
Case Report: Robotic Multi-Recurrence Inguinoscrotal Hernia IPOM Repair
*Corresponding Author(s):
Jolanta WilczynskaDepartment Of Psychiatry, St. Gallen Nord, Zürcherstrasse 30, 9500 Wil SG, Switzerland
Email:jolanta.wilczynska@hin.ch
Abstract
Background: This is a case report of a four-time recurrent inguinoscrotal hernia on the left side, that was finally successfully operated using robotic daVinci da Xi (Intuitive) intraperitoneal Onlay-Mesh-Plastic (rIPOM) hernia repair technique. To date, robotic IPOM operation procedures are less common in Europe. Therefore, we present our experience with this method for the treatment of a multiple recurrent inguinoscrotal hernia.
Case Presentation: This is a single-institute presentation and report of a challenging case. A 77-year-old man with a large four times recurrent inguinoscrotal hernia was treated using a minimally invasive robotic IPOM technique. The previous hernias repairs were performed during a period of 21 years between 1996 and 2015. In 1996, the initial hernia on the left side was an open transversalis plastic (Barwell). After two years, in 1998 the first recurrence occured and was treated with open mesh plastic (Lichtenstein). Six years later, in 2004 the second recurrence occured and was repaired with open preperitoneal mesh plastics (Rivers-Stoppa). Eleven years later, in 2015 the third hernia recurrence with incarceration of the colon was diagnosed. The hybrid operation mediale laparotomy for colon revision without resection and laparoscopic mesh palstic (TAPP) were performed. The current forth recurrence of the inguinoscrotal hernia appeared after four years in 2019. Its diagnosis was based on the patient’s history and physical examination. The rIPOM repair was performed and almost four years of follow-up showed that the patient was both recurrence and complications free.
Conclusion: The IPOM technique takes less time because intraoperative preparation of the preperitoneal space is not required and because it allows mesh coverage of the entire myopectineal orifice. The robotic approaches, as compared to laparoscopic approaches, provide the opportunity for better three-dimensional visualisation, elimination of surgeon tremors and precise dissection. We suggest the robotic IPOM technique in cases of multi-recurrence inguinoscrotal hernia if other open or minimally invasive hernia surgeries have failed.
Keywords
Inguinoscrotal hernia, Intraperitoneal Onlay-Mesh-Plastic (IPOM); Recurrence, Robotic surgical procedures
Background
This is the first report of a complicated four-time left site recurrent inguinoscrotal hernia that was successfully operated with a modern technique such as the robotic intraperitoneal Onlay-Mesh-Plastic (rIPOM) inguinal hernia repair. Despite the increasing use of the mesh, there is a small reducing effect on the rate of recurrent hernia repairs [1]. The robotic approaches, as compared to laparoscopic approaches, provide the opportunity for better three-dimensional visualisation, elimination of surgeon tremors and precise dissection [2,3]. We recommend the robotic IPOM technique in cases of multi-recurrence inguinoscrotal hernia if other open or minimally invasive hernia surgeries have failed.
Case Presentation
A 77-year-old man with a BMI of 23 kg/m2 presented in our hospital for the first time in 2019 with a symptomatic herination in his left scrotum. Previously, he had four different hernia repairs on the left side in other hospitals (Figure 1) [4]. All operations were performed during a period of 21 years between 1996 and 2015. Each time, a different repair technique was applied and a different well experienced surgeron preformed the operation in a single academic hospital. The primary surgery was an open transversalis plastic modo Barwell with out mesh implantation in 1996. After two years, in 1998 the first recurrence occured and was treated with open mesh Lichtenstein plastic. After six years, in 2004 the second recurrence happend and was treated with open Rivers-Stoppa preperitoneal mesh plastic. Eleven years later, in 2015 the third recurrence with incarceration of the colon was diagnosed. The hybrid operation with mediale laparotomy with colon inspection without resection and Laparoscopic Mesh Palstic (TAPP) were performed. The patient had additionaly the right inguinoscrotal plastic (Lichtenstein) in 1997.
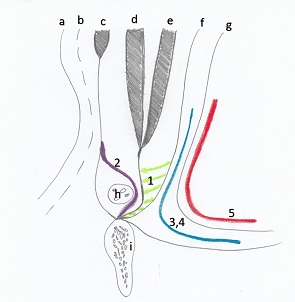 Figure 1: Summery of performed operations [4], a - skin, b -Scarp`s fascia, c - external oblique muscle, d -internal oblique muscle, e - transversus abdominalis muscle, f - fascia transversalis, g - peritoneum, h- spermatic cord, i - os pubis, 1 - primary operation, open tranversalis plastic (Barwell) without mesh (1996), 2 - 1st recurrence, open mesh plastic (Lichtenstein) (1998), 3 - 2nd recurrence, open preperitoneal mesh plastic (Rivers-Stoppa) (2004), 4 - 3rd recurrence, hybrid operation with mediale laparotomy without colon resection and laparoscopic mesh plastic (2015), 5 - 4th recurrence, our robotic intraperitoneal mesh plastic (2019).
