
Case Report: Robotic Assisted Deformity Correction of Grade IV Spondylolisthesis
*Corresponding Author(s):
Alexandra E. ThomsonVirginia Spine Institute, 11800 Sunrise Valley Drive Suite 800 Reston, VA 20191, United States
Tel:+1 7037091114,
Email:athomson@spinemd.com
Abstract
Background
Spondylolisthesis, the anterior translation of a vertebra on another, is a relatively common spinal pathology in adults estimated to occur in 4-8% of the population [1]. Commonly a defect in the pars interarticularis of the lumbar spine reduces posterior stability allowing anterior translation. Spondylolisthesis is further classified by into Grades IV-V based on the percent of anterior translation [2]. High grade spondylolisthesis (Grades VI-V), greater than 50% anterior translation, accounts for 11.3% of cases in the adult population [3]. Most cases in adults regardless of grade are asymptomatic or report vague lower back pain [1,3]. However, if the slip progresses and spino-pelvic balance is altered patients can experience severe pain, significant deformity, and difficulty ambulating [4]. Surgical intervention is necessary when slip progression is imminent or severe neurologic symptoms develop [3]. Surgical treatment in these cases is challenging and requires substantial preoperative planning due to complexity of deformity and loading forces on the lumbar spine. In recent review of the current literature Kunze, et al. found in situ fusion provides adequate fixation with lower incidence of neurologic complications [3]. However, this approach does not correct abnormal sagittal spino-pelvic balance seen in high grade spondylolisthesis. Fusion and reduction restores spino-pelvic balance and permits concurrent wide decompression of adjacent nerve roots without compromising overall construct stability. No single surgical technique has been proven to be consistently superior [5-7]. Robotic assisted spinal surgery offers significant promise in complex cases with improved surgical planning capabilities and operative precision.
Keywords
Grade IV Spondylolisthesis; Robotic Assisted Surgery; Spinal Deformity Correction
CASE PRESENTATION
A 61-year-old female with a 20 year history of chronic low back pain presented with 6 months of worsening lower back pain and bilateral leg pain, 6/10 on visual analog scale with episodes of right leg weakness. For 19 years prior to presentation her symptoms were managed nonoperative treatment including physical therapy and anti-inflammatory medications. Initial weight-bearing radiographs revealed grade IV spondylolisthesis with C7 plumbline 5.6 cm anterior to sacrum and 77.7° of lumbar lordosis (LL). Figure 1 illustrated a loss of sagittal balance with the following pelvic indices: pelvic incidence (PI) of 83.6°, pelvic tilt (PT) of 24.1°, and sacral slope (SS) of 59.5°.
On physical exam she exhibited diffuse tenderness to palpation in bilateral paraspinal muscles, 4/5 strength in bilateral EHL, and difficulty with tandem gait. EMG revealed evidence of mild chronic L5 radiculopathy bilaterally. Given worsening symptomatology and after discussion of risks and benefits patient elected to proceed with surgical intervention.
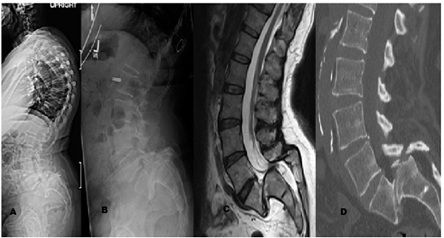 Figure 1: Preoperative Imaging demonstrating grade IV spondylolisthesis at L5 S1. A&B) Lateral upright radiographs of the spine. C) Sagittal T2 weighted MRI of the lumbar spine. D) Sagittal CT of lumbar spine.
Figure 1: Preoperative Imaging demonstrating grade IV spondylolisthesis at L5 S1. A&B) Lateral upright radiographs of the spine. C) Sagittal T2 weighted MRI of the lumbar spine. D) Sagittal CT of lumbar spine.
