
Case Report: Post Traumatic Uterine Arteriovenous Fistula Embolization
*Corresponding Author(s):
Carlos Alberto Da Silva Frias NetoDepartment Of Vascular Surgery, Hospital São Domingos, São Luís, Brazil
Tel:+55 981810084,
Email:friasneto@gmail.com
Abstract
Patient developed great amount of vaginal bleeding after curettage to resolve anembryonic pregnancy. Transvaginal ecodoppler and angiotomography shows uterine arteriovenous fistula related to right uterine artery. Angiography confirmed the later exams findings. At the same time as angiography it was made right uterine artery embolization with Onyx. Control angiography shows total fistula occlusion. In clinical evaluation made 16 days after the procedure the patient related no more abnormal bleedings. Periodic exames and clinical evaluations will be made in association with her gynecologist to determine how the lesion evolves and the success in her desire to get pregnant again.
Keywords
INTRODUCTION
Uterine Arteriovenous Malformation (AVM) is a rare cause of vaginal bleeding in women of reproductive age group. Clinically, it has varied presentation, from being completely asymptomatic to various degrees of vaginal bleeding. It can be congenital or acquired [1]. Most AVMs are acquired after damage to uterine tissue, and the majority of reported cases are acquired secondary to dilation and curettage [2,3].
Transvaginal ultrasound is the initial imaging study of choice for abnormal uterine bleeding. The identification of uterine high velocity blood flow with low impedance by Doppler ultrasound is highly suggestive for a uterine AVM. Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) can be helpful to assess the degree of involvement of the surrounding structures [4]. Angiography can determine the location of the lesion, size, blood supply arteries, and drainage veins, as well as reveal the relation between pelvic blood vessels; hence it serves as the gold standard for the diagnosis of uterine arteriovenous malformation. But due to its invasiveness, it is now mainly used to examine the lesion prior to the treatment of uterine artery embolization [5].
Prior to the advent of embolotherapy, hysterectomy was the therapy of choice. Since the first description of a successful embolization treatment for uterine AVM in 1986, embolotherapy has become a well-recognized alternative to surgical intervention for uterine AVMs, with the major advantage of maintaining childbearing capacity [3].
The present case shows an embolization case of an acquired uterine arteriovenous fistula.
CASE REPORT
Thirty-five years old patient, no comorbidities, G2P1, with reproductive intentions, developed vaginal bleeding in great amount after curettage to resolve anembryonic pregnancy (performed 12/21/2017). Transvaginal ecodoppler shows arterial flow in right uterine artery with low resistance, compatible with arteriovenous fistula (Figure 1). Angiotomography confirmed the diagnosis, showing right uterine artery ectasia and early veins filling (Figure 2).
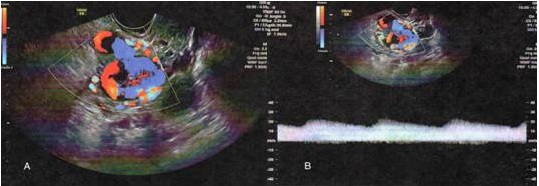 Figure 1: Transvaginal ecodoppler. (A) Color-Doppler showing arteriovenous fistula associated with right uterine artery. (B) Pulsed-wave Doppler showing flow with low distal resistance.
Figure 1: Transvaginal ecodoppler. (A) Color-Doppler showing arteriovenous fistula associated with right uterine artery. (B) Pulsed-wave Doppler showing flow with low distal resistance.
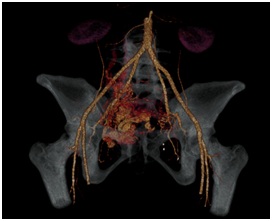 Figure 2: Angiotomography showing arteriovenous fistula associated with right uterine artery.
Figure 2: Angiotomography showing arteriovenous fistula associated with right uterine artery.
Angiography made in 04/04/2018 confirmed the latter exams findings (Figures 2 and 3) and no alterations in left uterine artery. In the same time as angiography it was made right uterine artery embolization with Onyx (Figure 4). Control angiography shows total fistula occlusion (Figure 5).
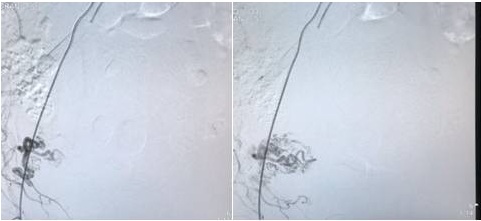 Figure 3: (A) Uterine fistula angiogram in an initial phase. (B) Uterine fistula angiogram in a later phase.
Figure 3: (A) Uterine fistula angiogram in an initial phase. (B) Uterine fistula angiogram in a later phase.
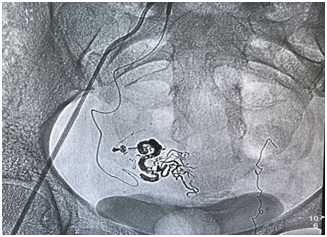 Figure 4: Fistula embolization using Onyx.
Figure 4: Fistula embolization using Onyx.
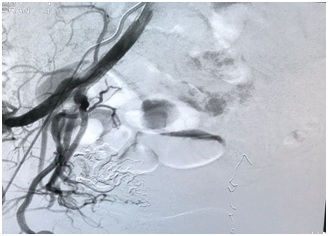 Figure 5: Final angiogram showing successful fistula occlusion.
Figure 5: Final angiogram showing successful fistula occlusion.
