
Case Report on Integrative Cardiology and Acupuncture Treatment for Hypertension and Its Cofactors Such As Daily, Multiple, Long Lasting Vertex and Occipital Migraines/Headaches
*Corresponding Author(s):
Jutta Gassner MSOM, LAcIntegrative Division, The Chambers Center For Well Being, Atlantic Health Care Systems, Morristown, NJ, United States
Tel:+1 9739782357,
Email:jutta.gassner@atlantichealth.org
Abstract
This case report describes the usage of integrative cardiology tools including acupuncture to help mitigate cofactors such as migraines and headaches due to hypertension. The patient suffered from idiopathic hypertension since the age of 16 accompanied with daily, long lasting severe occipital and vertex headaches/migraines. The patient incorporated nutritional recommendations as well as started an exercise and meditation program and received total of (13) acupuncture treatments and was also prescribed a Chinese medicinal herbal formula. After completing 13 acupuncture treatments, the patient had no symptoms of the cofactors (occipital and vertex headaches, irritability and short tempered) related to hypertension. Acupuncture could play a role in treating cofactors related to hypertension.
Keywords
Acupuncture; Hypertension; Integrative cardiology; Migraines; Vertex headaches
INTRODUCTION
Hypertension is the most common problem for primary care visits in the USA. Unfortunately, only 50% of hypertensive patients have the disease under control and continue to suffer with various cofactor related issues [5,6]. The American Heart Association estimated the economic toll from hypertension at $76.7 billion annually to the USA economy [7]. Hypertension increases the risk of heart attacks, stroke and kidney disease [8,9]. It is paramount to have proper disease management tools available in order to prevent subsequent debilitating illnesses resulting from hypertension and its cofactors. According to research, acupuncture could be used as an adjunct in the treatment of hypertension and its cofactors [10].
PRESENTING CONCERNS
CLINICAL FINDINGS
Patient self-referred herself for evaluation of her hypertension and subsequent headaches from an integrative cardiology perspective.
Physical exam showed no abnormalities.
Vital signs: BP 146/108 mm Hg, Temperature 98.8 degree Fahrenheit or 37.1 degree Celcius; BMI 23.83 kg/m2; constitutionally well developed and well nourished; normocephalic; negative for thyromegaly.
Cardiovascular: Patient experiences normal heart rate, regular rhythm, normal heart sounds and intact distal pulses, no heart murmurs heard.
Neurological: Patient is alert and oriented to person, place and time. No cranial nerve deficit, negative for seizures, syncope and facial asymmetry.
Psychiatric: Patient has normal mood and affect; behavior is normal and optimistic outlook on life, very animated but not hyperactive.
Integrative cardiology evaluation resulted in the following recommendation for outpatient treatment:
• Follow up with her regular cardiologist for her usual medical management and micronutrient testing - currently atenolol 50 mg daily oral, nifedipine 30 mg daily oral, Omega fish oil (3S/DHA/EPA/FISH) 1 tablet, Cholecaliferol Vit B12 oral 1 tablet daily, CholecaliferolVit D3 1000 unit chewable daily.
• 3 day doctor’s data stool test to evaluate for dysbiosis
• Urine testing for heavy metal toxicity
• Heart-Math biofeedback sessions
• 30 min of aerobic exercise daily
• Acupuncture
• Pranayama Universal Breathing - APP for iPhone
• Supplements: CoQ10 100 mg daily, Magnesium Citrate 400 mg at bedtime, garlic supplement, Metagenics Cardiogenics Intensive Care
• Foods add to daily regiment: Celery - 4 stalks, garlic - 4 raw cloves, onions - 4 raw slices, wakame, natto and dark chocolate (at least 70 %) 10-30 gm.
DIAGNOSTIC FOCUS AND ASSESSMENT
• Did patient experience any headaches if so?
• What was the frequency of the headaches?
• What was the intensity of the headaches?
• What was the duration of the headaches?
