
Bloody Nipple Discharge – A Stressful Presention with a Begnin Cause
*Corresponding Author(s):
Inês Pereira SoaresPaediatrics, Unidade Local De Saúde Estuário Do Tejo – Hospital De Vila Franca De Xira, Portugal
Email:ines_ips93@hotmail.com
Abstract
Bloody nipple discharge (BND) is a rare occurrence in infancy, with mammary duct ectasia being the most common cause. The occurrence of BND can be particularly distressing, for both parents and pediatricians, due to its association with breast carcinoma in adults. We present a case of a 10-month-old girl who exhibited intermittent left-sided BND for a duration of 6 weeks. Coagulation and hormonal tests were within the age-appropriate reference ranges, and ultrasound imaging was normal. The symptoms resolved spontaneously. In such cases, it is crucial to avoid unnecessary invasive procedures or treatments, while providing support to parents and addressing any misconceptions associated with this condition.
Introduction
Physiological milky nipple discharge, whether accompanied by breast enlargement, is commonly seen within the first months of life. This phenomenon, known as breast tissue hypertrophy, is attributed to maternal hormones, transmitted via the placenta, and fetal hormones [1]. In contrast, bloody nipple discharge (BND) is exceedingly rare, with fewer than 30 cases reported in children worldwide [2].
Mammary duct ectasia is recognized as the leading cause of BND in infants, yet the underlying etiologies and mechanisms are not well understood [2]. Possible contributing factors include hormonal and environmental influences, such as inflammation and obstruction, combined with a predisposition to ductal dilation, suggesting a multifactorial and complex pathogenesis [3]. Several reports have documented bacterial infections associated with duct ectasia, nonetheless these occurrences are too inconsistent to be considered a definitive etiological factor [1]. The incidence of ductal ectasia is higher in males, with a male-to-female ratio of 10:4, and it typically appears between 2 months and 13 years [4]. This differs from the female sex predilection reported in the adult population [5]. Other potential causes, such as intraductal papilloma, intraductal cyst, mammary ductal hyperplasia, prolactinoma, inflammatory breast pathologies or gynecomastia, are also considered [2].
Case Report
A 10-month-old girl presented with a 6-week history of intermittent left-sided BND, evidenced by stains on her clothing (Figure 1). The BND was not spontaneous, occurring only upon breast stimulation, particularly after being held. There was no prior history of breast discharge, fever, trauma, manipulation, or maternal drug ingestion during pregnancy or breastfeeding. 
Figure 1: Bloody nipple discharge stain on the clothing
The patient had a history of recurrent urinary tract infections and was on prophylaxis with trimethoprim/sulfamethoxazole. She was exclusively breast-fed until 6 months, with a weight evolution in the 85th percentile. Her head circumference was above the 97th percentile, however followed a parallel growth curve and she exhibited normal neurodevelopment and head ultrasound, consistent with familial macrocephaly. Family history was negative for bleeding diathesis, breast carcinoma, or endocrine disorders.
Physical examination revealed no hypertrophy, masses, or pain on palpation (Figure 2). There were no signs of inflammation or bloody discharge upon areolar pressure. Further physical examination was unremarkable, with normal female genitalia.
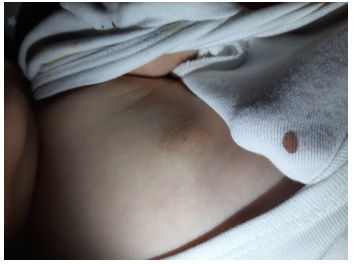 Figure 2: Nipple discharge with no signs of infection or hypertrophy
Figure 2: Nipple discharge with no signs of infection or hypertrophy
Laboratory investigations, including blood cell count and coagulation tests, returned normal results. Hormonal serum levels, including prolactin, oestradiol, thyrotropin, thyroxine, follicle-stimulating hormone, and luteinizing hormone, were within age- appropriate reference ranges. Culture and cytology were not performed due to intermittent discharge (it wasn´t possible to collect a sample). Bilateral breast ultrasonography revealed no abnormalities, with normal breast bud structure, no asymmetries, space-occupying lesions, cysts, or ductal ectasia.
A diagnosis of mammary duct ectasia was assumed, and a watchful waiting approach was adopted. The nipple discharge gradually subsided and resolved spontaneously within 3 months. Follow-up until the age of 36 months was uneventful, with no recurrence of BND.
Discussion
The occurrence of BND can be particularly distressing, for both parents and pediatricians, due to its association with breast carcinoma in adults [3], even though no malignant cases have been reported in patients younger than 3 years [6]. Despite its benign nature, BND often leads to unwarranted diagnostic procedures and treatments [7].