SURGEON’S RATIONALE
In adults there are multiple techniques for surgical treatment of high grade spondylolisthesis including:
- • Posterior instrumented fusion (PIF) with or without transforaminal lumbar interbody
- • fusion (TLIF) and Gill laminectomy
- • PIF with fibular strut in-situ fusion and Gill laminectomy
- • 360° fusion with TLIF and Gill laminectomy
- • 360° fusion with fibular strut in-situ fusion and Gill laminectomy
- • 360° with L5 corpectomy and PIF with Gill laminectomy [3,5,7]
Due complexity and heterogeneity seen in these deformities no single technique has been proven consistently superior. Panel of 4 spine surgeons reviewed the imaging and collectively decided to precede with anterior lumbar interbody fusion (ALIF) and PIF with Gill laminectomy and sacral dome osteotomy. In this case the L5-S1 level could not be safely accessed from an anterior approach due to degree of deformity and risk to surrounding structure. An ALIF would be performed at L3-L4 and L4-L5 for anterior column support and ensure stability in final construct after posterior decompression and stabilization. The patient’s chronic L5 radiculopathy necessitated wide posterior decompression, and decompression without anterior column support would increase risk of slip progression and fusion failure. Sacral dome osteotomy would provide access to the L5-S1 disc space for bilateral TLIF during the second surgery. PIF from L3-pelvis with robotic guidance would be preformed for deformity correction and posterior column support. The current literature supports the use of reduction and 360° fusion in patients with severe spino-pelvic imbalance, and increased risks of pseudarthrosis over in situ fusion alone [3]. Due to the severity of this case’s spinal imbalance and need for wide decompression necessitated a larger spinal reconstruction over in situ fusion. Multiple studies support the use of in situ fusion as it provides adequate fixation with lower incidence of neurologic complications [1,3,5]. In situ fusion provides the same outcomes with lower complications in lower grade spondylolisthesis [5]. However, in high grade defects particularly those with wide decompression in situ fusion result in a higher risk of pseudarthrosis and slip progression [3]. The implementation of robotic assisted surgery may facilitate improved surgical treatment with augmented surgical planning abilities and increased surgical precision. The Mazor X Stealth™ Edition (Medtronic, Dublin, Ireland) system encompasses three-dimensional preoperative planning software, intraoperative robotic guidance, and intraoperative navigation.
SURGICAL TECHNIQUE
Two-level ALIF was preformed through anterior retroperitoneal approach at L3-4 and L5-S1 with expandable cages adjusted to 14° and 16° of lordosis respectively. After the procedure CT imaging was obtained for preoperative robotic planning of the second stage. The robotic planning software used these CT images to create a detailed model the patient’s specific anatomy.
Robotic planning
The robotic planning interface allowed surgeons to design plans tailored to the specifics of our case’s deformity and simulate deformity correction. Based on these simulations and measurements the final construct instrumentation, incisions, and sacral dome osteotomy were optimized prior to the operation. This is illustrated in Figure 2. Correlated screw trajectories were combined and adjusted to minimize incision size and optimize surgical exposure. In this case the initial angle for L5 pedicle screws was adjusted to reduce distance between the midline open incision and percutaneous incisions. Figure 3 shows the planned, adjusted, and executed surgical incisions based on these trajectories.
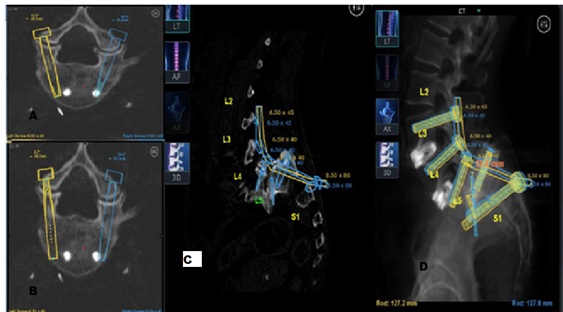 Figure 2: Preoperative planning construct. A&B) Two axial views demonstrate L5 pedicle screw planning. C) Sagittal view of planned osteotomy level and L5-S1 cage placement. D) Illustration of surgical design with 1.2 cm of reduction at L5 to achieve construct.
Figure 2: Preoperative planning construct. A&B) Two axial views demonstrate L5 pedicle screw planning. C) Sagittal view of planned osteotomy level and L5-S1 cage placement. D) Illustration of surgical design with 1.2 cm of reduction at L5 to achieve construct.