Initially MYMOP (Measure Yourself Medical Outcome Profile) for patient’s assessment was considered but due to time limitations, the above mentioned verbal shortened evaluation was used [11]. Patient’s level of “happiness” and “improved temperament” was not part of the initial treatment goal but was referenced several times as a positive by the patient herself. Also a decrease of neck, back and low back pain was mentioned by patient numerous times but was not part of the initial treatment goal. The treatment goal was to decrease/diminish headaches and migraines.
Please refer to “Timetable A” (Table 1) to see the progression of the migraines/headaches symptoms indicated on a scale 0 - 10. This Timetable A also illustrates the various cardiology appointments and their recommended tests.
| Initial On-Set of symptoms | Initial Visit to Integrative Cardiologist | Subsequent Visits to MD | Cardiology Results |
| 22 years ago | May 20th 2015 to Integrative cardiologist | June 30th 2015; Dec 17th 2015, March 29th 2016. | June 2nd 2015 - Cardio Metabolic Rate test negative; June 19th 2015 Comprehensive Stool Analysis test: No yeast isolated, Lysozyme elevated showing inflammation; Secretory Ig A elevated suggesting up-regulated immune response; June 19th 2015 Heavy metal test results showed non-significant results; all follow-up cardiology evaluations were stable. |
| Initial Visit to TCM practitioner (Traditional Chinese Practitioner, including acupuncture and Chinese herbology) | Subsequent visits to TCM practitioner | TCM Results | |
| Acupuncture treatment only | |||
| May 25th 2015 | June 1st 2015, June 5th 2015, June 11th 2015, June 18th 2015. | Weekly follow-up visits showed a substantial decrease in the frequency, duration & intensity of the headaches; from a scale of 0-10, the intensity decreased from a 6-7/10 down to a 2-3/10; and patient had no headaches on average of 3 consecutive days following the acupuncture treatment. | |
| June 30th 2015; July 10th 2015. |
Patient experienced no headaches at all, scale 0/10 |
||
| July 24th2015 | Two weeks without headaches scale 0/10 | ||
| July 31st 2015 | One week without headache scale 0/10 | ||
| August 21st 15 | Three week follow-up visit, no headache scale 0/10 | ||
| Acupuncture treatment and Chinese herbal formula (was authorized by integrative cardiologist) | |||
| Sep 4th 2015 | No headaches on a scale 0/10; patient received Liu Wei Di Huang Wan prescription 1 gram/day | ||
| Oct 1st 2015 |
Phone consultation with patient and patient reported no headaches only occasional tension and no issues with formula; I advised patient to take formula every other day, 1 gram |
||
| Jan 15th 2016 | Phone consultation with patient and patient reported no headaches only occasional tension and no issues with formula; I advised patient to take formula twice a week, 1 gram | ||
| Feb 11th 2016 | Phone consultation with patient and patient reported no headaches only occasional tension and no issues with formula; I advised patient to take formula twice a day, 1 gram |
The figure 1, “Timeline for Cardiology and Acupuncture Services” shows a visual representation of patient interventions on a consecutive time line such as cardiology and acupuncture visits, acupuncture and herbal phone consultations and the development of the patient’s blood pressure.
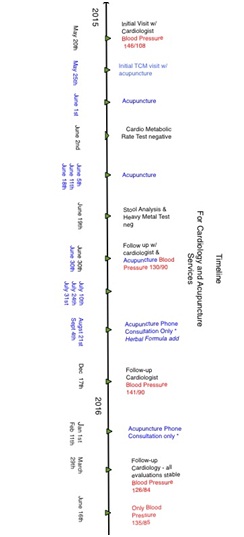
Please refer to the table for “Blood Pressure Development” (Table 2) to see swiftly how the blood pressure improved from the first cardiology visit back in May 2015 to the last follow-up in June 2016.
| Date | Blood Pressure Readings |
| Initial Visit 5/20/15 | 146/108 mmHg |
| 6/30/2015 | 130/90 mmHg |
| 12/17/2015 | 141/90 mmHg |
| 3/29/2016 | 126/84 mmHg |
| 6/16/2016 | 134/85 mmHg |
THERAPEUTIC FOCUS AND ASSESSMENT
Acupuncture treatment
Patient also reported an improvement in her mood aside from being headache free.