When a child presents with BND, it is crucial to obtain a thorough clinical history, focusing specifically on discharge´s characteristics, birth and feeding details, along with maternal background (2). Benign discharge typically manifests bilaterally and is induced by breast manipulation or stimulation, whereas pathological discharge tends to be unilateral, spontaneous, and persistent [8]. In our case, the BND occurred with stimulation but was unilateral, displaying a combination of features from both benign and pathological types, requiring a precise and cautious approach.
Physical examination is normal in nearly half of the cases of BND [9], as seen in figure 2. Therefore, a structured diagnostic approach should be outlined [8].
The initial workup must include laboratory tests - a complete blood cell count, coagulation tests, hormonal profile, discharge culture and Gram staining and ultrasound of the breast [2].
In this infant the hormonal and coagulation levels were found to be normal and the ultrasound results were unremarkable. Although the most common ultrasound´s finding of mammary duct ectasia is dilation of the retro-areolar mammary ducts, some case reports describe normal results as the mammary duct ectasia is usually mild [6], as evidenced here. It is important to highlight that when the imaging reveals an abnormality other than mammary duct ectasia, it is advisable to seek a consultation with a paediatric surgeon [8].
Cytological findings of BND vary widely, from diffuse foam cells and rare duct epithelial cells to erythrocytes and macrophages. Occasionally macrophages are described as "pigmented macrophages" possibly indicating a response to prior bleeding. Peri-ductal fibrosis, atrophy and the formation of granulation tissue are prevalent findings as well [5]. Despite its limited utility, cytology can help confirm the absence of atypical cells and acute inflammatory processes. By taking this approach, invasive procedures, including biopsies, can be avoided [6].
Children with BND, especially girls, should undergo regular follow-up without immediate interventions since even minor surgical trauma to the breast bud can cause significant tissue damage, leading to functional impairment and lasting disfigurement. Some experts recommend a monitoring period ranging from 6 to 10 months because most reported cases resolve spontaneously within 3-9 months. Nevertheless, certain authors, while advocating for conservative management, also outline specific criteria for surgical consideration. These criteria include suspicious cytological findings, persistent bleeding, enlargement of lesions, presence of pain or tenderness, unilateral BND, palpable masses, abnormal imaging findings, and BND persisting beyond 9 months [9].
Although this BND was unilateral, in infants, both bilateral and unilateral discharge are commonly benign [10], she displayed no other malignant features and the BND resolved spontaneously before 6 months, thus a conservative management was preferred.
This case underscores the significance of recognizing this condition, as meticulous clinical follow-up is safe and minimizes unnecessary diagnostic procedures and invasive treatments.
References
- Fouda EY, Shamrani K, Hamdi A, Jurebi M, Dahlan H, et (2017) Mammary duct ectasia with bloody nipple discharge in a 5-month-old infant: A case report. J Pediatr Surg Case Rep 18:24-26.
- Jung Y, Chung JH (2014) Mammary duct ectasia with bloody nipple discharge in a child. Ann Surg Treat Res 86: 165-167.
- Matamala ÁMA, Biain MA, Ferruz RM, Elfau MTS, García GG (2018) Duct ectasia, an infrequent condition in childhood. A case report. Arch Argent Pediatr 116: E782-E784.
- Gupta S, Goyal A, Mannan N, Bagarhatta M, Mendiratta K (2021) Mammary duct ectasia: an unusual cause of breast enlargment in paediatric age Eurorad.
- Mchoney M, Munro F, MacKinlay G (2011) Mammary duct ectasia in children: Report of a short series and review of the literature. Early Hum Dev 87: 527-530.
- Affranchino PN, Oglietti JP, Amoedo D, Nastri M (2013) Telorragia en el lactante por ectasia ductal. Consideraciones acerca de dos casos. Arch Argent Pediatr 111.
- Nascimento M, Portela A, Espada F, Fonseca M (2012) Bloody nipple discharge in infancy - Report of two cases. BMJ Case Rep.
- Seo JY, Kim SJ, Lee SJ, Song ES, Woo YJ, et al. (2010) Bloody nipple discharge in an infant. Korean J Pediatr 53: 917-920.
- Acer T, Derbent M, Hiçsönmez A (2015) Bloody nipple discharge as a benign, self-limiting disorder in young children: A systematic review including two related case Vol. 50, Journal of Pediatric Surgery. W.B. Saunders 1975-1982.
- Rodrigues CF, Silva N (2022) Bloody nipple discharge in an infant. Journal of Pediatric and Neonatal Individualized Medicine 11.
Citation: Soares IP, Malato MT, Ramos D (2025) Bloody Nipple Discharge – A Stressful Presention with a Begnin Cause. J Neonatol Clin Pediatr 12: 132.
Copyright: © 2025 Inês Pereira Soares, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

