
Biochemical Endothelial Injury and Platelets Activation Detectionin Endovenous Laser Ablation of Varicose Veins
*Corresponding Author(s):
Ayman M FakhryDepartment Of Vascular Surgery, Egyptian Medical Military Academy, Egypt
Email:ayman_vasc@LIVE.COM
Abstract
Background: Thrombus formation and extension to femoral or popliteal veins and pulmonary embolism may be though as a complication of EVLT in varicose veins treatment we aimed to study the thermal energy effect of the procedure under standardized conditions on biochemical markers of platelets and endothelium activities. Patients and methods: 25 patients admitted to vascular surgery dept. of Alexandria armed forces hospital with varicose veins and GSV. reflux and all treated by endovenous laser ablation during: 1/1/2018_12/31/2018. Venous blood samples were taken from iliofemoral and antecubital veins, before during and one day after surgery of P-selectin, soluble thrombomodulin, fibrin degradation products and D-dime
Results: There was no immediate rise of P-selectin and s TM in neither iliofemoral nor antecubital veins, where FDPs D-dimer was significantly elevated post operatively in the two regions.
Conclusion: 1480 pulsed mode diode laser doesn’t induce measurable endothelial and platelets activation in iliofemoral region during endovenous ablation of varicose veins.
Keywords
Ablation; Biomarkers; Laser; Varicose veins
Background
Chronic venous insufficiency is a major problem that includes varicose veins as one of its entities and accounts for about quarter of the US population. Most of the patients need intervention to deal with the problem at a specific stage of the disease [1]. Endovenous ablation of varicose veins is the new era for managing the varicose veins with clinical success comparable to the conventional stripping operations that were adopted [2]. However: major complications of venous thrombo-embolism are relatively less in the endovenous procedures compared to the standard stripping operation [3]. The thermal reactions induce endothelial damage causing venous Thrombosis which may extend from the superficial into the deep venous system bears the risk of Pulmonary Embolism (PE) The risk of Deep Vein Thrombosis (DVT) after EVLA is considered to be low, but there are two reports that describe thrombus extension in 7.7% of GSV and 5.7 % of Small Saphenous Vein (SSV) ablation ;But they account for about two percent in the endovenous procedures in most literatures [4]. Some risk factors are considered to increase the incidence of venous thrombo-embolism as previous deep venous thrombosis, Small saphenous vein ablation, age, gender and hypercoagulable state [5]. Endothelial and platelet activation and surgical trauma are measurable aspects to measure the effect of endovenous Laser ablation of primary varicose veins in inducing thrombosis, so we can predict which patients have more postoperative thrombosis risk and start prophylaxis against it [6].
Aim of the Study
To investigate whether an immediate rise of biochemical markers can be observed when laser ablation of the GSV is performed under standardized treatment conditions, leaving the most proximal 2 cm untreated.
Patients And Methods
This prospectively designed nonrandomized study. Enrolled 25 patients with primary GSV incompetence scheduled for EVLA performed under regional anesthesia (tumescent anesthesia). Admitted to vascular surgery department of Alexandria armed forces hospitalfromJan.1st 2018-Dec.31st 2018. Ethical approval for the study was obtained from the Ethics Committee Medical. All patients were clinically examined and assessed according to (CEAP Classification) after signing the approved medical consent. Dulex examination to assess the great and small Saphenous vein diameter, its patency and competency with measuring the direction,velocity and duration of reflex. Also femoral and poplitial veins and perforators were checked in both supine and erect positions using (Logiq 7 General Electric).this duplex examination was done before ablation, just after ,48 hours later,7 days ,one month and one year in the follow up visits. Venous blood samples were taken from iliofemoral and anticubital veins, before during and one just after surgery of P-selectin and D-diamer. Endovenous laser ablation of the great saphenous vein using the Fox 1040-nm diode system. (Fox, Inc., A.R.C., MA) undertumescent anesthesia and mild sedation (Figure 1).
 Figure 1: The laser machine - Fox 1040-nm diode system. (Fox, Inc., A.R.C., MA).
Figure 1: The laser machine - Fox 1040-nm diode system. (Fox, Inc., A.R.C., MA).
And the ablation was done under standardized treatment conditions, leaving the most proximal 2 cm untreated Figure 2(A&B).
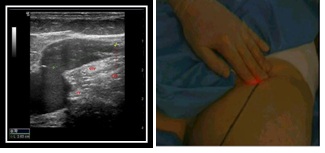 Figure 2(A&B): Laser fiber 2cm from sfj.
Figure 2(A&B): Laser fiber 2cm from sfj.