Patient also indicated that her lower and middle back and neck are pain free and the back feels looser all together.
Acupuncture had an immediate impact on the headaches as opposed to the dietary changes and nutritional supplements. During the first couple of treatments, patient experienced a headache prior to the acupuncture session. The headaches disappeared during the acupuncture session and patient remained headache free for a couple of hours initially and then days following the acupuncture treatment [12].
Acupuncture treatment was performed in prone position. The traditional Chinese diagnosis was “Kidney yin deficiency with underlying Spleen Qi Deficiency”.
The diagnosis was formulated due to patients’ symptoms such as a slightly V-shaped yet swollen tongue, malar flush in the afternoon and early evening hours, sweating of the palms, vaginal dryness, dry eyes, being bloated after eating, propensity towards flatulence, fatigued, headaches with a sensation of “flutter around the chest” and constipation with loose bowls.
The tongue, as mentioned above is slightly V-shaped, pink/reddish in color, swollen, scalloped on both sides, thick white coating and sublingual veins are negative.
Pulse presented as thin, weak and slightly floating; the chi position is not rooted and hardly felt. Both, the cun and guan positions are present. The overall pulse rate is 82 beats/minute.
Patient was diagnosed by the practitioner, Jutta Gassner.
The following acupuncture points were used: Small Intestine 3, Urinary Bladder 62, 13, 15, 17, 23, Kidney 2 & 7, Gall bladder 20 & 21. Even so patient presented with an underlying Spleen Qi Deficiency, no specific acupuncture points were selected to treat Spleen Qi Deficiency since Kidney Yin Deficiency presented itself so prominently. By nourishing Kidney Yin Deficiency, the patients “traditional” Spleen Qi Deficiency symptoms such as fatigue, constipation with loose bowls and propensity towards flatulence improved.
Needle retention was approximately 30 minutes without stimulation.
De Qi sensation was achieved by most points. De Qi was measured in two ways - one via subjective needle sensation experienced and felt by the practitioner (practitioner felt a slight “pull” by the needle) and the other one via patient feedback; where patient would state “Oh I feel an electric shock”.
Needle size used (0.12) X 30, brand, “Seirin”.
Follow up and Outcomes (Table 2)
| Acupuncture treatment only | |
| June 1st 2015, June 5th 2015, June 11th 2015, June 18th 2015 | Weekly follow-up visits showed a substantial decrease in the frequency, duration & intensity of the headaches; from a scale of 0-10, the intensity decreased from a 6-7/10 down to a 2-3/10; and patient had no headaches on average of 3 consecutive days following the acupuncture treatment |
| June 30th 2015; July 10th 2015 | Patient experienced no headaches at all, scale 0/10 |
| July 24th 2015 | Two weeks without headaches scale 0/10 |
| July 31st 2015 | One week without headache scale 0/10 |
| August 21st 15 | Three week follow-up visit, no headache scale 0/10 |
| Acupuncture treatment and Chinese herbal formula (was authorized by integrative cardiologist) | |
| Sep 4th 2015 | No headaches on a scale 0/10; patient received Liu Wei Di Huang Wan prescription 1 gram/day |
| Oct 1st 2015 | Phone consultation with patient and patient reported no headaches only occasional tension and no issues with formula; I advised patient to take formula every other day, 1 gram |
| Jan 15th 2016 | Phone consultation with patient and patient reported no headaches only occasional tension and no issues with formula; I advised patient to take formula twice a week, 1 gram |
| Feb 11th 2016 | Phone consultation with patient and patient reported no headaches only occasional tension and no issues with formula; I advised patient to take formula twice a day, 1 gram |
The Chinese herbal formula, Liu Wei Di Huang Wan, was prepared by Crane Herb Company, located in Mashpee, MA via pill form.
