. J Bone Joint Surg Am 74: 119-123.
- Zvijac JE, Lau AC, Hechtman KS, Uribe JW, Tjin-A-Tsoi EW (1999) Arthroscopic treatment of pigmented villonodular synovitis of the knee. Arthroscopy 15: 613-617.
- Myers BW, Masi AT (1980) Pigmented villonodular synovitis and tenosynovitis: a clinical epidemiologic study of 166 cases and literature review. Medicine (Baltimore) 59: 223-238.
- Duan Y, Qian J, Chen K, Zhang Z (2018) Necessity of adjuvant postoperative radiotherapy for diffuse pigmented villonodular synovitis of the knee: A case report and literature review. Medicine (Baltimore) 97: 9637.
- Granowitz SP, Mankin HJ (1967) Localized pigmented villonodular synovitis of the knee. Report of five cases. J Bone Joint Surg Am 49: 122-128.
- Casp AJ, Browne JA, Durig NE, Werner BC (2019) Complications After Total Knee Arthroplasty in Patients With Pigmented Villonodular Synovitis. J Arthroplasty 34: 36-39.
- Nassar WA, Bassiony AA, Elghazal HA (2009) Treatment of diffuse pigmented villonodular synovitis of the knee with combined surgical and radiosynovectomy. HSS J 5: 19-23.
- Aurégan JC, Klouche S, Bohu Y, Lefèvre N, Herman S, et al. (2014) Treatment of pigmented villonodular synovitis of the knee. Arthroscopy 30: 1327-1341.
- Temponi EF, Barros AAG, Paganini VO, Barbosa VAK, Badet R, et al. (2017) Diffuse pigmented villonodular synovitis in knee joint: diagnosis and treatment. Rev Bras Ortop 52: 450-457.
- Hilton J (1863) On the influence of mechanical and physiological rest in the treatment of accidents and surgical diseases, and the diagnostic value of pain: a course of lectures, delivered at the Royal College of Surgeons of England, in the years 1860, 1861, and 1862. London: Bell and Daldy, Pg No: 1-499.
- Garg K, Mrudula C, Pragati S (2016) BD Chaurasia’s Human Anatomy. New Delhi: CBS Publishers & Distributers 56.
- Moore KL, Daly AF, Agur AMR (2010) Clinically Oriented Anatomy, 6th edn. J Anat 215: 474.
- Hirasawa Y, Okajima S, Ohta M, Tokioka T (2000) Nerve distribution to the human knee joint: anatomical and immunohistochemical study. Int Orthop 24: 1-4.
- Callaghan JJ, Rosenberg AG, Rubash HE (2003) Surgical Anatomy of the Knee. Philadelphia: Lippincott Williams & Wilkins 2003: 77-78.
- Dellon AL (2009) Partial joint denervation II: knee and ankle. Plast Reconstr Surg 123: 208-217.
- Gardner E (1948) The innervation of the knee joint. The Anatomical Record 101: 109-130.
- Haemmerich D (2010) Biophysics of Radiofrequency Ablation. Crit Rev Biomed Eng 38: 53-63.
- Lalam RK, Cribb GL, Cassar-Pullicino VN, Cool WP, Singh J, et al. (2015) Radiofrequency thermo-ablation of PVNS in the knee: initial results. Skeletal Radiol 44: 1777-1784.
- Fairbank JC, Couper J, Davies JB, O'Brien JP (1980) The Oswestry low back pain disability questionnaire. Physiotherapy 66: 271-273.
- Choi WJ, Hwang SJ, Song JG, Leem JG, Kang YU, et al. (2010) Radiofrequency treatment relieves chronic knee osteoarthritis pain: a double-blind randomized controlled trial. Pain 152: 481-487.
Citation: Siddiqui M, Bajaj P, Hintz A (2020) Bilateral Genicular Nerve Radio Frequency Ablation (RFA) for the Treatment of Refractory Pain in a Patient with Pigmented Villonodular Synovitis (PVNS). J Phys Med Rehabil Disabil 6: 041.
Copyright: © 2020 Mohammed Siddiqui, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