Biomarkers and Assay Methods Measurements
Commercially available enzyme-linked immune sorbent assay kits were employed to measure plasma antigen levels of (s) P-selectin (Quantikine STM, R&D Systems, Minneapolis, MN; normal range 18–20 ng/mL; intra- and inter assay Coefficients of Variation (CV) 6.8% and 8.9%, respectively.)and D-dimer (Asserachrom D-dimer, Roche-Diagnostics, Mannheim, Germany) normal range 400 ng/mL; intra- and inter assay CV 2.8% and 6.8%, respectively) were measured according to the manufacturers’ instructions. All analyses were done in duplicate, and all samples were thawed and analyzed at the same time. Statistics:
All data are presented as means 7 standard deviations (SDs).
Statistical significance also measured and Po.05 was considered statistically significant.
Results
This study was done for treating 25 patients with primary varicose and all of them was complaining of heaviness and pain of different degrees in one or both lower limbs together with dilated veins with C2-6 (CEAP) 12 patients48% were (class 3), one patent 4% (class 2), 4 patients16%(class 6) and 2 patients8% in class (4&5) (Table 1).
|
CEAP class |
Patients |
|
2 |
One patients |
|
3 |
16 patients |
|
4 |
2 patients |
|
5 |
2 patients |
|
6 |
4 patients |
Table 1: CEAP classification of patients.
The mean age of patients during presentation was 32.3+1.04 years and ranged from 16 to 56 years. We conducted more female patients in our series 16 ladies 64% and only 9 male patients 36%. 16 patients 64% were presented by dilated veins on left lower limb, 3patents 12% on right lower limb while 6 patients 24% was presented by bilateral lowerlimb varicosities. Great saphenous vein was affected in all patients 100% and in combination with small saphenous vein in 4 patients 16% (Figure 3).
 Figure 3: GSV marked after assessment.
Figure 3: GSV marked after assessment.
Preoperative duplex examination using linear 7.5mg Htz probe in both supine and erect positions revealed patent and comprisable great and small saphenous veins, femoral and popliteal veins with no evidence of thrombosis. Persistent venous reflex after Valsalva method or onabdomeno- pelvic compression that lasted more than 0.5 second over the Saphenofemoral Valve (SFV) in both supine and erect positions in all patients with mean duration 0.7+0.04 second while it was noticed over Sapheno Popliteal Valve (SPV) after calf compression in supine position in 4 patient 16% (Figure 4).
 Figure 4: Duplex examination of GSV in erect position.
Figure 4: Duplex examination of GSV in erect position.
Diameter of great saphenous vein was ranged from 6-9 mm with mean diameter 7.8+0.5 mm and that of incompetent small saphenous vein5.7 +0.4 mm and ranged from 4.9-7.1 mm.
Post-operative duplex examination done immediately showed occlusion of great and small saphenous vein with no evidence of thrombosis and patent comprisable femoral and popliteal veins. Two days later 3 patients 12% revealed superficial; thrombophlebitis of great saphenous vein and one of them developed deep vein thrombosis of the left femoral vein 4% one week later. Also duplex showed absent reflux in immediate, 2 days, one week and one-month examinations while recurrence of reflux was noticed in Sapheno femoral valve in 3 patients 12%
Measurements of biomedical thrombosis {d-dime and P selection} was done in all patients in three times; just before ablation, during and immediately post ablation of great saphenous vein taking blood samples from the antecubital (peripheral vein) and femoral vein. Tables 2&3 P-selectin values were elevated non scientifically in both peripheral and femoral veins only after laser ablation of the saphenous vein, while there was no significant difference in its level in samples taken from both veins in the three times of blood sampling. There was a significant rise of its level in post ablation samples (22&23.2ng/mL) in both peripheral and femoral veins samples in 3 patients 12 %; all of them showed superficial thrombophlebitis after 48 hours and one showed femoral vein thrombosis one week later.
|
|
P-selectin ng/mL |
|
|
|
Peripheral vein |
Femoral vein |
|
Before ablation |
15.9 ng/mL |
16 ng/mL |
|
During ablation |
16.2 ng/mL |
16.4 ng/mL |
|
After ablation |
18.4 ng/mL |
18.2 ng/mL |
Table 2: P-selectin in peripheral & femoral veins.
Also we noticed d dimer values were elevated non scientifically in both peripheral and femoral veins during and after laser ablation of the saphenous vein, while there was no significant difference in its level in samples taken from both veins in the three times of blood sampling. There was a significant rise of its level in during ablation samples (500 &519ng/mL) which persists in the post ablation sample (555&538 ng/mL) in both peripheral and femoral veins samples in 3 patients 12 %; all of them showed superficial thrombophlebitis after 48 hours and one showed femoral vein thrombosis one week later.
|
|
Peripheral vein |
Femoral vein |
|
Before ablation |
199 ng/mL |
201 ng/mL |
|
During ablation |
421ng/mL |
419 ng/mL |
|
After ablation |
409 ng/mL |
408ng/mL |
Table 3: D dimer in peripheral & femoral veins.