Patient referred small amount of vaginal bleeding in the first 24h after the procedure with total resolution within 48h. Referred also low abdominal pain intensity in the first with total resolution within 48h. On clinical evaluation made 16 days after the procedure the patient related no more abnormal bleedings and pain absence.
Periodic exams and clinical evaluations will be made in association with her gynecologist to determine how the lesion evolves and success in her desire to get pregnant again.
DISCUSSION
Fleming et al., in 1989 [6] described, during a period of 10 years, six cases of uterine vascular anomalies, in which four cases were related with uterine curettage. Kwon e Kim in 2002 [7], described 24 cases of uterine vascular anomalies secondary to trauma, in which 21 patients had a history of curettage.
The emergence of these lesions after curettage complications, like uterine perforation, is possible because of the proximity between venous plexus and arcuate arteries and spiral and radial veins and arteries [8].
Recognition of this abnormality as the cause of hemorrhage is important since uterine instrumentation is clearly not indicated and may only worsen the condition. Hysterectomy has traditionally been the treatment of choice, but transcatheter embolization, first reported by Forssman et al., in 1982 and described in a number of single case reports since then, appears to allow successful treatment while sparing uterine childbearing capacity [9]. Other authors report successful pregnancies after uterine arteriovenous malformations embolizations [10-12].
Various embolic agents have been successfully used, including PVA and other particulate embolic agents, liquid embolic agents including n-butyl-cyanoacrylate glue and Onyx (Medtronic), Gelfoam, and coils, and they are often used in combination [13]. Onyx has been used more often when the choice of embolization is a liquid agent (non-adhesive), because it allows prolonged injections and, therefore, better nidus penetration without causing an immediate obliteration of the vessel. On the other hand, it needs longer procedure time, resulting in more radiation, and is more expensive [14].
The present case was treated with Onyx as it brings best control on delivering the substance with lesser risk of non-target embolization. Fistula occlusion was obtained immediately. Patient referred small amount of vaginal bleeding in the first 24h after the procedure, which could have been caused by residual blood or tissue ischemia caused by embolization, but it was resolved within 48h. Pain was not significant and was also resolved in 48h.
CONCLUSION
Endovascular Uterine arteriovenous fistula treatment resulted in total fistula occlusion and successful control of abnormal bleeding. Periodic exams and clinical evaluations will be made in association with her gynecologist to determine how the lesion evolves and success in her desire to get pregnant again.
REFERENCES
- Agarwal N, Chopra S, Aggarwal N, Gorsi U (2017) Congenital uterine arteriovenous malformation presenting as postcoital bleeding: A rare presentation of a rare clinical condition. J Clin Imaging Sci 7: 11.
- Calzolari, S, Cozzolino, M, Castellacci, E, Dubini V, Farruggia, et al. (2017) Hysteroscopic management of uterine arteriovenous malformation. JSLS 21.
- Evans A, Gazaille RE 3rd, McKenzie R, Musser M, Lemming R et al. (2017) Acquired uterine arteriovenous fistula following dilatation and curettage: An uncommon cause of vaginal bleeding. Radiol Case Rep 12: 287-291.
- Yoon D, Jones M, Taani JA, Buhimschi C, Dowell JD (2016) A systematic review of acquired uterine arteriovenous malformations: Pathophysiology, diagnosis, and transcatheter treatment. AJP Rep 6: 6-14.
- Yan X, Zhao C, Tian C, Wen S, He X et al (2017) Ultrasound-guided high-intensity focused ultrasound ablation for treating uterine arteriovenous malformation. BJOG 124: 93-96.
- Fleming H, Ostor AG, Pickel H, Fortune DW (1989) Arteriovenous malformations of the uterus. Obstetrics and Gynecology 73: 209-214.
- Kwon JH, Kim GS (2002) Obstetric iatrogenic arterial injuries of the uterus: Diagnosis with US and treatment with transcatheter arterial embolization. Radiographics 22: 35-46.
- Poli-Neto OB, Neto JBV, Nogueira AA, Reis FJCd (2004) Embolizac?a?o arterial seletiva em fi?stula arteriovenosa uterina po?s-trauma?tica. Radiologia Brasileira 37: 303-305.
- Vogelzang RL, Nemcek AA, Skrtic Z, Gorrell J, Luraln JR (1991) Uterine arteriovenous malformations: Primary treatment with therapeutic embolization. JVIR 2: 517-522.
- Poppe W, Van Assche FA, Wilms G, Favril A, Baert A (1987) Pregnancy after transcatheter embolization of a uterine arteriovenous malformation. Am J Obstet Gynecol 156: 1179-1180.
- Polat P, Suma S, Kantarcy ? M, Alper F, Levent A (2002) Color Doppler US in the evaluation of uterine vascular abnormalities. Radiographics 22: 47-53.
- Chia YN, Yap C, Tan BS (2003) Pregnancy following embolization of uterine arteriovenous malformation-a case report. Ann Acad Med Singapore 32: 658-660.
- Sridhar D, Vogelzang RL (2018) Diagnosis and treatment of uterine and pelvic arteriovenous malformations. Endovascular Today 17: 1-5.
- Woodhams R, Ogasawara G, Ishida K, Fujii K, Yamane T, et al. (2014) Successful treatment of acquired uterine arterial venous malformation using N-butyl-2-cyanoacrylate under balloon occlusion. Acta Radiol Short Rep 3.
Citation: da Silva Frias Neto CA, Felice KP, de Brito Filho SB, Durans MSB (2018) Case Report: Post Traumatic Uterine Arteriovenous Fistula Embolization. J Surg Curr Trend Innov 2: 008.
Copyright: © 2018 Carlos Alberto da Silva Frias Neto, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