The ingredients for Liu Wei Di Huang Wan are as followed: Shu Di Huang 9 grams, Shan Zhu 9 grams, Shan Yao 9 grams, Mu Dan Pi 4.5 grams, Fu Ling 6 grams, Ze Xie 3.5 grams, Du Zhong 6 grams.
Initially, the herbal formula was prescribed for 1 gram/day for 2 weeks; then 1 gram every other day for 4 months and finally 1 gram 2 times per week only as maintenance dose as long as the patient was covering for the strike and working these extra long hours.
DISCUSSION
Some research studies show positive effects of acupuncture treatments of hypertensive cofactors such as headaches and or migraines and adding acupuncture to standard care to this patient population, can result in a better quality of life. (Cevik C1, Iseri So 2013). Furthermore, a recent meta-analysis on the effects of acupuncture on blood pressure reduction only without looking at cofactors, showed mixed results. 23 RCT, sampling over 1788 patients showed on two trials a decrease in systolic blood pressure when acupuncture was administered in conjunction with pharmaceuticals. The remaining 21 trials were unclear of bias and the evidence alone for acupuncture lowering blood pressure is insufficient. Nonetheless, acupuncture needs to be further investigated as an adjunct treatment modality for co-factors related to hypertension.
REFERENCES
- Poulter NR, Prabhakaran D, Caulfield M (2015) Hypertension. Lancet 386: 801-812.
- Carretero OA, Oparil S (2000) Essential hypertension. Part I: definition and etiology. Circulation 101: 329-335.
- Burt VL, Cutler JA, Higgins M, Horan MJ, Labarthe D, et al. (1995) Trends in the prevalence, awareness, treatment and control of hypertension in the adult US population: data from the health examination surveys, 1960 to 1991. Hypertension 26: 60-69.
- Ostchega Y, Dillon CF, Hughes JP, Carroll M, Yoon S (2007) Trends in hypertension prevalence, awareness, treatment and control in older US adults: data from the National Health and Nutrition Examination Survey 1988 to 2004. J Am Geriatr Soc 55: 1056-1065.
- Centers for Disease Control and Prevention (2013) High Blood Pressure. Centers for Disease Control and Prevention, Atlanta, GA, USA.
- Frieden T (2012) CDC Director Thomas Frieden Plays ‘Not My Job’. Interview with Thomas Frieden, Director of the Center for Disease Control, USA Today Show, Atlanta, GA, USA.
- Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, et al. (2010) Heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation 121: 46-215.
- Lackland DT, Weber MA (2015) Global burden of cardiovascular disease and stroke: hypertension at the core. Can J Cardiol 31: 569-571.
- Mendis S, Puska P, Norrving B (2011) Global atlas on cardiovascular disease prevention and control. World Heart Federation, World Stroke Organization, World Health Organization, Geneva, Switzerland.
- Cevik C, I?eri SO (2013) The effect of acupuncture on high blood pressure of patients using antihypertensive drugs. Acupunct Electrother Res 38: 1-15.
- Paterson C (1996) Measuring outcomes in primary care: a patient generated measure, MYMOP, compared with the SF-36 health survey. BMJ 312: 1016-1020.
- Zhao XF, Hu HT, Li JS, Shang HC, Zheng HZ, et al. (2015) Is Acupuncture Effective for Hypertension? A Systematic Review and Meta-Analysis. PLoS One 10: 0127019.
Citation: Campanile G, Gassner J (2016) Case Report on Integrative Cardiology and Acupuncture Treatment for Hypertension and Its Cofactors Such As Daily, Multiple, Long Lasting Vertex and Occipital Migraines/Headaches. J Altern Complement Integr Med 2: 015.
Copyright: © 2016 Giovanni Campanile, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