Discussion
The aim of the study was to investigate whether an immediate rise of biochemical markers can be observed when 1040 diode laser used for the ablation of the GSV is performed under standardized treatment conditions, leaving the most proximal 2 cm untreated with enough amount of tumescent anesthesia knowing that the energy liberated from laser may be responsible for thrombus formation that may migrate to the deep veins .the platelet activator marker (P selectin) and D-dimer as surgical trauma marker we measured before, during and immediate after laser ablation in blood samples taken from peripheral and femoral venous cannulas. P-selectin values were elevated non stigmatically in both peripheral and femoral veins only after laser ablation of the saphenous vein, while there was no significant difference in its level in samples taken from both veins in the three times of blood sampling. Femoral sample of P-selectin levels mainly reflects heat-induced activation of the most-proximal part of the GSV and the FV area, which are not directly exposed to the laser beam and of surviving islands of endothelium within the treated vein. P-select in is not specific for endothelial cells, but as an activation marker for platelets which is important for thrombus formation [6]. The same results of non-significant rise of P Selectin was observed in peripheral venous samples. Although there was a significant rise of its level in post ablation samples (22&23.2ng/mL) in both peripheral and femoral veins samples in 3 patients 12 %; all of them showed superficial thrombophlebitis after 48 hours and one showed femoral vein thrombosis one week later. This was different from results of Ress, et al. as they did not study those patients who developed VTE separately [7]. Also, we noticed d dimer (activation marker of coagulation and fibrinolysis, supports the diagnosis of DVT). Values were none elevated scientifically in both peripheral and femoral veins during and after laser ablation of the saphenous vein. Also, Probstle et al. reported a D-dimer increase within normal limits during laser ablation [8]. During this study, there was a significant rise of its level in during ablation samples (500 &519ng/mL) which persists in the post ablation sample (555&538 ng/mL) in both peripheral and femoral veins samples in 3 patients 12 %; all of them showed superficial thrombophlebitis after 48 hours and one showed femoral vein thrombosis one week later. This may correlate with clear increase of hemostatic markers above baseline levels during the surgical procedure in highly traumatizing surgery [9]. Therefore, it is worthwhile to consider whether thrombotic complications are due to individual variation for hypercoagulation state of the patient or either inadvertent application errors than the thrombotic burden of the procedure itself.
Conclusion
Pulsed mode laser ablation with an 1040-nm fiber starting 2 cm distal to the SFJ does not induce measurable platelet and endothelium activation in the femoral or systemic blood. Furthermore, the immediate surgical trauma associated with EVLA appears to be modest. Although elevated level of biomarkers in patients who developed VTE could be a warning sign to put these patients on prophylactic anticoagulation method and push us to do further trials on that track.
References
- Piazza G (2014) Varicose veins. Circulation 130: 582-587.
- Hartmann K (2020) Endovenous (minimally invasive) procedures for treatment of varicose veins: The gentle and effective alternative to high ligation and stripping operations. Hautarzt 71: 12-19.
- Mozes G, Kalra M, Carmo M, Swenson L, Gloviczki P (2005) Extension of saphenous thrombus into the femoral vein: A potential complication of new endovenous ablation techniques. J Vasc Surg 41: 130-135.
- Healy DA, Kimura S, Power D, Elhaj A, Abdeldaim Y, et al. (2018) A Systematic Review and Meta-analysis of Thrombotic Events Following Endovenous Thermal Ablation of the Great Saphenous Vein. Eur J Vasc Endovasc Surg 56: 410-424.
- Jacobs CE, Pinzon MM, Orozco J, Hunt PJB, Rivera A, et al. (2014) Deep venous thrombosis after saphenous endovenous radiofrequency ablation: Is it predictable? Ann Vasc Surg 28: 679-685.
- Heere-Ress E, Veensalu M, Wacheck V, Tzaneva S, Kittler H, et al. (2011) Does endovenous laser ablation induce endothelial damage at the saphenofemoral junction? Dermatologic Surg 37: 1456-1463.
- Cambien B, Wagner DD (2004) A new role in hemostasis for the adhesion receptor P-selectin. Trends Mol Med 10: 179-186.
- Proebstle TM, Lehr HA, Kargl A, Espinola-Klein C, Rother W, et al. (2002) Endovenoustreatment of the greater saphenous vein with a 940-nmdiode laser: thrombotic occlusion after endoluminal thermal damage by laser-generated steam bubbles. J Vasc Surg 35: 729-736.
- Aglietti P, Baldini A, Vena LM, Abbate R, Fedi S, et al. (2000) Effect of tourniquetuse on activation of coagulation in total knee replacement. Clin Orthop Relat Res Page no: 169-177.
Citation: Fakhry AM, AbdRahman MA, Nagib SA, Zyada AA (2021) Biochemical Endothelial Injury and Platelets Activation Detectionin Endovenous Laser Ablation of Varicose Veins. J Angiol Vasc Surg 6: 063.
Copyright: © 2021 Ayman M Fakhry, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