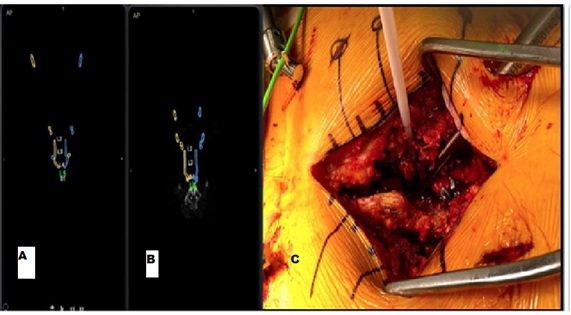 Figure 3: Preoperative Planning for Surgical Incisions. A) Initial skin entry point for screw placement, with L5 screw entry at top of image. B) Plan with adjusted angle for L5 screws, moving entry point closer to others. C) Executed combined open surgical incision with percutaneous L5 screw placement.
Figure 3: Preoperative Planning for Surgical Incisions. A) Initial skin entry point for screw placement, with L5 screw entry at top of image. B) Plan with adjusted angle for L5 screws, moving entry point closer to others. C) Executed combined open surgical incision with percutaneous L5 screw placement.
Second Stage Robotic Procedure
A combined open percutaneous approach was used to minimize over all incision length. Robotic arm was docked, secured to spine with bilateral PSIS Schanz pins, and registered using intraoperative fluoroscopic imaging. Bilateral L3-S2 pedicles were cannulated through robotic arm using drill bit followed by tap and pedicle screw placement. Robotic navigation provided real-time monitoring of screw trajectory, angle, and depth. All pedicle screws w ere stimulated above 15mA on neuromonitoring and AP and lateral imaging confirmed appropriate screw position. The robotic arm was removed for posterior decompression. Complete laminectomy of L3 and L4, medial facetectomy a t L3-4, bilateral foraminotomy of L3, complete Gill laminectomy, central laminectomy at S1, removal of anterior inferior articular facet of L5-S1, removal of superior articular facet of L5-S1, and removal of interior articular facet of L4 were preformed to achieve wide posterior decompression. Sacral dome osteotomy was performed at level designated in the preoperative planning interface to expose the L5-S1 disc space. Figure 4 shows preparation of L5-S1 disc space prior to cage placement. A 22x9x8mm titanium (Titian) cage was placed in the L5-S1 dis c space. Rods were cut and contorted to achieve 50% reduction of L5 with reduction screws. Allograft, autograft, and recombinant human bone morphogenetic protein (rhBMP-2, off-label use) were place in cage. AP, lateral, and O-arm navigation imaging were used to confirm proper location of instrumentation. Allograft and autograft were placed along posterolateral gutters for posterolateral fusion. Procedure was concluded without complication or neuromonitoring changes.
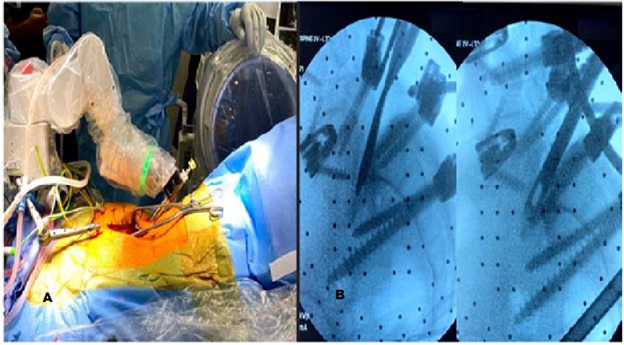 Figure 4: Intraoperative Robotic Assistance. A) Robot docking and operative setup. B) Fluoroscopic radiographs demonstrating preparation of the L5-S1 disc space after sacral dome osteotomy.
Figure 4: Intraoperative Robotic Assistance. A) Robot docking and operative setup. B) Fluoroscopic radiographs demonstrating preparation of the L5-S1 disc space after sacral dome osteotomy.
Postoperative Course
Postoperatively she developed 3/ 5 weakness in left L5 nerve root distribution likely due to neuropraxia. By discharge her preoperative right leg pain completely resolved and her left leg weakness was improving. Postoperative imaging demonstrates bilateral posterior instrumentation of L3 to pelvis with interbody devices at L3-4, L4-5, and L5-S1 without halos or evidence of pseudarthrosis (Figure 5). Lateral radiograph demonstrates improved sagittal balance, grade II spondylolisthesis with 84° LL and the following pelvic indices: PI-83.6°, PT-20.7°, SS-62.9°, and C7 plumbline now falling 3.4 cm anterior to sacrum. At most recent follow up, 3 months post-operative she reports her lower back pain is drastically improved now 4/10 on VAS. Her left L5 distribution weakness is improving and she is progressing well with physical therapy.