Figure 1: Summery of performed operations [4], a - skin, b -Scarp`s fascia, c - external oblique muscle, d -internal oblique muscle, e - transversus abdominalis muscle, f - fascia transversalis, g - peritoneum, h- spermatic cord, i - os pubis, 1 - primary operation, open tranversalis plastic (Barwell) without mesh (1996), 2 - 1st recurrence, open mesh plastic (Lichtenstein) (1998), 3 - 2nd recurrence, open preperitoneal mesh plastic (Rivers-Stoppa) (2004), 4 - 3rd recurrence, hybrid operation with mediale laparotomy without colon resection and laparoscopic mesh plastic (2015), 5 - 4th recurrence, our robotic intraperitoneal mesh plastic (2019).
The current forth recurrence of the inguinoscrotal hernia took place in 2019. Its diagnosis was based on his history and physical examination. The risk factors for actuell recurrence were advanced age of the patient, direct hernia and previous performed ingunal hernia operations. The diagnosis was clinically evident, and no additional sonography or computer tomography was needed. The electiv roboter-assisted laparoscopic transabdominal intraperitoneal mesh repair surgery was performed. The surgeron was well experienced. Operation time was 180 minutes. A presurgical single dose of iv Zinacef 1.5g was given. During the operation, intra-abdominal adhesions, mostly located in the left pelvis, were found. After releasing of adhesions (Figure 2), the hernia sac was found and it contained a large part of the colon (Figure 3). The colon was inspected, no resection was needed and its reposition was performed. A large 4 cm diameter defect, direct inguinoscrotal hernia, R3M in European Society of Hernia (ESH) Classifictation was found (Figure 4). Our defect gap was directly sutured using V-Loc 0 (Medtronic) surgical suture (Figure 5). Bard 3-D Max Light Mesh Extralarge (Bard) at 17.0 x 12.2 cm, was used to cover the defect by attaching a Sorbafix (Bard) to the Lig. Cooperi and the entire myopectinal orifice (Figure 6). Neither we nor prevoius surgerons removed the old mesh.
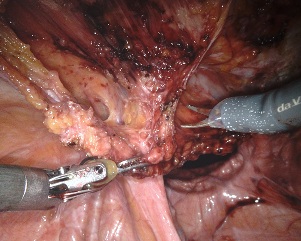 Figure 2: Removing of all adhesions from hernia sac.
Figure 2: Removing of all adhesions from hernia sac.
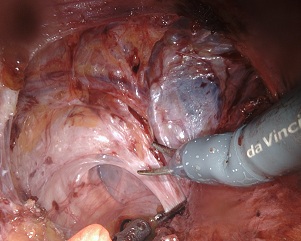 Figure 3: The hernia sac containing a large part of the colon.
Figure 3: The hernia sac containing a large part of the colon.
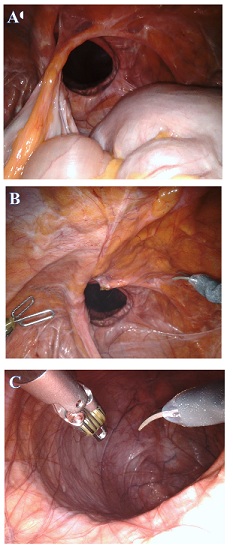 Figure 4: A 4 cm diameter direct inguinal hernia, R3M in ESH Classification in (A), (B) and (C).
Figure 4: A 4 cm diameter direct inguinal hernia, R3M in ESH Classification in (A), (B) and (C).
 Figure 5: Closing an inguinal hernia with a V-Loc 0 (Medtronic) suture.
Figure 5: Closing an inguinal hernia with a V-Loc 0 (Medtronic) suture.
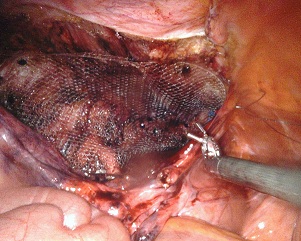 Figure 6: Bard 3-D Max Light Mesh Extralarge (Bard) implantation.
Figure 6: Bard 3-D Max Light Mesh Extralarge (Bard) implantation.