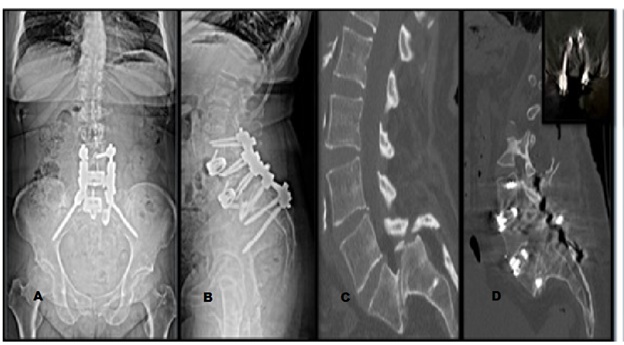 Figure 5: Postoperative Imaging. A & B) AP and lateral views of upright postoperative radiographs demonstrating instrumentation and improved sagittal balance. C & D) Comparison of preoperative and post operative sagittal CT imaging with inset axial view of L5 instrumentation.
Figure 5: Postoperative Imaging. A & B) AP and lateral views of upright postoperative radiographs demonstrating instrumentation and improved sagittal balance. C & D) Comparison of preoperative and post operative sagittal CT imaging with inset axial view of L5 instrumentation.
CONCLUSIONS
The use of peoperative CT and robotic planning, robotic guidance, intraoperative CT navigation, and neuromonitoring allows for precise instrumentation, improved operative efficiency, and improved patient outcomes. Preoperative planning is integral in complex deformity correction of high grade spondylolisthesis. Robotic preoperative planning software provides increased flexibility in surgical design allowing surgeons to make adjustments with simulated deformity correction and considerable flexibility with extensive instrumentation options. A detailed preoperative plan improves intraoperative efficiency; known number, size, and type of instrumentation needed streamlines operation room setup and flow. Robotic assisted surgery combined with comprehensive preoperative planning and intraoperative CT navigation can augment surgical precision and outcomes in complex high grade spondylolisthesis deformity correction.
CONFLICT OF INTEREST/DISCLOSURES
This case report was conducted without external funding sources.
Alexandra E. Thomson- no relevant disclosures, Sam Namian- no relevant disclosures, Christopher R. Good- Medtronic consultant/advisor board member: stock in Mazor Robotics, Ehsan Jazini- no relevant disclosures.
ACKNOWLEDGEMENTS
None.
REFERENCES
- DeWald CJ, Vartabedian JE, Rodts MF, Hammerberg KW (2005) Evaluation and management of high-grade spondylolisthesis in adults. Spine 30(6 Suppl): S49- S59.
- Meyerding HW (1931) Spondylolisthesis. JBJS 13: 39-48.
- Kunze KN, Lilly DT, Khan JM, Louie PK, Ferguson J, et al. (2020) High-Grade Spondylolisthesis in Adults: Current Concepts in Evaluation and Management. International Journal of Spine Surgery 14: 327-340.
- Li Y, Hresko MT (2012) Radiographic analysis of spondylolisthesis and sagittal spinopelvic deformity. J Am Acad Orthop Surg 4: 194-205.
- Noorian S, Sorensen K, Cho W (2018) A systematic review of clinical outcomes in surgical treatment of adult isthmic spondylolisthesis. Spine J 18: 1441–1454.
- Etemadifar MR, Hadi A, Masouleh MF (2016) Posterolateral instrumented fusion with and without transforaminal lumbar interbody fusion for the treatment of adult isthmic spondylolisthesis: A randomized clinical trial with 2-year follow-up. J Craniovertebr Junction Spine 7: 43-49.
- Jones TR, Rao RD (2009) Adult isthmic spondylolisthesis. J Am Acad Orthop Surg 17: 609-617.
Citation: Thomson AE, Namian S, Good CR, Jazini E (2020) Case Report: Robotic Assisted Deformity Correction of Grade IV Spondylolisthesis. Archiv Surg S Educ 2: 011.
Copyright: © 2020 Alexandra E. Thomson, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