Postoperative complications due to a known Benign Prostata Hyperplasie (BPH) was treated with a single urinary catherisation. There were no futher postoperativ complications after surgical intervention. Almost a 4-year follow-up after our direct rIPOM hernia repair showed that the patient was free of recurrence and complications.
Discussion
Worldwide more than 20 million inguinal hernia repairs are being performed every year [2]. With approximately 13% are recurrent [2,5,6]. The risks for hernia recurrence are multifactoral and some of them are surgical and non-surgical [5]. Surgical risk factors are for example operation method such as minimally invasive one or suture repair [1,4], mesh fixation strategy or surgeon experience [5]. Advanced age, gender, smoking, connective tissue composition, type of admission, previous operations and additional or direct hernia are non-surgical risk factors and can play also an imprtant role in hernia recurrence [5].
Both laparoscopic and robotic hernia repair are often performed in complex inguinal hernias, such as bilateral, recurrent or femoral hernias [2,5,6]. The robotic approach allows the surgeon to identify patients with mixed wall defects such as inguinal, femoral/obturator and contralateral hernias [1,6,7]. It allows for coverage of the entire myopectineal orifice with the mesh [1]. Robotic surgery has better three-dimensional optics and allows for better movement of wristed instruments and a more stable operation [2,3,8]. It also outperforms laparoscopic surgery in tremor correction and precise dissection [3]. Early clinical outcomes showes no significat differences between the robotic and laparoscopic groups in postoperative pain, quality of life, mobility, esthetic outcomes, wound morbidity, and complications [9]. The disadvantages of a robotic approach are longer operation time and increased expense compared to the laparoscopic procedure [6,10,11]. The costs of robotic platforms and instruments are higher [10,12,13]. However, time is a less important factor in this case because IPOM is less time-consuming.
Compared to Europe, in the United States, robotic inguinal hernia repair is a very sophisticated minimally invasive technique for hernia surgery. It is very commonly performed and its use has recently increased exponentially [3,6]. In our opinion in Europe, robotic IPOM technique is performed as the last resort when the prevoius options have failed in cases of multiple recurrent hernias.
Our patient had already been operated on with many different surgical technique. We decided that a robotic IPOM technique would be a beneficial option for him. Our choice of technique has had a significant impact and is a growing popularity of this technique for primary and recurrence inguinal hernia repair in the United States [3,6].
Despite the higher costs, we prefer a robotic IPOM procedure for multi-recurrence inguinal hernia patients, especially when the defect in the abdominal wall is large. The robotic technique provides a better opportunity of recurrence free repair the wall defect because of precise dissection, improved wrist movements as well as much better three-dimensional visualisation [3,8,11]. IPOM technique gave the opportunity to fix posterior abdominal wall defect from an intraabdominal site, which was not tried yet. It also gives the chance to larger mesh size implantation. The study from India showes that the ideal mesh size for open inguinal repair is 9.0 x 15.0 cm, which allows to cover all the potential sites of recurrence [14]. IPOM give us the opportunity to implantate the larger size mesh 17.0 x 12.2 cm. All this above aspects had an impact of our decision to go for rIPOM in this recurrence. We also recommend robotic IPOM hernia surgery, especially if recurrence is difficult to repair.
Comparing robotic versus laparoscopic procedures, the robotic procedure takes significantly longer operation time but has less complications than the laparoscopic group [15]. The common complications of any inguinal hernia surgery technique are recurrence, urinary retention or vascular injuries causing ischaemic orchitis or testicular atrophy [1]. Ingiunodynia and recurrent hernia are more likely to occur in both laparoscopic and robotic hernia repairs than in the open approach [15]. Both laparoscopic and robotic techniques have similar recurrence rates [15]. The readmission rate is without difference.
The indications for prophylactic antibiotic use are skin infection, psoriasis, immune system dysfunction, emergency operation as well as risk of bowel injury [1]. The goal of this prophylaxis is to decrease the risk of surgical site infection and subsequent complications [1]. Approximately 44.4% of general surgeons use preoperative antibiotic prophylaxis [16]. The National Institute of Clinical Excellence (NICE) finds procedures such as mesh implantation as indications for prophylactic antibiotics [17]. The British Hernia Society also gives clear recommendations for high-risk patients, such as those with recurrent hernias [17]. In our department, we prefer zinacef as a prophylactic antibiotic and we performed it.
Conclusion
Both laparoscopic and robotic approach is a significant technique in detecting one of the most common causes of recurrence, such as a preoperative unrecognized hernia, mixed hernias or contralateral inguinal hernias, which are identified for the first time intraoperatively [1,6]. Robotic versus laparoscopic approaches provide the opportunity for better three-dimensional visualization, elimination of surgeon tremors, better wrist movement and precise dissection [2,3,8]. Robotic IPOM technique takes less time because preparation of the preperitoneal space is not required and because it allows for coverage of the entire myopectineal orifice with a mesh. IPOM is worth to try if it was not performed in multi-recurrence case yet despite the most important disadvantage of leaving the prosthetic material within the peritoneal cavity. We recommend the robotic IPOM technique in cases of multi-recurrence inguinoscrotal hernia if other open or other minimally invasive hernia surgeries have failed.
Acknowledgement
Not applicable.
Funding
There was no funding for this study.
Role of the Funding Source
There was no funding for this study.
Conflict of Interest
There is no conflict of interest.
Data availability
Not applicable.
Ethics Approval
Not applicable.
Informed Consent
There is informed consent.
Declaration of Generative AI and AI-Assisted Technologies in the Writing Process
Not applicable.
References
- Peterson-Brown S, Peterson H (2019) Core Topics in General and Emergency Surgery. Edinburgh: Elsevier, Amsterdam, Netherlands.
- Huerta S, Timmerman C, Argo M, Favela J, Pham T, et al. (2019) Open, laparoscopic, and robotic inguinal hernia repair: outcomes and predictors of complications. J Surg Res 241: 119-127.
- Vossler JD, Pavlosky KK, Murayama SM, Moucharite MA, Murayama KM, et al. (2019) Predictors of robotic versus laparoscopic inguinal hernia repair. J Surg Res 241: 247-253.
- Kusia H, Mackiewicza Z (1997) Przepukliny brzuszne. Warszawa: PZWL.
- Burcharth J (2014) The epidemiology and risk factors for recurrence after inguinal hernia surgery. Dan Med J 61: 4846.
- Awad MA, Buzalewski J, Anderson C, Dove JT, Soloski A, et al. (2020) Robotic inguinal hernia repair outcomes: operative time and cost analysis. JSLS 24: 58.
- Jarrard JA, Arroyo MR, Moore BT (2019) Occult contralateral inguinal hernias: what is their true incidence and should they be repaired? Surg Endosc 33: 2456-2458.
- Fitzgibbons RJ, Forse RA (2015) Clinical practice. Groin hernias in adults. N Engl J Med 372: 756-763.
- Prabhu AS, Carbonell A, Hope W, Warren J, Higgins R, et al. (2020) Robotic Inguinal vs Transabdominal laparoscopic Inguinal Hernia Repair. JAMA Surg 155: 380-387.
- Khoraki J, Gomez PP, Mazzini GS, Pessoa BM, Browning MG, et al. (2020) Perioperative outcomes and cost of robotic-assisted versus laparoscopic inguinal hernia repair. Surg Endosc 34: 3496-3507.
- Muysoms F (2021) Robotic abdominal wall surgery: where is its most powerful potential? Cir Esp (Engl Ed). 99: 627-628.
- Charles EJ, Mehaffey JH, Tache-Leon CA, Hallowell PT, Sawyer RG, et al. (2018) Inguinal hernia repair: is there a benefit to using the robot? Surg Endosc 32: 2131-2136.
- Abdelmoaty WF, Dunst CM, Neighorn C, Swanstrom LL, Hammill CW (2019) Robotic-assisted versus laparoscopic unilateral inguinal hernia repair: a comprehensive cost analysis. Surg Endosc 33: 3436-3443.
- Anitha B, Aravindhan K, Sureshkumar S, Bli MS, Vijayakumar C, et al. (2018) The Ideal Size of Mesh for Open Inguinal Hernia Repair: A Morphometric Study in Patients with Inguinal Hernia. Cureus 10: 2573.
- Qabbani A, Aboumarzouk O, ElBakry T, Al-Ansari A, Elakkad MS (2021) Robotic inguinal hernia repair: systematic review and meta-analysis. ANZ J Surg 91: 2277-2287.
- MacCormick AP, Akoh JA (2018) Survey of surgeons regarding prophylactic antibiotic use in inguinal hernia repair. Scand J Surg 107: 208-211.
- Aiken AM, Haddow JB, Symons NR, Kaptanis S, Katz-Summercorn AC, et al. (2013) Use of antibiotic prophylaxis in elective inguinal hernia repair in adults in London and south-east England: a cross-sectional survey. Hernia 17: 657-664.
Citation: Wilczynska J, Gantert W, Nowak A, Nowak P, Kremer M (2023 Case Reports: Robotic Multi-Recurrence Inguinoscrotal Hernia IPOM Repair. J Angiol Vasc Surg 8: 114.
Copyright: © 2023 Jolanta Wilczynska, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

